Abstract
Synopsis
Desflurane is a halogenated ether inhalation general anaesthetic agent with low solubility in blood and body tissues, and approximately one-fifth the potency of isoflurane. The pharmacodynamic properties of desflurane generally resemble those of isoflurane; thus, it produces dose-dependent depression of the central nervous and cardiorespiratory systems, and tetanic fade at the neuromuscular junction.
The alveolar equilibration of desflurane is rapid (90% complete at 30 minutes compared with 73% for isoflurane). Both desflurane and isoflurane are distributed to various tissues to a similar extent. Desflurane is resistant to chemical degradation and undergoes negligible metabolism (≈10% of that seen with isoflurane). Desflurane ‘wash-out’ is ≈2 to 2.5 times faster than that of isoflurane in the first 2 hours after discontinuation of anaesthesia.
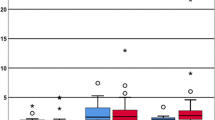
The low solubility of desflurane facilitates a rapid induction of anaesthesia and precise control of the depth of anaesthesia (during maintenance). Results from a few clinical studies indicate that emergence from desflurane is significantly earlier (by ≈2 to 6 minutes) than that from propofol anaesthesia, whereas other studies do not concur. In comparison with isoflurane, emergence from desflurane anaesthesia is significantly earlier (by 5 minutes) after ambulatory and ≈50% earlier (also significant) after nonambulatory surgical procedures. Limited comparative studies with halothane or sevoflurane also suggest an earlier time of emergence from desflurane anaesthesia.
Comparative studies of desflurane and propofol, and other inhalation agents, indicate that the times to toleration of oral fluids, sitting and discharge from recovery room are similar, regardless of the general anaesthetic agent administered. However, some limited data in elderly patients (aged >65 years) suggest that this patient group spends a significantly shorter time in the postanaesthesia care unit after desflurane than after isoflurane anaesthesia.
Differences, if any, in the recovery of cognitive and psychomotor functions after desflurane or propofol anaesthesia remain unclear. However, in comparison with isoflurane anaesthesia, recovery of these functions (up to 45 minutes post-operatively) occurs earlier after desflurane. Significantly fewer patients are subjectively impaired (i.e. drowsy, clumsy, fatigued or confused) upon recovery from desflurane than from isoflurane anaesthesia. Likewise, significantly fewer adult patients are delirious when recovering from desflurane than from isoflurane anaesthesia, though in paediatric patients delirium is more likely when recovering from desflurane than from halothane anaesthesia.
Haemodynamic stability during coronary artery surgery is as well maintained with desflurane as with isoflurane, and the drug does not worsen the adverse postoperative outcomes. Moreover, desflurane appears to be better than isoflurane at blunting the haemodynamic response after sternotomy and other noxious stimuli. The incidence of myocardial ischaemia during coronary artery surgery is similar with either desflurane or isoflurane anaesthesia.
Transient airway irritant effects are the most common adverse events during induction of anaesthesia with deseflurane; therefore, this agent is not recommended for induction of anaesthesia in paediatric patients. The incidence of intraoperative cardiovascular events during desflurane anaesthesia is similar to that reported with isoflurane. The incidence of postoperative nausea and vomit-ing after desflurane anaesthesia is higher than after propofol but similar to that after other inhalation agents. Hepatic or renal function is not adversely affected after desflurane anaesthesia.
Overall, although desflurane is generally not well tolerated during induction of anaesthesia, it embodies many of the desirable feature s of an ideal agent, which include stability to chemical degradation, low solubility in blood and body tissues, negligible metabolism and low potential for hepato-renal toxicity. These favourable physical and pharmacokinetic characteristics should present desflurane as a valuable inhalation anaesthetic agent for the maintenance of general anaesthesia in ambulatory surgery (complementary to intravenous induction with propofol) as well as in nonambulatory surgical procedures.
Pharmacodynamic Properties
Desflurane is a halogenated ether inhalation general anaesthetic agent with low solubility in blood and body tissues and low potency [minimum alveolar concentration (MAC) value ranging from 4.58 to 7.25%, depending on the stimulus used]. It is approximately one-fifth as potent as isoflurane.
The cerebrovascular and cardiorespiratory effects of desflurane essentially parallel those of isoflurane. It produces dose-dependent decreases in cerebrovascular resistance and cerebral metabolic rate of oxygen consumption, increases in intracranial pressure at 0.5 to 1.5 MAC doses and impairment of cerebral autoregulation.
Desflurane suppresses EEG activity at ≥1.24 MAC, and it is not epileptogenic either at deep anaesthetic levels or under hypocapnic conditions. There is a dose-dependent suppression of somatosensory-evoked potentials at 0.5 to >1.5 MAC in healthy volunteers, while sub-MAC concentrations suppress intermediate-latency auditory-evoked responses.
Cardiac output is maintained in humans despite dose-dependent depression of cardiovascular function and myocardial contractility during desflurane anaesthesia with controlled ventilation. Tachycardia may be more prominent with desflurane than isoflurane at >1.0 MAC. Adequate myocardial tissue perfusion is maintained despite a decline in perfusion pressure during desflurane anaesthesia. Prolonged anaesthesia (up to 7 hours) appears to result in cardiovascular, but not cerebral, tolerance in humans. Desflurane, like isoflurane, is a coronary vasodilator, but it does not appear to induce the ‘coronary steal’ phenomenon in a canine model.
A rapid increase in end-tidal concentrations of desflurane (at ≥1.0 MAC) in patients and healthy volunteers results in transient sympathetic-mediated cardiovascular stimulation which is significantly more pronounced than that observed with isoflurane. This sympathoexcitation is absent with sevoflurane.
Dose-dependent respiratory depressant effects of desflurane (at ≤1.24 MAC), such as decrease in tidal volume and increase in ventilation rate, are similar to those of isoflurane. Desflurane produces neuromuscular relaxation and therefore potentiates skeletal muscle relaxation induced by neuromuscular blocking agents.
Pharmacokinetic Properties
Equilibration between inspired and tissue concentrations of desflurane is rapid compared with that of other inhalation anaesthetic agents. Alveolar equilibration of desflurane is ≈90% complete in healthy volunteers within 30 minutes compared with isoflurane (73%) or halothane (58%). The estimated tissue distribution of desflurane is generally similar to that of isoflurane.
Desflurane is eliminated ≈2 to 2.5 times more quickly than isoflurane or halothane in the first 2 hours after discontinuation of anaesthesia. Pulmonary clearance of desflurane is 4.11 L/min (vs 3.94 L/min for isoflurane and halothane) and total body clearance is 4.60 L/min (vs 4.00 and 3.94 L/min for isoflurane and halothane, respectively).
