Abstract
Objective
To determine the cost utility of treating schizophrenic patients with olanzapine compared with other antipsychotics in a naturalistic outpatient setting.
Methods
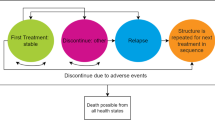
The pan-European SOHO study is a 3-year, prospective, outpatient, observational study of outcomes associated with antipsychotic treatment, focusing on olanzapine, in ten European countries. For the cost-utility analysis, healthcare resource use (inpatient care, day care, outpatient psychiatric consultations and antipsychotic and concomitant medication use) and EQ-5D data were collected at baseline and at 3, 6 and 12 months. The perspective was that of the health service payer. UK healthcare unit costs (year 2004 values) were applied to the resource use data for the ten countries. UK population tariffs were applied to the EQ-5D data to determine utility values.
An Epoch analysis was used to analyze the longitudinal data. Multivariate regression analyses that adjusted for baseline covariates were used to estimate the incremental cost and utility gains for patients treated with olanzapine compared with each of the other antipsychotics (risperidone, quetiapine, amisulpride, clozapine and oral or depot typical antipsychotics).
Results
A total of 10 972 patients were enrolled at baseline, of which 9107 completed the 12-month study period. Treatment with olanzapine was more effective in terms of QALYs gained than all of the other antipsychotic treatments. Treatment with olanzapine dominated quetiapine and amisulpride. The incremental cost for olanzapine compared with risperidone was £226 per patient over 12 months and the incremental cost per QALY gained was £5156, with bootstrap analyses showing 100% of the replications falling below a £30 000 per QALY gained threshold. Compared with treatment with clozapine, olanzapine was found to be marginally more effective, at an additional cost of £13 per patient over 12 months and to have an incremental cost per QALY gained of £775. Bootstrap analyses showed that 81% of replications fell below a £30 000 per QALY gained threshold. Comparing olanzapine with oral and depot typical antipsychotics, the incremental cost was £849 and £1106 per patient over 12 months and the incremental cost per QALY gained was £15 696 and £23 331, respectively. Bootstrap analyses showed that 98% of the replications fell below a £30 000 per QALY gained threshold for the comparison with oral typical antipsychotics, and 79% of replications for the comparison with depot preparations.
Conclusions
Among SOHO patients, if a funding threshold of £30 000 per QALY gained is assumed, this analysis suggests that olanzapine has a high probability of being the most cost-effective treatment compared with other antipsychotic treatments. However, comparison of olanzapine with clozapine and typical depot antipsychotics should be viewed with caution because clozapine is a second-line treatment and depot treatment is used for patients who do not adhere to their oral medication.









Similar content being viewed by others
References
Davies LM, Lewis S, Jones PB, et al. Cost-effectiveness of first-v second-generation antipsychotic drugs: results from a randomised controlled trial in schizophrenia responding poorly to previous therapy. Br J Psychiatry 2007; 191: 14–22
Haro JM, Edgell ET, Jones PB, et al. The European Schizophrenia Outpatient Health Outcomes (SOHO) study: rationale, methods and recruitment. Acta Psychiatr Scand 2003; 107: 222–232
American Psychiatric Association. Practice guidelines for the treatment of patients with schizophrenia. Am J Psychiatry 2004; 161 Suppl. 2: 1–56
Expert Consensus Panels. The expert consensus guideline series: treatment of schizophrenia 1999. J Clin Psychiatry 1999; 60: 1–82
Lehman AF, Steinwachs DM. Translating research into practice: the schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophr Bull 1998; 24: 1–10
National Institute of Clinical Excellence (NICE). Technology appraisal: guidance on the use of newer (atypical) antipsychotic drugs for the treatment of schizophrenia. NICE Guidance 2002 [online]. Available from URL: http://www.nhshealthquality.org/nhsqis/controller?p_service-Content.sho&p_applic=CCC&pContentID=962 [Accessed 2005 Aug 1]
Black N. What observational studies can offer decision makers. Horm Res 1999; 51 Suppl. 1: 44–49
McKee M, Britton A, Black N, et al. Methods in health services research: interpreting the evidence. Choosing between randomised and non-randomised studies. BMJ 1999; 319: 312–315
Woods K. Filling the gap: how big is it? In: Rawlins M, Littlejohns P, editors. Delivering quality in the NHS 2004. Oxford: Radical Medical Press, National Institute for Clinical Excellence, 2004: 11–13
Haro JM, Edgell ET, Novick D, et al. Effectiveness of anti-psychotic treatment for schizophrenia: 6-month results of the Pan-European Schizophrenia Outpatient Health Outcomes (SOHO) study. Acta Psychiatr Scand 2005; 111: 220–231
Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press, 2005
Netten A, Curtis L. Unit costs of health and social care 2002. Canterbury: PSSRU University of Canterbury, 2002
Netten A, Curtis L. Unit cost of health and social care 2003. Canterbury: PSSRU University of Canterbury, 2003
Netten A, Curtis L. Unit costs of health and social care 2004. Canterbury: PSSRU University of Canterbury, 2004
Monthly Index of Medical Specialities (MIMS). London: Haymarket Publications, 2004 Nov
CMP Medica Ltd. Chemist and druggist supplement 2005 [online]. Available from URL: http://www.cddata.co.uk [Accessed 2005 Aug 1]
IMS Health Inc., MIDAS®, Q2/2004
UK Pharmaceutical Industry Costing Analysis System (PI-CAS®) [database]. Fort Washington (PA): Data Edge, LLC, 1992 (no longer commercially available)
Brooks R. EuroQol: the current state of play. Health Policy 1996; 37: 53–72
Kind P, Hardman G, Macran S. UK population norms for EQ-5D [working paper #172]. York (UK): York Centre for Health Economics, 1999
Covell NH, Jackson CT, Evans AC, et al. Antipsychotic prescribing practices in Connecticut’s public mental health system: rates of changing medications and prescribing styles. Schizophr Bull 2002; 28: 17–29
Windmeijer F, Kontodimas S, Knapp M, et al. Methodological approach for assessing the cost-effectiveness of treatments using longitudinal observational data: the SOHO study. Int J Technol Assess Health Care 2006; 22: 460–468
Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ 2001; 20: 461–494
Santos-Silva JMC, Tenreyro S. The log of gravity. Rev Econ Stat 2006; 88: 641–658
Briggs AH. Handling uncertainty in economic evaluation and presenting the results. In: Drummond M, McGuire A, editors. Economic evaluation in health care: merging theory with practice. Oxford: Oxford University Press, 2001: 172–214
Devlin N, Parkin D. Does NICE have a cost-effectiveness threshold and what other factors influence its decisions? A binary choice analysis. Health Econ 2004; 13: 437–452
Basu A. Cost-effectiveness analysis of pharmacological treatments in schizophrenia: critical review of results and methodological issues. Schizophr Res 2004; 71: 445–462
Woods K. Filling the gap: how big is it? In: Rawlins M, Littlejohns P, editors. Delivering quality in the NHS 2004. Oxford: Radical Medical Press, National Institute for Clinical Excellence, 2004: 11–13
Willan AR, Briggs AH, Hoch JS. Regression methods for covariate adjustment and subgroup analysis for non-censored cost-effectiveness data. Health Econ 2004; 13: 461–475
Willke RJ, Glick HA, Polsky D, et al. Estimating country-specific cost-effectiveness from multinational clinical trials. Health Econ 1998; 7: 481–493
Raikou M, Briggs A, Gray A, et al. Centre-specific or average unit costs in multi-centre studies? Some theory and simulation. Health Econ 2000; 9: 191–198
Szende A. Oppe M, Devlin N, editors. EQ-5D value sets: inventory, comparative review and use guide. Dordrecht: Springer, 2007
Rosenheck RA, Leslie DL, Sindelar J, et al. Cost-effectiveness of second-generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. Am J Psychiatry 2006; 163: 2080–2089
Lieberman JA, Stroup S, McEvoy J, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia: primary efficacy and safety outcomes of the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial. N Engl J Med 2005; 353: 1209–1223
Almond S, O’Donnell O. Cost analysis of the treatment of schizophrenia in the UK. Pharmacoeconomics 2000; 17: 383–389
Davies LM, Drummond MF. Economics and schizophrenia: the real cost. Br J Psychiatry 2004; 165: 18–21
Glazer WM, Johnstone BM. Pharmacoeconomic evaluation of antipsychotic therapy for schizophrenia. J Clin Psychiatry 1997; 10: 50–54
Hamilton SH, Revicki DA, Edgell ET, et al. Clinical and economic outcomes of olanzapine compared with haloperidol for schizophrenia: results from a randomized clinical trial. Pharmacoeconomics 1999; 15: 469–480
Jerrell MJ. Cost-effectiveness of risperidone, olanzapine and conventional antipsychotic medications. Schizophr Bull 2002; 28: 589–605
Le Pen C, Lilliu H, Allicar MP, et al. An economic comparison of olanzapine versus haloperidol in the treatment of schizophrenia in France. Encephale 1999; 25: 281–286
Palmer CS, Revicki DA, Genduso LA, et al. A cost-effective clinical decision analysis model for schizophrenia. Am J Manag Care 1998; 4: 345–355
Rosenheck R, Perlick D, Bingham S, et al. Effectiveness and cost of olanzapine and haloperidol in the treatment of schizophrenia: a randomized controlled trial. JAMA 2003; 290: 693–702
Sacristan J A, Gomez JC, Salvador-Carulla L. Cost effectiveness analysis of olanzapine versus haloperidol in the treatment of schizophrenia in Spain. Actas Luso Esp Neurol Psiquiatr Cienc Afines 1997; 25: 255–234
Tunis SL, Johnstone BM, Gibson PJ, et al. Changes in perceived health and functioning as a cost-effectiveness measure for olanzapine versus haloperidol treatment of schizophrenia. J Clin Psychiatry 1999; 60: 38–45
