Abstract
The endothelial barrier controls the passage of solutes from the vascular space. This is achieved through active reorganization of the actin cytoskeleton. A central cytoskeletal protein involved into this is vasodilator-stimulated phosphoprotein (VASP). However, the functional role of endothelial VASP during hypoxia has not been thoroughly elucidated. We determined endothelial VASP expression through real-time PCR (Rt-PCR), immunhistochemistry, and Western blot analysis during hypoxia. VASP promoter studies were performed using a PGL3 firefly luciferase containing plasmid. Following approval by the local authorities, VASP −/− mice and littermate controls were subjected to normobaric hypoxia (8% O2, 92% N2) after intravenous injection of Evans blue dye. In in vitro studies, we found significant VASP repression in human microvascular and human umbilical vein endothelial cells through Rt-PCR, immunhistochemistry, and Western blot analysis. The VASP promoter construct demonstrated significant repression in response to hypoxia, which was abolished when the binding of hypoxia-inducible factor 1 alpha was excluded. Exposure of wild-type (WT) and VASP −/− animals to normobaric hypoxia for 4 h resulted in an increase in Evans blue tissue extravasation that was significantly increased in VASP −/− animals compared to WT controls. In summary, we demonstrate here that endothelial VASP holds significant importance for endothelial barrier properties during hypoxia.
Similar content being viewed by others
INTRODUCTION
The passive and active movement of solutes from the intravascular space to the extracellular compartment is controlled by the endothelial barrier. Central to this process is the cytoskeleton, wherein dynamic reorganization of the actin filaments is crucial for the control of fluid exchange [1]. Vasodilator-stimulated phosphoprotein (VASP) is a central cytoskeletal protein that holds significant impact on the active reorganization of the cytoskeleton. In endothelial cells, VASP functions in membrane ruffling, aggregation, and tethering of actin filaments during the formation of endothelial cell–substrate and cell–cell contacts. Moreover, VASP expression is increased in endothelial cells during angiogenesis and at most phases involving cell shape change [2]. At resting conditions, siRNA-mediated downregulation of VASP does not affect transendothelial resistance (TER) but increases permeability to fluorescein isothiocyanate-conjugated dextran (FITC-dextran) [3, 4]. Similarly, murine microvascular myocardial endothelial (MyEnd) cells derived from VASP −/− mice show no difference in TER when compared to control MyEnd cells but exhibit an increase in permeability to FITC-dextran under resting conditions [5–7].
During periods of hypoxia or inflammation, the endothelial barrier becomes dysfunctional and fluid passes from the intravascular to the extravascular compartment [8]. This process is associated with the formation of stress fibers within endothelial cells [9–11]. VASP prevents the formation of stress fibers and as such is protective for the maintenance of the endothelial barrier function. Furman et al. demonstrated that a reduction of the Ena/VASP expression is detrimental during embryologic development. In this study, the authors demonstrated that in the absence of Ena/VASP, the vasculature exhibits patterning defects and lacks structural integrity, leading to edema, hemorrhaging, and, as a result, late stage embryonic lethality [12]. We have previously demonstrated that VASP is repressed during hypoxia, and this repression results in a reduction of intestinal barrier function during periods of tissue hypoxia in vivo [4]. However, the role of endothelial VASP for the maintenance of barrier function during hypoxia in vivo has not been investigated yet.
In the present study, we pursued the role of VASP for barrier function during hypoxia in vivo. We found a significant repression of endothelial VASP through a hypoxia-inducible factor-1 (HIF-1α)-dependent mechanism which correlated with increased tissue permeability. Studies employing VASP −/− animals identified VASP to be of great importance for vascular barrier function during conditions associated with tissue hypoxia.
MATERIALS AND METHODS
HMEC-1 Cell Line and HUVEC
Human microvascular endothelial cells (HMEC-1) were grown as described previously, and human umbilical cord endothelial cells (HUVEC) were freshly separated according to standard protocols [13].