Desflurane is resistant to in vitro degradation in moist soda lime at ≤60°C, although there is slight degradation at 80°C (0.45% per hour). Desflurane undergoes negligible metabolism (≈10% that of isoflurane) in vivo, although the precise mechanism is unknown.
Clinical Evaluation
A number of studies in ambulatory patients report a statistically significant earlier emergence from desflurane than from propofol or isoflurane anaesthesia (≈2 to 6 and 5 minutes earlier, respectively), although some studies have not found this difference between desflurane and propofol anaesthesia. Emergence from desflurane anaesthesia in this group of patients appears to be significantly more rapid than emergence from sevoflurane or halothane anaesthesia. The times to toleration of oral fluids, sitting and readiness for discharge from the recovery room are comparable, regardless of the general anaesthetic administered.
In the early postoperative period up to 90 minutes, psychomotor and cognitive functions are less impaired after desflurane than after isoflurane ambulatory anaesthesia, whereas such differences are less apparent when desflurane is compared with propofol. Generally, these functions return to their baseline levels within 2 hours postoperatively regardless of the anaesthetic background. Subjective impairment (i.e. drowsiness, clumsiness, fatigue or confusion) is significantly less upon recovery from desflurane than from isoflurane anaesthesia.
Emergence from nonambulatory anaesthesia with desflurane is ≈50% significantly earlier than that with isoflurane. In addition, up to 45 minutes postoperatively, cognitive and psychomotor function recovery occurs earlier after desflurane than after isoflurane anaesthesia, although this difference is not apparent 60 minutes after cessation of administration.
Elderly patients (aged >65 years) recovering from nonambulatory desflurane anaesthesia tend to spend a shorter time in the postanaesthesia care unit compared with those who received isoflurane anaesthesia (80 vs 128 minutes).
Desflurane does not worsen the adverse postoperative outcomes after coronary artery surgery, and haemodynamic stability during desflurane anaesthesia is similar to that during isoflurane or opioid anaesthesia. Compared with isoflurane, desflurane is better at blunting the haemodynamic response after sternotomy and other noxious stimuli. There is no difference between desflurane and isoflurane anaesthesia with respect to the incidence of ECG changes indicative of myocardial ischaemia during coronary artery surgery. However, when desflurane is compared with opioid anaesthesia, conflicting results with respect to the incidence of myocardial ischaemia upon induction, but not during maintenance of anaesthesia, were reported. Changes in the depth of anaesthesia in response to surgical stimuli are more rapidly controlled with desflurane than with isoflurane.
Limited data suggest that desflurane (1 to 4.5%) in oxygen provides well tolerated and effective obstetric analgesia during vaginal delivery. Likewise, caesarean section surgery can be performed without excessive uterine bleeding when desflurane 3% (end-tidal concentration) is administered.
Tolerability
The pungency of desflurane is reflected in its transient airway irritant effects during induction of anaesthesia at concentrations >6%. These effects (commonly seen in adults) include coughing, excitatory effects, breath-holding, excessive secretions and laryngospasm. The airway irritant effects are not well tolerated by paediatric patients, in whom excitatory effects (51 %) and coughing (29%) are the most commonly reported reflexes. Other adverse events include apnoea, pharyngitis and oxyhaemoglobin desaturation (SpO2 <90%).
Haemodynamic stability during maintenance of anaesthesia with desflurane is generally well preserved and similar to that during isoflurane, propofol or halothane anaesthesia. The incidence of a number of cardiovascular events occurring during desflurane anaesthesia, namely, tachycardia, bradycardia, hypertension, hypotension and nodal arrhythmias, is not significantly different from that with isoflurane.
Postoperative nausea is reported in 10 to 54% of adult and paediatric patients after desflurane anaesthesia, whereas vomiting occurs in 7 to 33% of patients. Significantly fewer adult patients experience delirium when recovering from desflurane anaesthesia than when recovering from isoflurane anaesthesia (0 to 13% vs 44 to 75%). In contrast, paediatric patients tend to be delirious more frequently after emergence from desflurane than from halothane anaesthesia.
Hepatic or renal function is not affected by desflurane anaesthesia up to 7.35 MAC-hours. Desflurane, given at 2.8 to 3% for 2.0 to 2.5 hours, does not worsen chronic hepatic or renal disease. To date, malignant hyperthermia has not been reported with desflurane anaesthesia in humans.
Dosage and Administration
Inspired concentrations of 4 to 11 % desflurane usually produce surgical anaesthesia in adult patients, with or without premedication with opioids, in 2 to 4 minutes. Induction of anaesthesia with desflurane is not recommended in paediatric patients aged <12 years.
Surgical anaesthesia in adult patients may be maintained with concentrations of 2 to 6% desflurane with concomitant use of nitrous oxide and 2.5 to 8.5% when oxygen is used concomitantly. Surgical anaesthesia in paediatric patients may be maintained with concentrations of 5.2 to 10% desflurane with or without the concomitant use of nitrous oxide.
Concentrations of 1 to 4% desflurane in nitrous oxide-oxygen are recommended for maintenance of anaesthesia in patients with chronic renal or hepatic impairment and during renal transplantation surgery.
Desflurane is currently not recommended for administration to neurosurgical patients (except in the US, where it is authorised for this patient group, provided it is administered at ≤0.8 MAC), during pregnancy, or in patients with known or suspected genetic susceptibility to malignant hyperthermia.
Nitrous oxide, opioids, benzodiazepines and other sedative agents reduce the MAC of desflurane. Desflurane potentiates the pharmacological activity of neuromuscular blocking agents in a dose-dependent manner.