Laux G, Heeg BMS, van Haut BA, et al. Costs and effects of long-acting risperidone compared with oral atypical and conventional depot formulations in Germany. Pharmacoeconomics 2005; 23 Suppl. 1: 49–61
Gibson P, Damler R, Jackson E, et al. The impact of olanzapine, risperidone, or haloperidol on the cost of schizophrenia care in a Medicaid population. Value Health 2004; 7: 22–35
Lewis M, McCrone P, Frangou S. Service use and costs of treating schizophrenia with atypical antipsychotics. J Clin Psychiatry 2001; 62: 749–756
Byerly MJ, Weber M, Brooks D, et al. Cost evaluation of risperidone compared with olanzapine. Psychiatr Serv 2003; 54: 742–744
Edgell ET, Andersen SW, Johnstone BM, et al. Olanzapine versus risperidone: a prospective comparison of clinical and economic outcomes in schizophrenia. Pharmacoeconomics 2000; 18: 567–579
Fuller MA, Shermock KM, Secic M, et al. Service use and costs among VA patients with schizophrenia taking risperidone or olanzapine. Psychiatric Serv 2002; 53: 855–860
Hueguelet PH, Girardet F. A Swiss retrospective naturalistic outcome study comparing risperidone and olanzapine in the treatment of schizophrenic inpatients. Schwiezer Archiv fur Neuro und Psychi 2002; 153: 282–288
Karki SD, Bellnier TJ, Patil K, et al. Cost effectiveness of atypical antipsychotics in severely and persistently mentally ill patients with schizophrenia and schizoaffective disorders. Drug Ben Trends 2001; 13: 7–12
Lecomte P, Hert M, van Dijk Mark M, et al. A 1-year cost-effectiveness model for the treatment of chronic schizophrenia with acute exacerbations in Belgium. Value Health 2000; 3: 1–11
Rascati KL, Johnsrud MT, Crismon ML, et al. Olanzapine versus risperidone in the treatment of schizophrenia: a comparison of costs among Texas Medicaid recipients. Pharmacoeconomics 2005; 21: 683–697
Taylor DM, Wright T, Libretto SE. Risperidone compared with olanzapine in a naturalistic clinical study: a cost analysis. J Clin Psychiatry 2003; 64: 589–597
Vera-Llonch M, Delea TE, Richardson E, et al. Outcomes and costs of risperidone versus olanzapine in patients with chronic schizophrenia or schizoaffective disorders: a Markov model. Value Health 2004; 7: 569–584
Zhao Z. A retrospective economic evaluation of olanzapine versus risperidone in the treatment of schizophrenia. Manag Care Interface 2002; 15: 75–81
Gureje O, Miles W, Keks N, et al. Olanzapine vs. risperidone in the management of schizophrenia: a randomized double-blind trial in Australia and New Zealand. Schizophr Res 2003; 61: 303–314
Russo PA, Smith MW, Namjoshi M. Healthcare costs for schizophrenia patients started on olanzapine versus risperidone. Am J Health-Syst Pharm 2005; 62: 610–615
Hargreaves WA, Gibson PJ. Effectiveness and cost of risperidone and olanzapine for schizophrenia: a systematic review. CNS Drugs 2005; 19 (5): 393–410
Acknowledgements
The SOHO study is funded by Eli Lilly and Company, Windlesham, Surrey, UK. The SOHO Study Group comprises:
France: J-P. Lepine, Hôspital Fernand Widal, Paris; I. Gasquet, INSERM U 669, Maison des Adolescents, Hôpital Cochin, Paris.
Germany: D. Naber, Universitatskrankenhaus-Eppendorf, Klinik fur Psychiatrie und Psychotherapie, Hamburg.
The Netherlands: C.J. Slooff, Psychosencluster GGX N-Drenthe, Kenniscentrum Scizofrenie, RA Assen.
Spain: J. Alonso, Health Services Research Unit, Institut Municipal D’Investigacio Medica, University of Barcelona, Barcelona; J.M. Haro, Research and development Unit, Sant Joan de Deu-SMM, Sant Boi, Barcelona.
UK: T. Croudace, Department of Psychiatry, Addenbrooke’s Hospital, Cambridge; P.B. Jones, University of Cambridge, Addenbrooke’s Hospital, Cambridge; M. Knapp, PSSRU, London School of Economics, Centre for the Economics of Mental Health, Institute of Psychiatry, London.
The authors thank Mark Belger (Eli Lilly and Company) for his statistical advice and Jo Cooper for her administrative support.
Frank Windmeijer received monetary compensation from Eli Lilly and Company for econometric advice. Martin Knapp and Josep Maria Haro were paid by Eli Lilly and Company for their participation in the SOHO Advisory Board. Stathis Kontodimas, Jacqueline Brown, Mark Ratcliffe and Diego Novick are Eli Lilly employees. Spyridon Tzivelekis was an Eli Lilly employee at the time of submission. Jihyung Hong is working at the London School of Economics as a research assistant and also as consultant for Eli Lilly and Company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Knapp, M., Windmeijer, F., Brown, J. et al. Cost-Utility Analysis of Treatment with Olanzapine Compared with Other Antipsychotic Treatments in Patients with Schizophrenia in the Pan-European SOHO Study. Pharmacoeconomics 26, 341–358 (2008). https://doi.org/10.2165/00019053-200826040-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200826040-00006