Transcriptional Analysis
Semiquantitative analysis was performed employing real-time PCR (Rt-PCR, iCycler; Bio-Rad Laboratories, Inc.) to examine VASP expression levels in HMEC-1 after confluent cells were exposed to 4, 12, 24, and 48 h of normobaric hypoxia (2% O2, 98% N2). Primer sets contained 10 pM each of the sense primer 5′-GAA AAC CCC CAA GGA TGA AT-3′ and the antisense primer 5′-GGA AGT GGT CAC CGA AGA AG-3′. The primer set was amplified using increasing numbers of cycles of 94°C for 1 min, 60°C for 2 min, 72°C for 4 min, and a final extension of 72°C for 7 min. Samples were controlled for β-actin using following primers: sense 5′-GGT GGC TTT TAG GAT GGC AAG-3′ and antisense 5′-ACT GGA ACG GTG AAG GTG ACA G-3′ (162 bp). Analysis of expressional levels of vascular endothelial growth factor (VEGF) was performed using sense primer 5′-TTG CCT TGC TGC TCT ACC TC-3′ and antisense 5′-AGC TGC GCT GAT AGA CAT CC-3′.
VASP Protein Analysis
Cell culture samples were normalized for protein levels before applying them in non-reducing conditions to SDS containing polyacrylamide gels. Antibodies used for Western blotting included mouse polyclonal anti-VASP (BD Biosciences). Actin was stained using rabbit anti-actin (Cell Signaling). Detection of HIF-α was performed as described previously (BD Biosciences), and detection of VEGF was performed using murine polyclonal anti-VEGF primary antibody (Santa Cruz). Blots were washed, and species-matched peroxidase-conjugated secondary antibody was added. Labeled bands from washed blots were detected by enhanced chemiluminescence (Amersham Pharmacia Biotech).
Immunofluorescent Staining
HMEC-1 were grown to confluency on acid-washed 12-mm glass cover slips. Cells were then exposed to normobaric hypoxia for 24 h. Cover slips were then washed once in phosphate-buffered saline and fixed for 10 min at room temperature in 1% paraformaldehyde in cacodylate buffer (0.1 M sodium cacodylate; pH 7.4, 0.72% sucrose). The monolayers were permeabilized for 10 min in PBS containing 0.2% Triton X-100 and 3% BSA and VASP protein detected using monoclonal anti-VASP (BD Biosciences) as described previously [4]. Nuclei were counter-stained with 4′,6-diamidino-2-phenylindole (DAPI, 10 μg/ml, Molecular Probes, Eugene, OR). Actin fiber staining was performed using rhodamine-phalloidine (Invitrogen). Confocal laser scanning microscope LSM 510 Meta (Carl Zeiss Jena) was used for imaging.
VASP pGL3 Reporter Assay
Available public databases [14] and analysis of full-length cDNA [GenBank NM_003370] identified the transcription start site of VASP at position −260 relative to the first codon. Analysis of our cloned region of VASP revealed the existence of three potential binding sites for NF-κB and one binding site for HIF-1α (Fig. 4). Truncations of the putative VASP promoter was performed and ligated into a pGL-3 firefly luciferase vector, HMEC-1 transfected, and luciferase activity determined after 24 h exposure to normobaric hypoxia. As a positive control for hypoxia, cells were transfected with a vector-based hypoxia-responsive element (HRE) plasmid containing four tandem HIF-1 enhancer sequences from the 3′-region of the erythropoietin gene.
Quantification of Microvascular Permeability In Vivo
All animal protocols were in accordance with the German guidelines for use of living animals and were approved by the Institutional Animal Care and Use Committee of the Tübingen University Hospital and the Regierungspraesidium Tuebingen. VASP −/− mice and gender-matched C57Bl/6 control mice were bred and genotyped as described previously [15]. Animals were exposed for 4 h to normobaric hypoxia (8%O2, 92%N2). We employed the Evans blue (EB) dye extravasation technique for determination of vascular integrity. EB (20 mg/kg; Sigma-Aldrich) was injected intravenously prior to hypoxia exposure. After animals were sacrificed, EB was extracted as described previously [16]. The absorption of Evans blue was measured at 620 nm and corrected for contamination by heme pigments at 740 nm.
Data Analysis
Data are presented as mean ± SEM. We performed statistical analysis using the Student’s t test or ANOVA to determine group differences. A value of p < 0.05 was considered statistically significant.