Similar content being viewed by others
References
Kennedy SK, Longnecker DE. History and principles of anesthesiology. In: Gilman AG, Rall TW, Nies AS, et al., editors. Goodman and Gilman’s the pharmacological basis of therapeutics. 8th ed. New York: Pergamon Press, 1990: 269–84
Calverly RK. Fluorinated anesthetics. 1. The early years 1932–1946. Survey of Anesthesiology 1986; 30: 170–3
Robbins BH. Preliminary studies of the anesthetic activity of fluorinated hydrocarbons. J Pharmacol Exp Ther 1946; 86: 197–204
Vitcha JF. A history of Forane [editorial]. Anesthesiology 1971 Jul; 35(1): 4–7
Wallin RF, Napoli MD, Regan BM. Laboratory investigation of a new series of inhalational anesthetic agents: the halomethyl polyfluorisopropyl ethers. In: Fink BR, editor. Symposium on cellular biology and toxicity of anesthetics; Seattle May 11-12, 1970. Baltimore: Williams and Wilkins, 1972: 285–95
Bryce-Smith R, O’Brien HD. Fluothane: a non-explosive volatile anaesthetic agent. BMJ 1956 Oct; 2: 969–72
Johnstone M. The human cardiovascular response to Fluothane anaesthesia. Br J Anaesth 1956; 28: 392–410
Suckling CW. Some chemical and physical features in the development of Fluothane. Br J Anaesth 1957; 29: 466–72
Jones RM. Desflurane and sevoflurane: inhalation anaesthetics for this decade? Br J Anaesth 1990 Oct; 65: 527–36
Marshall BE, Longnecker DE. General Anesthetics. In: Gilman AG, Rail TW, Nies AS, et al., editors. Goodman and Gilman’s the pharmacological basis of therapeutics. 8th ed. New York: Pergamon, 1990:285–310
Eger El. Desflurane animal and human pharmacology: aspects of kinetics, safety, and MAC. Anesth Analg 1992 Oct; 75 Suppl. 4: S3–9
Rampil IJ, Lockhart SH, Zwass MS, et al. Clinical characteristics of desflurane in surgical patients: minimum alveolar concentration. Anesthesiology 1991 Mar; 74(3): 429–33
Quasha AL, Eger El, Tinker JH. Determination and applications of MAC. Anesthesiology 1980 Oct; 53(4): 315–34
Katoh T, Ikeda K. The minimum alveolar concentration (MAC) of sevoflurane in humans. Anesthesiology 1987 Mar; 66(3): 301–3
Hornbein TF, Eger EI, Winter PM, et al. The minimum alveolar concentration of nitrous oxide in man. Anesth Analg 1982 Jul; 61(7): 553–6
Eger EI. Partition coefficients of I-653 in human blood, saline, and olive oil. Anesth Analg 1987 Oct; 66: 971–3
Malviya S, Lerman J. The blood/gas solubilities of sevoflurane, isoflurane, halothane, and serum constituent concentrations in neonates and adults. Anesthesiology 1990 May; 72(5): 793–6
Kety SS, Harmel MH, Broomell HT, et al. The solubility of nitrous oxide in blood and brain. J Biol Chem 1948; 173: 487–96
Yasuda N, Targ AG, Eger EI. Solubility of I-653, sevoflurane, isoflurane, and halothane in human tissues. Anesth Analg 1989 Sep; 69: 370–3
Eger EI. New inhaled anesthetics. Anesthesiology 1994 Apr; 80(4): 906–22
Eger EI, Saidman LJ, Brandstater B. Minimum alveolar anesthetic concentration: a standard of anesthetic potency. Anesthesiology 1965 Nov-Dec; 26(6): 756–63
Taylor RH, Lerman J. Minimum alveolar concentration of desflurane and hemodynamic responses in neonates, infants, and children. Anesthesiology 1991 Dec; 75(6): 975–9
Fisher DM, Zwass MS. MAC of desflurane in 60% nitrous oxide in infants and children. Anesthesiology 1992 Mar; 76: 354–6
Gold MI, Abello D, Herrington C. Minimum alveolar concentration of desflurane in patients older than 65 yr. Anesthesiology 1993 Oct; 79(4): 710–4
Sebel PS, Glass PSA, Fletcher JE, et al. Reduction of the MAC of desflurane with fentanyl. Anesthesiology 1992 Jan; 76(1): 52–9
Ghouri AF, White PF. Effect of fentanyl and nitrous oxide on the desflurane anesthetic requirement. Anesth Analg 1991 Mar; 72: 377–81
Glosten B, Faure EAM, Lichtor JL, et al. Desflurane MAC is decreased but recovery time is unaltered following premedi-cation with midazolam (0.05mg/kg) [abstract]. Anesthesiology 1990 Sep; 73 Suppl. 3A: A346
Eger El, Johnson BH. MAC of I-653 in rats, including a test of the effect of body temperature and anesthetic duration. Anesth Analg 1987 Oct; 66: 974–6
Jones RM, Cashman JN, Eger EI, et al. Kinetics and potency of desflurane (I-653) in volunteers. Anesth Analg 1990 Jan; 70: 3–7
Stoelting R, Longnecker D, Eger EI. Minimum alveolar concentrations in man on awakening from methoxyflurane, halothane, ether and fluorexene anesthesia: MAC awake. Anesthesiology 1970 Jul; 33(1): 5–9
Chortkoff BS, Eger EI, Crankshaw D, et al. Concentrations of desflurane and propofol that suppress response to command in human volunteers [abstract]. Anesth Analg 1994; 78: S59
Eger EI, Strum DP. The absorption and degradation of isoflurane and I-653 by dry soda lime at various temperatures. Anesth Analg 1987 Dec; 66: 1312–5
Targ AG, Yasuda N, Eger EI. Solubility of I-653, sevoflurane, isoflurane, and halothane in plastics and rubber composing a conventional anesthetic circuit. Anesth Analg 1989 Aug; 69: 218–25
Eger EI. Stability of I-653 in soda lime. Anesth Analg 1987 Oct; 66: 983–5
Van Poznak A, Artusio JF. Anesthetic properties of a series of fluorinated compounds. I. Fluorinated hydrocarbons. Toxicol Appl Pharmacol 1960; 2: 363–73
Fang ZX, Eger EI, Laster MJ, et al. Carbon monoxide production from degradation of desflurane, enflurane, isoflurane, halothane, and sevoflurane by soda lime and Baralyme. Anesth Analg 1995; 80: 1187–93
Franks NP, Lieb WR. Molecular and cellular mechanisms of general anaesthesia. Nature 1994 Feb; 367: 607–14
Yost CS. G proteins: basic characteristics and clinical potential for the practice of anesthesia. Anesth Analg 1993 Oct; 77(4): 822–34
