Abstract
Background
Lumbar disc prolapse is one of the common causes of low back pain seen in the working population13. There are contradictorty reports regarding the clinical significance of various magnetic resonance imaging (MRI) findings observed in these patients. The study was conducted to correlate the abnormalities observed on MRI and clinical features of lumbar disc prolapse.
Materials and Methods
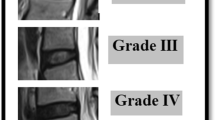
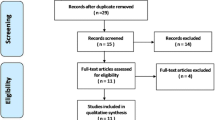
119 clinically diagnosed patients with lumbar disc prolapse were included in the study. Clinical evaluation included pain distribution, neurological symptoms and signs. MR evaluation included grades of disc degeneration, type of herniation, neural foramen compromise, nerve root compression, and miscellaneous findings. These MRI findings were tested for inter- and intraobserver variability. The MRI findings were then correlated with clinical symptoms and the level of disc prolapse as well as neurological signs and symptoms. Statistical analysis included the Kappa coefficient, Odd’s ratio, and logistic regression analysis.
Results
There were no significant inter-or intraobserver variations for most of MRI findings (Kappa value more than 0.5) except for type of disc herniation which showed a interobserver variation of 0.46 (Kappa value). The clinical level of pain distribution correlated well with the MRI level (Kappa 0.8), but not all disc bulges produced symptoms. Central bulges and disc protrusions with thecal sac compression were mostly asymptomatic, while centrolateral protrusions and extrusions with neural foramen compromise correlated well with the dermatomal distribution of pain. Root compression observed in MRI did not produce neurological symptoms or deficits in all patients but when deficits were present, they correlated well with the presence of root compression in MRI. Multiple level disc herniations with foramen compromise were strongly associated with the presence of neurological signs.
Conclusions
The presence of centrolateral protrusion or extrusion with gross foramen compromise correlates with clinical signs and symptoms very well, while central bulges and disc protrusions correlate poorly with clinical signs and symptoms. The presence of neural foramen compromise is more important in determining the clinical signs and symptoms while type of disc herniation (bulge, protrusion, or extrusion) correlates poorly with clinical signs and symptoms.
Similar content being viewed by others
References
Postacchini F. Management of herniation of lumbar disc. J Bone Joint Surg Br 1999;81:567–76.
Vroomen PC, de Krom MC, Wilmink JT. Pathoanatomy of clinical findings in patients with sciatica: A magnetic resonance imaging study. J Neurosurg Spine 2000;92:135–41.
Borenstein DG, O’Mara JW Jr, Boden SD, Lauerman WC, Jacobson A, Platenberg C, et al. The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: A seven-year follow-up study. J Bone Joint Surg Am 2001;83:1306–11.
Ito M, Incorvaia KM, Yu SF, Fredrickson BE, Yuan HA, Rosenbaum AE. Predictive signs of discogenic lumbar pain on magnetic resonance imaging with discography correlation. Spine (Phila Pa 1976) 1998;23:1252–8; discussion 1259-60.
Milette PC, Fontaine S, Lepanto L, Cardinal E, Breton G. Differentiating lumbar disc protrusions, disc bulges, and discs with normal contour but abnormal signal intensity: Magnetic resonance imaging with discographic correlations. Spine (Phila Pa 1976) 1999;24:44–53.
Elfering A, Semmer N, Birkhofer D, Zanetti M, Hodler J, Boos N. Risk factors for lumbar disc degeneration: A 5-year prospective MRI study in asymptomatic individuals. Spine (Phila Pa 1976) 2002;27:125–34.
Weisel SW. Surgical indications and technique. The lumbar spine (Text book), p. 494, Vol 1.
Beattie PF, Meyers SP, Stratford P, Millard RW, Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine (Phila Pa 1976) 2000;25:819–28.
Rankine JJ, Fortune DG, Hutchinson CE, Hughes DG, Main CJ. Pain drawings in the assessment of nerve root compression: A comparative study with lumbar spine magnetic resonance imaging. Spine (Phila Pa 1976) 1998;23:1668–76.
Wong DA. Transfeldt, Ensor Macnab’s Backache. 4th ed. Chapter No. 9. Lippincott Williams & Wilkins; 2007. p. 157.
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001;26:1873–8.
Dora C, Schmid MR, Elfering A, Zanetti M, Hodler J, Boos N. Lumbar disk herniation: Do MR imaging findings predict recurrence after surgical diskectomy? Radiology 2005;235:562–7.
Carragee EJ, Kim DH. A prospective analysis of magnetic resonance imaging findings in patients with sciatica and lumbar disc herniation: Correlation of outcomes with disc fragment and canal morphology. Spine (Phila Pa 1976) 1997;22:1650–60.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Janardhana, A.P., Rajagopal, Rao, S. et al. Correlation between clinical features and magnetic resonance imaging findings in lumbar disc prolapse. IJOO 44, 263–269 (2010). https://doi.org/10.4103/0019-5413.65148
Published:
Issue Date:
DOI: https://doi.org/10.4103/0019-5413.65148