RESULTS
Endothelial VASP Is Repressed During Hypoxia
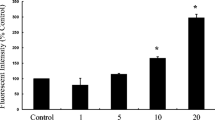
We initially performed transcriptional analysis of VASP expression in endothelial cells during normobaric hypoxia. Following exposure of confluent endothelial HMEC-1 to hypoxia for up to 48 h, we found endothelial VASP expression to be significantly repressed in a time-dependent fashion (Fig. 1a). To control for appropriate hypoxia exposure, we evaluated the expression of vascular endothelial growth factor and found a robust induction of VEGF within these cells confirming adequate exposure to hypoxia (Fig. 1b).
Next, we performed Western blot analysis of two lines of endothelial cells, HMEC-1 and freshly isolated HUVEC. We exposed these cells to 24 h of hypoxia and found a significant repression of VASP levels within both cell types. To confirm hypoxia exposure, we performed analysis of VEGF expression and the expression of HIF-1α. This clearly demonstrated that HIF-1α was significantly induced within these cells (Fig. 2). To gain further proof about the hypoxia-induced repression of VASP, we performed immunohistochemical staining of both endothelial cell lines and found a reduction of VASP immunofluorescence in endothelial cells following exposure to normobaric hypoxia for 24 h (Fig. 3).
VASP Promoter Is Repressed Through HIF-1α During Hypoxia
We performed truncations of the VASP promoter to subsequently exclude the binding sites for NF-κB and HIF-1α. Using these promoter constructs, we found a significant repression of VASP luciferase activity in HMEC-1 in response to hypoxia (Fig. 4a). When excluding the first of three binding sites for NF-κB (construct 1, Fig. 4b) we still observed the previously identified repression. Following exclusion of the HIF-1α binding site through truncation (construct 2, Fig. 4c), we found an attenuation of this repression, demonstrating complete loss of the previously observed repression. Further exclusion of the following two binding sites for NF-κB (constructs 3 and 4, Fig. 4d, e) did not attenuate VASP promoter luciferase activity.
VASP promoter analysis during hypoxia in vitro. Schematic drawing of the putative VASP promoter. Displayed are the potential binding sequences for HIF-1α and NF-κB (green). Serial truncations were then performed relative to transcription start site (TSS) to identify the influence of HIF-1α or NF-κB on the putative VASP promoter HMEC-1 were transfected with the a VASP-PGL3 plasmid, b construct 1 excluding NF-κB binding site 1, c construct 2 excluding the HIF-1α binding site, d construct 3, e construct 4, and f HRE luciferase reporter driven by four tandem HREs (positive control) (Data are mean ± SEM, n = 5, * p < 0.05 as indicated).
VASP −/− Mice Demonstrate Reduced Barrier Properties During Hypoxia
We next sought to investigate whether the in vitro findings of reduced VASP expression during hypoxia would have a functional correlate in vivo. For this, we employed a model of normobaric hypoxia exposing wild-type (WT) mice and mice with gene-targeted repression of VASP (VASP −/−) for 4 h to normoxia or hypoxia following injection with EB dye. After harvesting several organs, we found that during normoxia, WT and VASP −/− animals did not demonstrate significant differences of EB tissue extravasation (Fig. 5a). Following hypoxia exposure, VASP −/− mice demonstrated significantly increased EB tissue extravasation compared to the WT animals (Fig. 5b). Changes in overall vascular leakage between WT and VASP−/− mice under hypoxic conditions were also evident in open abdominal images taken at necropsy (Fig. 5c). These findings identify VASP as a critical control point for permeability changes associated during hypoxia.
Increased vascular permeability in VASP −/− animals during hypoxia. WT and VASP −/− animals were injected with Evan blue dye and exposed to room air or normobaric hypoxia (8% O2, 92% N2) for 4 h. Animals were killed and the lung (Lu), liver (Li), spleen (Sp), kidney (Ki), and colon (Co) were harvested. Organ specific Evans blue concentrations were quantified and corrected for contamination by heme pigments at 740 nm. a Evans blue tissue extravasation in WT and VASP −/− animals following exposure for 4 h to normoxia. b Evans blue tissue extravasation in WT and VASP −/− animals following exposure for 4 h to hypoxia. c Representative images of abdominal dissections of WT and VASP−/− animals following exposure to normoxia or hypoxia for 4 h are demonstrated (All data are mean ± SEM, n = 8–9 per group, *p < 0.05 as indicated).