Kosk-Kosicka D, Roszczynska G. Inhibition of plasma membrane Ca2+-ATPase activity by volatile anesthetics. Anesthesiology 1993 Oct; 79(4): 774–80
Warltier DC, Pagel PS. Cardiovascular and respiratory actions of desflurane: is desflurane different from isoflurane? Anesth Analg 1992 Oct; 75 Suppl. 2: S17–31
Watson NA, Jones RM. Desflurane. Baillieres Clin Anaesth 1993 Dec; 7(4): 873–97
Caldwell JE. Desflurane clinical pharmacokinetics and pharmacodynamics. Clin Pharmacokinet 1994 Jul; 27: 6–18
Young WL. Effects of desflurane on the central nervous system. Anesth Analg 1992 Oct; 75 Suppl. 4: S32–7
Lutz LJ, Milde JH, Milde LN. The cerebral functional, metabolic, and hemodynamic effects of desflurane in dogs. Anesthesiology 1990 Jul; 73(1): 125–31
Artru AA, Powers K, Doepfner P. CSF, sagittal sinus, and jugular venous pressures during desflurane or isoflurane anesthesia in dogs [abstract]. Anesth Analg 1995; 80: S17
Ornstein E, Young WL, Fleischer LH, et al. Desflurane and isoflurane have similar effects on cerebral blood flow in patients with intracranial mass lesions. Anesthesiology 1993 Sep; 79(3): 498–502
Brenet O, Granry JC, Jacob JP, et al. Effects of desflurane on cerebral blood flow velocity in children [abstract]. Br J Anaesth 1995 May; 74 Suppl. 1: A318
Muzzi DA, Losasso TJ, Dietz NM, et al. The effect of desflurane and isoflurane on cerebrospinal fluid pressure in humans with supratentorial mass lesions. Anesthesiology 1992 May; 76(5): 720–4
Milde LN, Milde JH. The cerebral and systemic hemodynamic and metabolic effects of desflurane-induced hypotension in dogs. Anesthesiology 1991 Mar; 74(3): 513–8
Strebel S, Lam AM, Matta B, et al. Dynamic and static cerebral autoregulation during isoflurane, desflurane, and propofol anesthesia. Anesthesiology 1995 July; 83(1): 66–76
Rampil IJ, Lockhart SH, Eger EI, et al. The electroencephalographic effects of desflurane in humans. Anesthesiology 1991 Mar; 74: 434–9
Black S, Konstadt SN, Sami H, et al. Effect of I-653 (desflurane) on somatosensory evoked potentials [abstract]. Anesthesiology 1990 Sep; 73 Suppl. 3A: A181
Cahalan MK, Weiskopf RB, Eger EI, et al. Hemodynamic effects of desflurane/nitrous oxide anesthesia in volunteers. An-esth Analg 1991 Aug; 73: 157–64
Weiskopf RB, Cahalan MK, Eger EI, et al. Cardiovascular actions of desflurane in normocarbic volunteers. Anesth Analg 1991 Aug; 73: 143–56
Cromwell TH, Stevens WC, Eger EI, et al. The cardiovascular effects of compound 469 (Forane) during spontaneous ventilation and CO2 challenge in man. Anesthesiology 1971 Jul; 35(1): 17–25
Weiskopf RB, Cahalan MK, Ionescu P, et al. Cardiovascular actions of desflurane with and without nitrous oxide during spontaneous ventilation in humans. Anesth Analg 1991 Aug; 73: 165–74
Weiskopf RB, Holmes MA, Rampil IJ, et al. Cardiovascular safety and actions of high concentrations of I-653 and isoflurane in swine. Anesthesiology 1989 May; 70(5): 793–8
Hartman JC, Pagel PS, Kampine JP, et al. Influence of desflurane on regional distribution of coronary blood flow in a chronically instrumented canine model of multivessel coronary artery obstruction. Anesth Analg 1991 Mar; 72: 289–99
Weiskopf RB, Eger EI, Noorani M, et al. Repetitive rapid increases in desflurane concentration blunt transient cardiovascular stimulation in humans. Anesthesiology 1994 Oct; 81(4): 843–9
Weiskopf RB, Moore MA, Eger EI, et al. Rapid increase in desflurane concentration is associated with greater transient cardiovascular stimulation than with rapid increase in isoflurane concentration in humans. Anesthesiology 1994 May; 80(5): 1035–45
Moore MA, Weiskopf RB, Eger EI, et al. Rapid 1% increases of end-tidal desflurane concentration to greater than 5% transiently increase heart rate and blood pressure in humans. Anesthesiology 1994 Jul; 81(1): 94–8
Ebert TJ, Muzi M. Sympathetic hyperactivity during desflurane anesthesia in healthy volunteers. A comparison with isoflurane. Anesthesiology 1993 Sep; 79(3): 444–53
Ostapkovich N, Ornstein E, Jackson L, et al. Hemodynamic changes with rapid increases in desflurane or isoflurane dose [abstract]. Anesthesiology 1992 Sep; 77 Suppl. 3A: A333
Ciofolo MJ, Jansson E, Johansson G, et al. Sympathetic activation of desflurane is not mediated by airway or lung receptors [abstract]. Br J Anaesth 1995 May; 74 Suppl. 1: A128
Ishikawa T, Nishino T, Hiraga K. Immediate responses of arterial blood pressure and heart rate to sudden inhalation of high concentrations of isoflurane in normotensive and hypertensive patients. Anesth Analg 1993; 77: 1022–5
Yli-Hankala A, Randell T, Seppälä T, et al. Increases in hemodynamic variables and catecholamine levels after rapid increase in isoflurane concentration. Anesthesiology 1993 Feb; 78(2): 266–71
Yonker-Sell A, Muzi M, Lopatka CW, et al. Desflurane produces greater sympathetic excitation than isoflurane during slow, controlled increases [abstract]. Anesth Analg 1995; 80: S571
Ebert TJ, Muzi M, Lopatka CW. Neurocirculatory responses to sevoflurane. A comparison to desflurane. Anesthesiology 1995 July; 83(1): 88–95
Schmeling WT, Seagard JL, Perez F. The effects of isoflurane and desflurane on carotid baroreceptor afferent activity in dogs [abstract]. Anesth Analg 1995; 80: S417
Lopatka CW, Muzi M, Foley P, et al. Slow desflurane increases do not attenuate the sympathoexcitatory response in humans [abstract]. Anesthesiology 1994 Sep; 81 Suppl. 3A: A136
Muzi M, Pacentine GG, Lopatka CW, et al. Lidocaine airway anaesthesia does not attenuate sympathetic activation during desflurane administration in humans [abstract]. Anesthesiology 1994 Sep; 81 Suppl. 3A: A370