DISCUSSION
Given the importance of VASP for the endothelial cytoskeleton, the repression of VASP might have functional impact on the endothelial barrier function in vivo. In the presented study, we found a significant repression VASP in endothelial cells during hypoxia which was associated with altered barrier properties during hypoxia in vitro and in vivo as demonstrated through the exposure of VASP −/− mice to hypoxia.
VASP mediates actin dynamics within endothelial and epithelial cells and is involved in cell shape change [2]. In addition, passive cell retraction as a result of cytoskeletal rearrangement plays a key role in mediating cellular contractile response and changes paracellular permeability [17–21]. This rearrangement transposes its force on cell–cell junctions through indirect attachment of actin fibers with tight and adherens junctions. Previous reports have shown that VASP may protect the endothelial barrier during exposure to H2O2 or lipopolysaccharide (LPS) through a prevention of stress fiber formation. In endothelial cells, this stress fiber formation or destruction of cytoskeletal structures is associated with an increase in permeability [22–24]. Downregulation of VASP using VASP siRNA techniques in human pulmonary artery endothelium exacerbates the H2O2-induced decrease in TER, whereas in human lung microvascular ECs, it potentiated LPS-induced decrease in TER [3, 25]. Thus, VASP appears to be a common downstream target for oxidants and inflammatory mediators increasing vascular permeability. A redistribution of actin in cells exposed to chemical hypoxia persists longer than 3 h and is also associated with increased paracellular flux [8, 26]. In addition, ischemia, or as such hypoxia, is a cause for cells to lose their polarity, to open tight junctions, and, as a result, to increase paracellular permeability [27]. We have demonstrated previously that VASP is repressed in response to inflammatory cytokines in endothelial cells and epithelial cells [28]. The presented study extends these findings and identifies HIF-1α to be responsible for the observed repression. An involvement of NF-κB, which is also induced during periods of tissue hypoxia, in the observed VASP repression during periods of hypoxia seems rather unlikely given the results of this study [29]. The possible interaction between hypoxia and inflammation through the IκB kinase complex, a regulatory component of NF-κB, and in the regulation of HIF-1α transcription by NF-κB before and during inflammation, however, has to be kept in mind [8, 29, 30].
Sites of acute inflammation are characterized by shifts in the supply and demand of metabolites that result in limited oxygen availability (inflammation-associated hypoxia) [8, 31, 32]. But hypoxia itself represents an inflammatory stimulus [8, 33–35]. Just as hypoxia can induce inflammation, inflamed lesions often become severely hypoxic [8]. Moreover, exposure of mice to ambient hypoxia (e.g., 8% oxygen over 4–8 h) induces increased leakage through epithelial or endothelial barriers and induces inflammatory cell accumulation in mucosal organs. This plays a critical role in several human clinical conditions including solid organ transplantation (e.g., lung or liver) [36–41]. Although protective pathways are triggered during periods of tissue hypoxia, the effect of these potential pathways on vascular leakage during conditions of VASP repression has to be seen critical [42]. This highlights the fact that VASP is protective for barrier properties in vivo. This was also demonstrated by Furman et al. evaluating the edema formation of mice with gene-targeted deletion of the Ena/VASP complex [12]. This study demonstrated that during embryonic development, Ena/VASP repression resulted in reduced vascular barrier properties and in tissue edema formation [12]. We have demonstrated that VASP deficiency does not alter barrier properties at baseline but results in a significant difference during an acute inflammatory response within the lung [28, 42]. Profirovic et al. extended these findings demonstrating increased vascular permeability in response to thrombin in VASP −/− deficient lungs [43]. We now demonstrate that VASP −/− animals do not demonstrate a difference in vascular permeability at baseline but have increased vascular permeability during a hypoxic challenge. Therefore, our findings are in accordance with previous in vivo reports and further the knowledge about the role of VASP for barrier protection.
In summary, we demonstrate that endothelial VASP has significant impact on vascular barrier function during periods of hypoxia in vivo but does not influence baseline fluid exchange. The results of this and other studies related to the role of VASP in endothelial barrier function during hypoxia may be helpful for development of efficient pharmacological treatment of conditions associated with hypoxia and vascular leak.
REFERENCES
Comerford, K.M., D.W. Lawrence, K. Synnestvedt, B.P. Levi, and S.P. Colgan. 2002. Role of vasodilator-stimulated phosphoprotein in protein kinase A-induced changes in endothelial junctional permeability. FASEB J 16: 583–585.
Price, C.J., and N.P. Brindle. 2000. Vasodilator-stimulated phosphoprotein is involved in stress-fiber and membrane ruffle formation in endothelial cells. Arterioscler Thromb Vasc Biol 20: 2051–2056.
Rentsendorj, O., T. Mirzapoiazova, D. Adyshev, L.E. Servinsky, T. Renne, A.D. Verin, et al. 2008. Role of vasodilator-stimulated phosphoprotein in cGMP-mediated protection of human pulmonary artery endothelial barrier function. Am J Physiol Lung Cell Mol Physiol 294: L686–L697.
Rosenberger, P., J. Khoury, T. Kong, T. Weissmuller, A.M. Robinson, and S.P. Colgan. 2007. Identification of vasodilator-stimulated phosphoprotein (VASP) as an HIF-regulated tissue permeability factor during hypoxia. FASEB J 10: 2613–2621.
Schlegel, N., and J. Waschke. 2009. VASP is involved in cAMP-mediated Rac 1 activation in microvascular endothelial cells. Am J Physiol Cell Physiol 296: C453–C462.
Schlegel, N., S. Burger, N. Golenhofen, U. Walter, D. Drenckhahn, and J. Waschke. 2008. The role of VASP in regulation of cAMP- and Rac 1-mediated endothelial barrier stabilization. Am J Physiol Cell Physiol 294: C178–C188.
Schlegel, N., and J. Waschke. 2009. Impaired integrin-mediated adhesion contributes to reduced barrier properties in VASP-deficient microvascular endothelium. J Cell Physiol 220: 357–366.
Eltzschig, H.K., and P. Carmeliet. 2011. Hypoxia and inflammation. N Engl J Med 364: 656–665.
Wojciak-Stothard, B., L.Y. Tsang, and S.G. Haworth. 2005. Rac and Rho play opposing roles in the regulation of hypoxia/reoxygenation-induced permeability changes in pulmonary artery endothelial cells. Am J Physiol Lung Cell Mol Physiol 288: L749–L760.
Wojciak-Stothard, B., L.Y. Tsang, E. Paleolog, S.M. Hall, and S.G. Haworth. 2006. Rac1 and RhoA as regulators of endothelial phenotype and barrier function in hypoxia-induced neonatal pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 290: L1173–L1182.
Kayyali, U.S., C.M. Pennella, C. Trujillo, O. Villa, M. Gaestel, and P.M. Hassoun. 2002. Cytoskeletal changes in hypoxic pulmonary endothelial cells are dependent on MAPK-activated protein kinase MK2. J Biol Chem 277: 42596–42602.
Furman, C., A.L. Sieminski, A.V. Kwiatkowski, D.A. Rubinson, E. Vasile, R.T. Bronson, et al. 2007. Ena/VASP is required for endothelial barrier function in vivo. J Cell Biol 179: 761–775.
Eltzschig, H.K., M. Faigle, S. Knapp, J. Karhausen, J. Ibla, P. Rosenberger, et al. 2006. Endothelial catabolism of extracellular adenosine during hypoxia: the role of surface adenosine deaminase and CD26. Blood 108: 1602–1610.
Yamashita, R., Y. Suzuki, H. Wakaguri, K. Tsuitani, K. Nakai, and S. Sugano. 2006. DBTSS: DataBase of Human Transcription Start Sites, progress report 2007. Large-scale collection and characterization of promoters of human and mouse genes 5′-end SAGE for the analysis of transcriptional start sites. Nucleic Acids Res 34: D86–D89.