Weiskopf RB, Eger EI, Noorani M, et al. Fentanyl, esmolol, and clonidine blunt the transient cardiovascular stimulation induced by desflurane in humans. Anesthesiology 1994 Dec; 81(6): 1350–5
Devcic A, Muzi M, Ebert TJ. The effects of clonidine on desflurane-mediated sympathoexcitation in humans. Anesth Analg 1995; 80: 773–9
Pacentine GG, Muzi M, Kampine JP, et al. The effects of nitrous oxide (N2O) on the neurocirculatory responses to desflurane anesthesia [abstract]. Anesth Analg 1994; 78: S331
Pacentine GG, Muzi M, Ebert TJ. Effects of fentanyl on sympathetic activation associated with the administration of desflurane. Anesthesiology 1995 Apr; 82(4): 823–31
Grundmann U, Müller M, Larsen B, et al. Haemodynamic effects of desflurane and isoflurane in patients with coronary artery disease [abstract]. Br J Anaesth 1995 June; 74 Suppl. 2: A48
Jones RM, Cashman JN, Mant TGK. Clinical impressions and cardiorespiratory effects of a new fluorinated inhalation anaesthetic, desflurane (1-653), in volunteers. Br J Anaesth 1990 Jan; 64: 11–5
Hartman JC, Pagel PS, Proctor LT, et al. Influence of desflurane, isoflurane and halothane on regional tissue perfusion in dogs. Can J Anaesth 1992; 39(8): 877–87
Merin RG, Bernard J-M, Doursout M-F, et al. Comparison of the effects of isoflurane and desflurane on cardiovascular dynamics and regional blood flow in the chronically instrumented dog. Anesthesiology 1991 Mar; 74(3): 568–74
Zbinden AM, Petersen-Felix S, Thomson DA. Anesthetic depth defined using multiple noxious stimuli during isoflurane/ox-ygen anesthesia. II. Hemodynamic responses. Anesthesiology 1994 February; 80(2): 261–7
Yasuda N, Weiskopf RB, Cahalan MK, et al. Does desflurane modify circulatory responses to stimulation in humans? Anesth Analg 1991 Aug; 73: 175–9
Lockhart SH, Rampil IJ, Yasuda N, et al. Depression of ventilation by desflurane in humans. Anesthesiology 1991 Mar; 74(3): 484–8
Fourcade HE, Stevens WC, Larson CP, et al. The ventilatory effects of Forane, a new inhaled anesthetic. Anesthesiology 1971 Jul; 35(1): 26–31
Brichant J-F, Gunst SJ, Warner DO, et al. Halothane, enflurane, and isoflurane depress the peripheral vagal motor pathway in isolated canine trachéal smooth muscle. Anesthesiology 1991; 74: 325–32
Warner D, Vettermann J, Brichant J-F, et al. Direct and neurally mediated effects of halothane on pulmonary resistance in vivo. Anesthesiology 1990 Jun; 72(6): 1057–63
Mazzeo AJ, Cheng EY, Bosnjak ZJ, et al. Topographical differences in the direct effects of desflurane and halothane on canine airway smooth muscle [abstract]. Anesth Analg 1994; 78: S274
Lee C, Tsai S-K, Kwan W-F, et al. Desflurane potentiates atracurium in humans: a comparative study with isoflurane. J Clin Anesth 1992 Nov-Dec; 4: 448–54
Azad SS, Bartkowski RR, Witkowski TA, et al. A comparison of desflurane and isoflurane in prolonged surgery. J Clin Anesth 1993 Mar-Apr; 5: 122–8
Caldwell JE, Laster MJ, Magorian T, et al. The neuromuscular effects of desflurane, alone and combined with pancuronium or succinylcholine in humans. Anesthesiology 1991 Mar; 74: 412–8
Wright PMC, Hart P, Lau M, et al. The magnitude and time course of vecuronium potentiation by desflurane versus isoflurane. Anesthesiology 1995 Feb; 82(2): 404–11
Tuchy GL, Tuchy E, Bleyberg M, et al. Pharmacodynamics of mivacurium during desflurane anesthesia [abstract]. Anesthesiology 1994 Sep; 81 Suppl. 3A: A1116
Yasuda N, Lockhart SH, Eger El, et al. Kinetics of desflurane, isoflurane, and halothane in humans. Anesthesiology 1991 Mar; 74(3): 489–98
Allison JM, Gregory RS, Birch KP, et al. Determination of anaesthetic agent concentration by refractometry. Br J Anaesth 1995 Jan; 74: 85–8
Edmondson W. Gas analysis by refractive index measurement. Br J Anaesth 1957; 29: 570–4
Hulands GH, Nunn JF. Portable interference refractometers in anaesthesia. Br J Anaesth 1970; 42: 1051–9
Sugg BR, Palayiwa E, Davies WL. An automated interferometer for the analysis of anaesthetic gas mixtures. Br J Anaesth 1988; 61: 484–91
Lockhart SH, Cohen Y, Yasuda N, et al. Cerebral uptake and elimination of desflurane, isoflurane, and halothane from rabbit brain: an in vivo NMR study. Anesthesiology 1991 Mar; 74(3): 575–80
Litt L, Lockhart S, Cohen Y, et al. In vivo 19F nuclear magnetic resonance brain studies of halothane, isoflurane, and desflurane. Rapid elimination and no abundant saturable binding. Ann N Y Acad Sci 1991; 625: 707–24
Graham SG. New drug in volatile anaesthesia — desflurane. Ann Acad Med Singapore 1994 Jul; 23: 510–8
Carpenter RL, Eger EI, Johnson BH, et al. Pharmacokinetics of inhaled anesthetics in humans: measurements during and after simultaneous administration of enflurane, halothane, isoflurane, methoxyflurane, and nitrous oxide. Anesth Analg 1986; 65: 575–82
Fassoulaki A, Lockhart SH, Freire BA, et al. Percutaneous loss of desflurane, isoflurane, and halothane in humans. Anesthesiology 1991 Mar; 74: 479–83
Laster MJ, Taheri S, Eger El, et al. Visceral losses of desflurane, isoflurane, and halothane in swine. Anesth Analg 1991 Aug; 73: 209–12
Kharasch ED, Thummel KE. Identification of cytochrome P450 2E1 as the predominant enzyme catalyzing human liver mi-crosomal defluorination of sevoflurane, isoflurane, and methoxyflurane. Anesthesiology 1993 Oct; 79(4): 795–807
Holaday DA, Fiserova-Bergerova V, Latto IP, et al. Resistance of isoflurane to biotransformation in man. Anesthesiology 1975 September; 43(3): 325–32
Koblin DD, Weiskopf RB, Holmes MA, et al. Metabolism of I-653 and isoflurane in swine. Anesth Analg 1989 Feb; 68: 147–9