Hohenstein, B., L. Kasperek, D.J. Kobelt, C. Daniel, S. Gambaryan, T. Renne, et al. 2005. Vasodilator-stimulated phosphoprotein-deficient mice demonstrate increased platelet activation but improved renal endothelial preservation and regeneration in passive nephrotoxic nephritis. J Am Soc Nephrol 16: 986–996.
Barone, G.W., P.C. Farley, J.M. Conerly, T.L. Flanagan, and I.L. Kron. 1989. Morphological and functional techniques for assessing endothelial integrity: the use of Evans blue dye, silver stains, and endothelial derived relaxing factor. J Card Surg 4: 140–148.
Hu, R.J., and V. Bennett. 1991. In vitro proteolysis of brain spectrin by calpain I inhibits association of spectrin with ankyrin-independent membrane binding site(s). J Biol Chem 266: 18200–18205.
Lee, A., J.S. Morrow, and V.M. Fowler. 2001. Caspase remodeling of the spectrin membrane skeleton during lens development and aging. J Biol Chem 276: 20735–20742.
Roberts-Lewis, J.M., and R. Siman. 1993. Spectrin proteolysis in the hippocampus: a biochemical marker for neuronal injury and neuroprotection. Ann NY Acad Sci 679: 78–86.
Garcia, J.G., A.D. Verin, and K.L. Schaphorst. 1996. Regulation of thrombin-mediated endothelial cell contraction and permeability. Semin Thromb Hemost 22: 309–315.
Kolodney, M.S., and R.B. Wysolmerski. 1992. Isometric contraction by fibroblasts and endothelial cells in tissue culture: a quantitative study. J Cell Biol 117: 73–82.
Garcia, J.G., A. Siflinger-Birnboim, R. Bizios, P.J. Del Vecchio, J.W. Fenton 2nd, and A.B. Malik. 1986. Thrombin-induced increase in albumin permeability across the endothelium. J Cell Physiol 128: 96–104.
Wu, N.Z., and A.L. Baldwin. 1992. Transient venular permeability increase and endothelial gap formation induced by histamine. Am J Physiol 262: H1238–H1247.
Bouvry, D., C. Planes, L. Malbert-Colas, V. Escabasse, and C. Clerici. 2006. Hypoxia-induced cytoskeleton disruption in alveolar epithelial cells. Am J Respir Cell Mol Biol 35: 519–527.
Bogatcheva, N.V., and A.D. Verin. 2008. The role of cytoskeleton in the regulation of vascular endothelial barrier function. Microvasc Res 76: 202–207.
Kwon, O., C.L. Phillips, and B.A. Molitoris. 2002. Ischemia induces alterations in actin filaments in renal vascular smooth muscle cells. Am J Physiol Renal Physiol 282: F1012–F1019.
Molitoris, B.A. 1991. Ischemia-induced loss of epithelial polarity: potential role of the actin cytoskeleton. Am J Physiol 260: F769–F778.
Henes, J., M.A. Schmit, J.C. Morote-Garcia, V. Mirakaj, D. Kohler, L. Glover, et al. 2009. Inflammation-associated repression of vasodilator-stimulated phosphoprotein (VASP) reduces alveolar-capillary barrier function during acute lung injury. FASEB J 23: 4244–4255.
Rius, J., M. Guma, C. Schachtrup, K. Akassoglou, A.S. Zinkernagel, V. Nizet, et al. 2008. NF-kappaB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1alpha. Nature 453: 807–811.
Bonello, S., C. Zahringer, R.S. BelAiba, T. Djordjevic, J. Hess, C. Michiels, et al. 2007. Reactive oxygen species activate the HIF-1alpha promoter via a functional NFkappaB site. Arterioscler Thromb Vasc Biol 27: 755–761.
Sitkovsky, M., and D. Lukashev. 2005. Regulation of immune cells by local-tissue oxygen tension: HIF1 alpha and adenosine receptors. Nat Rev Immunol 5: 712–721.