Koblin DD, Eger EI, Johnson BH, et al. I-653 resists degradation in rats. Anesth Analg 1988 Jun; 67: 534–8
Sutton TS, Koblin DD, Gruenke LD, et al. Fluoride metabolites after prolonged exposure of volunteers and patients to desflurane. Anesth Analg 1991 Aug; 73: 180–5
Smiley RM, Ornstein E, Pantuck EJ, et al. Metabolism of desflurane and isoflurane to fluoride ion in surgical patients. Can J Anaesth 1991 Nov; 38(8): 965–8
Weiskopf RB, Eger EI, Ionescu P, et al. Desflurane does not produce hepatic or renal injury in human volunteers. Anesth Analg 1992 Apr; 74: 570–4
Jones RM, Koblin DD, Cashman JN, et al. Biotransformation and hepato-renal function in volunteers after exposure to desflurane (1-653). Br J Anaesth 1990 Apr; 64: 482–7
Lebenbom-Mansour MH, Pandit SK, Kothary SP, et al. Desflurane versus propofol anesthesia: a comparative analysis in outpatients. Anesth Analg 1993 May; 76: 936–41
Rapp SE, Conahan TJ, Pavlin DJ, et al. Comparison of desflurane with propofol in outpatients undergoing peripheral orthopedic surgery. Anesth Analg 1992 Oct; 75: 572–9
Wrigley SR, Fairfield JE, Jones RM, et al. Induction and recovery characteristics of desflurane in day case patients: a comparison with propofol. Anaesthesia 1991 Aug; 46: 615–22
Graham SG, Aitkenhead AR. A comparison between propofol and desflurane anaesthesia for minor gynaecological laparo-scopic surgery. Anaesthesia 1993 Jun; 48: 471–5
Kallar SK, Everett LL. Desflurane versus propofol for outpatient laparoscopic surgery [abstract]. Anesthesiology 1991 Sep; 75 Suppl. 3A: A10
Thirion AV, Clergue F, Seebacher J, et al. Desflurane with or without N2O vs propofol for outpatient laparoscopy [abstract]. Anesthesiology 1991 Sep; 75 Suppl. 3A: A18
Van-Hemelrijck J, Smith I, White PF. Use of desflurane for outpatient anesthesia. A comparison with propofol and nitrous oxide. Anesthesiology 1991 Aug; 75(2): 197–203
Ghouri AF, Bodner M, White PF. Recovery profile after desflurane-nitrous oxide versus isoflurane-nitrous oxide in outpatients. Anesthesiology 1991 Mar; 74(3): 419–24
Fletcher JE, Sebel PS, Murphy MR, et al. Psychomotor performance after desflurane anesthesia: a comparison with isoflurane. Anesth Analg 1991 Sep; 73: 260–5
Dixon RA, Thornton JA. Tests of recovery from anaesthesia and sedation: intravenous diazepam in dentistry. Br J Anaesth 1973; 45: 207–15
Zimmerman IL, Woo-Sam JM. Digit Symbol. In: Zimmerman IL, Woo-Sam JM, editors. Clinical interpretation of the Wechsler adult intelligence scale. New York: Grune and Strat-ton, 1973: 121–31
Newman MG, Trieger N, Miller JC. Measuring recovery from anesthesia: a simple test. Anesth Analg 1969 Jan-Feb; 48(1): 136–40
Wernberg M, Nielson SF, Hommelgaard P. A comparison between reaction time measurement and critical flicker fusion frequency under rising nitrous oxide inhalation in healthy subjects. Acta Anaesthesiol Scand 1980; 24: 86–9
Tsai SK, Lee C, Kwan W-F, et al. Recovery of cognitive functions after anaesthesia with desflurane or isoflurane and nitrous oxide. Br J Anaesth 1992 Sep; 69: 255–8
Hindmarch I, Bhatti JZ. Recovery of cognitive and psychomotor function following anaesthesia: a review. In: Hindmarch I, Jones JG, Moss E, editors. Aspects of recovery from anaesthesia. New York: John Wiley & Sons Ltd., 1987: 113–26
Bond A, Lader M. The use of analogue scales in rating subjective feelings. Br J Med Psychol 1974; 47: 211–8
Dexter F, Tinker JH. Comparisons between desflurane and isoflurane or propofol on time to following commands and time to discharge. Anesthesiology 1995 Jul; 83(1): 77–82
O’Connor TC, Abram SE. Inhibition of nociception-induced spinal sensitization by anesthetic agents. Anesthesiology 1995 Jan; 82(1): 259–66
Rane K, Jakobsson J, Ryberg G. Anaesthesia for laparoscopic gynaecological surgery. A comparison between desflurane and isoflurane [abstract]. Br J Anaesth 1995 May; 74 Suppl. l: A20
Nathanson MH, Fredman B, Smith I, et al. Recovery profiles after outpatient anaesthesia: sevoflurane vs desflurane [abstract]. Br J Anaesth 1994 Nov; 73: 722P
Welborn LG, Frazier LJ, Hannallah RS, et al. Comparison of emergence of recovery characteristics of sevoflurane. desflurane and halothane in pediatric patients [abstract]. Anesth An-alg 1995; 80: S550
Zwass MS, Fisher DM, Welborn LG, et al. Induction and maintenance characteristics of anesthesia with desflurane and nitrous oxide in infants and children. Anesthesiology 1992 Mar; 76(3): 373–8
Davis PJ, Cohen IT, McGowan FX, et al. Recovery characteristics of desflurane versus halothane for maintenance of anesthesia in pediatric ambulatory patients. Anesthesiology 1994 Feb; 80(2): 298–302
Coté CJ, Liu LMP, Alifimoff JK, et al. Is desflurane (I-653) really faster than halothane? [abstract]. Anesthesiology 1991 Sep; 75 Suppl. 3A: A17
Smith I, Taylor E, White PR Comparison of tracheal extubation in patients deeply anesthetized with desflurane or isoflurane. Anesth Analg 1994 Oct; 79: 642–5
Lee C, Kwan W-F, Tsai S-K, et al. A clinical assessment of desflurane anaesthesia and comparison with isoflurane. Can J Anaesth 1993 Jun; 40_(6): 487–94
Eisenkraft J, Abel M, Bradford C, et al. Safety and efficacy of desflurane in peripheral vascular surgery [abstract]. Anesth Analg 1992 Feb; 74: S84
Smiley RM, Ornstein E, Matteo RS, et al. Desflurane and isoflurane in surgical patients: comparison of emergence time. Anesthesiology 1991 Mar; 74(3): 425–8
Bennett JA, Lingaraju N, Horrow JC, et al. Elderly patients recover more rapidly from desflurane than from isoflurane anesthesia. J Clin Anesth 1992 Sep-Oct; 4: 378–81