Sitkovsky, M.V., D. Lukashev, S. Apasov, H. Kojima, M. Koshiba, C. Caldwell, et al. 2004. Physiological control of immune response and inflammatory tissue damage by hypoxia-inducible factors and adenosine A2A receptors. Annu Rev Immunol 22: 657–682.
Cummins, E.P., E. Berra, K.M. Comerford, A. Ginouves, K.T. Fitzgerald, F. Seeballuck, et al. 2006. Prolyl hydroxylase-1 negatively regulates IkappaB kinase-beta, giving insight into hypoxia-induced NFkappaB activity. Proc Natl Acad Sci USA 103: 18154–18159.
Walmsley, S.R., C. Print, N. Farahi, C. Peyssonnaux, R.S. Johnson, T. Cramer, et al. 2005. Hypoxia-induced neutrophil survival is mediated by HIF-1{alpha}-dependent NF-{kappa}B activity. J Exp Med 201: 105–115.
Rius, J., M. Guma, C. Schachtrup, K. Akassoglou, A.S. Zinkernagel, V. Nizet, et al. 2008. NF-kappaB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1alpha. Nature 53(7196): 807–811.
Eckle, T., M. Faigle, A. Grenz, S. Laucher, L.F. Thompson, and H.K. Eltzschig. 2008. A2B adenosine receptor dampens hypoxia-induced vascular leak. Blood 111: 2024–2035.
Eltzschig, H.K., P. Abdulla, E. Hoffman, K.E. Hamilton, D. Daniels, C. Schonfeld, et al. 2005. HIF-1-dependent repression of equilibrative nucleoside transporter (ENT) in hypoxia. J Exp Med 202: 1493–1505.
Eltzschig, H.K., J.C. Ibla, G.T. Furuta, M.O. Leonard, K.A. Jacobson, K. Enjyoji, et al. 2003. Coordinated adenine nucleotide phosphohydrolysis and nucleoside signaling in posthypoxic endothelium: role of ectonucleotidases and adenosine A2B receptors. J Exp Med 198: 783–796.
Eltzschig, H.K., L.F. Thompson, J. Karhausen, R.J. Cotta, J.C. Ibla, S.C. Robson, et al. 2004. Endogenous adenosine produced during hypoxia attenuates neutrophil accumulation: coordination by extracellular nucleotide metabolism. Blood 104: 3986–3992.
Morote-Garcia, J.C., P. Rosenberger, J. Kuhlicke, and H.K. Eltzschig. 2008. HIF-1-dependent repression of adenosine kinase attenuates hypoxia-induced vascular leak. Blood 111: 5571–5580.
Synnestvedt, K., G.T. Furuta, K.M. Comerford, N. Louis, J. Karhausen, H.K. Eltzschig, et al. 2002. Ecto-5′-nucleotidase (CD73) regulation by hypoxia-inducible factor-1 mediates permeability changes in intestinal epithelia. J Clin Invest 110: 993–1002.
Rosenberger, P., J.M. Schwab, V. Mirakaj, E. Masekowsky, A. Mager, J.C. Morote-Garcia, et al. 2009. Hypoxia-inducible factor-dependent induction of netrin-1 dampens inflammation caused by hypoxia. Nat Immunol 10: 195–202.
Profirovic, J., J. Han, A.V. Andreeva, R.F. Neamu, S. Pavlovic, S.M. Vogel, et al. 2011. Vasodilator-stimulated phosphoprotein deficiency potentiates PAR-1-induced increase in endothelial permeability in mouse lungs. J Cell Physiol 226: 1255–1264.
ACKNOWLEDGMENTS
We thank Alice Mager, Michaela Hoch-Gutbrot, and Stefanie Laucher for technical assistance. This work was supported by a grant from the Fonds National de la Recherche (FNR) to M.A.S. and a grant from the Deutsche Forschungsgemeinschaft (DFG) DFG-RO 3671/4-1 to P.R.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Schmit, M.A., Mirakaj, V., Stangassinger, M. et al. Vasodilator Phosphostimulated Protein (VASP) Protects Endothelial Barrier Function During Hypoxia. Inflammation 35, 566–573 (2012). https://doi.org/10.1007/s10753-011-9347-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-011-9347-z