McMillan DW, Gold MI, de Lisser EA, et al. Desflurane: how does it compare to isoflurane in elderly patients? [abstract]. Anesth Analg 1991 Feb; 72: S179
van Wandelen RN, Kesecioglu J, Erdmann W. The comparative anaesthetic effects of desflurane versus isoflurane during general anaesthesia in elderly patients [abstract]. In: 9th European Congress of Anaesthesiology. Jerusalem:, 1994: 29
Katoh T, Suguro Y, Ikeda T, et al. Influence of age on awakening concentrations of sevoflurane and isoflurane. Anesth Analg 1993; 76: 348–52
Leavell ME, Monk TG, Lemon DJ, et al. Age does not influence recovery following desflurane anesthesia [abstract]. Anesth Analg 1994; 78: S241
Parsons RS, Jones RM, Wrigley SR, et al. Comparison of desflurane and fentanyl-based anaesthetic techniques for coronary artery bypass surgery. Br J Anaesth 1994 Apr; 72:430–8
Helman JD, Leung JM, Bellows WH, et al. The risk of myocardial ischemia in patients receiving desflurane versus sufentanil anesthesia for coronary artery bypass graft surgery. Anesthesiology 1992 Jul; 77: 47–62
Ross A, Gomez M, Lemmer J, et al. Hemodynamic effects of desflurane versus isoflurane in patients undergoing coronary bypass graft surgery [abstract]. Anesthesiology 1990 Sep; 73 Suppl. 3A: A165
Spiess BD, Jones D, McCarthy RJ, et al. Desflurane vs isoflurane: a comparison of hemodynamics in patients undergoing coronary artery bypass [abstract]. Anesth Analg 1991 Feb; 72: S271
Thomson IR, Bowering JB, Hudson RJ, et al. A comparison of desflurane and isoflurane in patients undergoing coronary artery surgery. Anesthesiology 1991 Nov; 75(5): 776–81
Mahadeviah A, Bennett J, Stewart J, et al. Desflurane versus isoflurane for control of the hemodynamic response to surgical stimulation [abstract]. Anesth Analg 1993 Feb; 76: S235
Abboud TK, Swart F, Zhu J, et al. Desflurane analgesia for vaginal delivery. Acta Anaesthesiol Scand 1995; 39: 259–61
Abboud TK, Zhu J, Richardson M, et al. Desflurane: a new volatile anaesthetic for cesarean section. Maternal and neonatal effects. Acta Anaesthesiol Scand 1995; 39: 723–6
Taylor RH, Lerman J. Induction, maintenance and recovery characteristics of desflurane in infants and children. Can J Anaesth 1992 Jan; 39(1): 6–13
Robinson CP. Desflurane. Drugs Today 1993 Apr-May; 29: 171–81
Hussar DA. New drugs of 1992. Am Pharm 1993 Apr; NS33(4): 20–56
Hartman GS, Kelly RE, Embree PB, et al. Vital capacity rapid inhalation induction with desflurane: the effects of premedi-cation on emergence characteristics and patient acceptance [abstract]. Anesthesiology 1991 Sep; 75 Suppl. 3A: A23
Kelly RE, Hartman GS, Embree PB, et al. Induction of anesthesia with desflurane: a comparison of conventional (C) and vital capacity rapid inhalation induction (VCRII) techniques [abstract]. Anesthesiology 1990 Sep; 73 Suppl. 3A: A51
Hartman GS, Kelly RE, Embree PB, et al. Vital capacity rapid inhalation induction (VCRII) with desflurane [abstract]. Anesthesiology 1990 Sep; 73 Suppl. 3A: A20
Kelly RE, Hartman GS, Embree PB, et al. Inhaled induction and emergence from desflurane anesthesia in the ambulatory surgical patient: the effect of premedication. Anesth Analg 1993 Sep; 77: 540–3
Battito MF, Langner R, Bradley EL. Desflurane (1-653) and isoflurane in surgical patients: comparative hemodynamics and emergence [abstract]. Anesthesiology 1990 Sep; 73 Suppl. 3A: A393
Palazzo MGA, Strunin J. Anaesthesia and emesis. I: etiology. Can J Anaesth 1984 Mar; 31(2): 178–87
Pavlin J, Kallar S, Everett L, et al. Desflurane versus alfentanyl/nitrous oxide (N2O) anesthesia for outpatient lapa-roscopy [abstract]. Anesthesiology 1991 Sep; 75 Suppl. 3A: A11
Zahl K, Prasad K, Mingus M, et al. Desflurane vs isoflurane with or without N2O for outpatient laparoscopy [abstract]. Anesthesiology 1990 Sep; 73 Suppl. 3A: A11
Hellquist E, Bastos M, Jakobsson J. Anaesthesia for arthroscopic day-case surgery. A comparison between desflurane and propofol [abstract]. Br J Anaesth 1995 May; 74 Suppl. 1: A19
McCollum JSC, Milligan KR, Dundee JW. The antiemetic action of propofol. Anaesthesia 1988; 43: 239–40
Oral U, Balcioglu O, Özbeck H, et al. Can propofol be used as an antiemetic? [abstract]. Br J Anaesth 1995 May; 74 Suppl. 1: A22
Felts JA, Poler SM, Spitznagel EL. Nitrous oxide, nausea, and vomiting after outpatient gynecologic surgery. J Clin Anesth 1990 May-Jun; 2: 168–71
Christ DD, Kenna JG, Kammerer W, et al. Enflurane metabolism produces covalently bound liver adducts recognised by antibodies from patients with halothane hepatitis. Anesthesiology 1988; 69: 833–8
Koblin DD. Characteristics and implications of desflurane metabolism and toxicity. Anesth Analg 1992 Oct; 75 Suppl. 4: S10–6
Elliott RH, Strunin L. Hepatotoxicity of volatile anaesthetics. Br J Anaesth 1993 Mar; 70: 339–48
Ray DC, Drummond GB. Halothane hepatitis. Br J Anaesth 1991 Jul; 67: 84–99
Kenna JG, Neuberger JM. Immunopathogenesis and treatment of halothane hepatitis. Clin Immunother 1995; 3(2): 108–24
Zaleski L, Abello D, Gold MI. Desflurane versus isoflurane in patients with chronic hepatic and renal disease. Anesth Analg 1993 Feb; 76: 353–6
Lyons JDM, Murray J, Fee JPH. Hepatic glutathione-S-transferase concentrations (GST) during and after brief desflurane anaesthesia in children [abstract]. Br J Anaesth 1995 May; 74 Suppl. 1: A319
McGrath CJ, Rempel WE, Jesson CR, et al. Malignant hyperthermia-triggering liability of selected inhalant anesthetics in swine. Am J Vet Res 1981 Apr; 42: 604–7
Wedel DJ, Iaizzo PA, Milde JH. Desflurane is a trigger of malignant hyperthermia in susceptible swine. Anesthesiology 1991 Mar; 74(3): 508–12
Wedel DJ, Gammel SA, Milde JH, et al. Delayed onset of. malignant hyperthermia induced by isoflurane and desflurane compared with halothane in susceptible swine. Anesthesiology 1993 Jun; 78(6): 1138–44
Dale O. Drug interactions in anaesthesia: focus on desflurane and sevoflurane. Baillieres Clin Anaesth 1995 March; 9(1): 105–17
Ghouri AF, White PF. Comparative effects of desflurane and isoflurane on vecuronium-induced neuromuscular blockade. J Clin Anesth 1992 Jan-Feb; 4: 34–8
Smiley RM, Ornstein E, Mathews D, et al. A comparison of the effects of desflurane and isoflurane on the action of atracur-ium in man [abstract]. Anesthesiology 1990 Sep; 73 Suppl. 3A: A882
Kelly RE, Belmont MR, Lien CA, et al. A comparison of atracurium (A) requirements during desflurane (D) and isoflurane (I) anesthesia [abstract]. Anesth Analg 1994; 78: S201
Gan TJ, Pressley C, Shlugman D, et al. Determination of the infusion rate of mivacurium to obtain 90% neuromuscular blockade during either isoflurane or desflurane anesthesia [abstract]. Anesthesiology 1994 Sep; 81 Suppl. 3A: A1064
Sarner JB, Cook DR, Davis PJ. The cumulative dose-response relationship of vecuronium in children during halothane-N2O or desflurane-N2O anesthesia [abstract]. Anesth Analg 1993 Feb; 76: S366
Perov S, Nagelhout J, Knoles M, et al. Desflurane prolongation of vecuronium reversal time by neostigmine [abstract]. In: 9th European Congress of Anaesthesiology. Jerusalem:, 1994: 155
Moore MA, Weiskopf RB, Eger El, et al. Arrhythmogenic doses of epinephrine are similar during desflurane or isoflurane anesthesia in humans. Anesthesiology 1993 Nov; 79(5): 943–7
Marti RA, Spahr-Schopfer I, Forster A. Place of sevoflurane and desflurane in pediatric anaesthesia [in French]. Med Hyg 1994 Dec; 52: 2593–8
Andrews JJ, Johnston RV. The new Tec 6 desflurane vaporizer. Anesth Analg 1993 Jun; 76: 1338–41
Andrews JJ, Johnston JRV, Kramer GC. Consequences of misfilling contemporary vaporizers with desflurane. Can J Anaesth 1993 Jan; 40(1): 71–6
Joyce TH, Younker D, Pai UT, et al. Clinical evaluation of the accuracy of TEC6 vaporizer for desflurane [abstract]. Anesth Analg 1993 Feb; 76: S174
Johnston RV, Kramer GC, Arens JF. Desflurane overdose from vaporizer failure (loss of pressurization) [abstract]. Anesthesiology 1991 Sep; 75 Suppl. 3A: A416
Weiskopf RB, Sampson D, Moore MA. The desflurane (Tec 6) vaporizer: design, design considerations and performance evaluation. Br J Anaesth 1994 Apr; 72: 474–9
Graham SG. The desflurane Tec 6 vaporizer. Br J Anaesth 1994 Apr; 72: 470–3
Riddle RT. Tec 6 recall [letter]. Anesthesiology 1994 Sep; 81(3): 791–2
Andrews JJ, Deyo DJ, Johnston RV, et al. Consequences of misfilling isoflurane vaporizers with desflurane [abstract]. Anesth Analg 1994; 78: S7
Merrett KL, Jones RM. Inhalational anaesthetic agents. Br J Hosp Med 1994 Sep; 52(6): 260–3
Miller ED, Greene NM. Waking up to desflurane: the anesthetic for the ’90s? [editorial]. Anesth Analg 1990 Jan; 70: 1–2
Saidman L. The role of desflurane in the practice of anesthesia [editorial]. Anesthesiology 1991 Mar; 74(3): 399–401
Heijke S, Smith G. Quest for the ideal inhalation anaesthetic agent [editorial]. Br J Anaesth 1990 Jan; 64: 3–6
Weiskopf RB, Eger EI. Comparing the costs of inhaled anesthetics. Anesthesiology 1993 Dec; 79(6): 1413–8
Szocik JF, Powell B. A comparison of theoretical vs actual cost of desflurane [abstract]. Anesthesiology 1994 Sep; 81 Suppl. 3A: A536
Hendrickx J, De Wolf AM. Costs of administering desflurane or isoflurane via a closed circuit [letter]. Anesthesiology 1994 Jan; 80(1): 240–2
Nash JA, Stevens WC, Au Y-H. Desflurane and isoflurane induction rate using a closed circuit system [abstract]. Anesthesiology 1994 Sep; 81 Suppl. 3A: A369
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: R.R. Bartkowski, Department of Anesthesiology, Jefferson Medical College, Thomas Jefferson University, Philadelphia, Pennsylvania, USA; AM. Breckenridge, Department of Pharmacology and Therapeutics, The University of Liverpool, Liverpool, England; P.J. Davis, Department of Anesthesiology and Critical Care Medicine, Children’s Hospital of Pittsburgh, University of Pittsburgh, Pittsburgh, Pennsylvania, USA; C. Diefenbach, Klinik für Anaesthesiologie und Operative Intensivmedizin der Universität zu Köln, Cologne, Germany; E.I. Eger, Department of Anesthesia, University of California, San Francisco, California, USA; P. Flynn, Anaesthetics Unit, The Royal London Hospital, London, England; M.I. Gold, Department of Anesthesiology, University of Miami School of Medicine, Miami, Florida, USA; J.M. Hunter, University Department of Anaesthesia, Royal Liverpool University Hospital, Liverpool, England; R.M. Jones, Department of Anaesthetics, St Mary’s Hospital Medical School, Imperial College of Medicine, London, England; J. Lerman, Department of Anaesthesia, The Hospital for Sick Children, University of Toronto Faculty of Medicine, Toronto, Ontario, Canada; C.A. Lien, Department of Anesthesiology, The New York Hospital-Cornell University Medical Center, New York, New York, USA; S. Oshita, Department of Anesthesiology, Yamaguchi University Hospital, Ube, Yamaguchi, Japan; D.C. Warltier, Department of Anesthesiology, Medical College of Wisconsin, Milwaukee, Wisconsin, USA.
An erratum to this article is available at http://dx.doi.org/10.1007/BF03259621.
Rights and permissions
About this article
Cite this article
Patel, S.S., Goa, K.L. Desflurane. Drugs 50, 742–767 (1995). https://doi.org/10.2165/00003495-199550040-00010
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199550040-00010