Abstract
Migraine and depression coincide in some 20–30% of patients. Although antidepressants (namely tricyclics) are not considered as first-line prophylactic compounds in patients with migraine alone, several clinical trials support a remarkable benefit in the treatment of migraine and related headache disorders. However, treatment with one antidepressant alone often does not suffice to treat both disorders effectively. Therefore, combinations of classical antidepressants with both newer antidepressants and established prophylactic drugs (e.g. β-adrenergic receptor antagonists [β-blockers], topiramate and sodium valproate) are required. In addition, acute attack medication (such as triptans, ergotamines or analgesics) is regularly combined with the preventive medication, thus requiring elaborate knowledge about the complex network of potential interactions and contraindications. Fear of potentially serious interactions can frequently lead to insufficient treatment of both underlying disorders, with an enormous impact on the patient’s life. Pathophysiologically, multiple neurotransmitters have been attributed an important role in the aetiology of migraine (mainly serotonin and calcitonin gene-related peptide) and depression (among others, serotonin, dopamine and noradrenaline [norepinephrine]). Most drugs used to treat both disorders influence at least one of these transmitter systems, such as classical tricyclics. This review discusses the efficacy of antidepressants in migraine prevention. In addition, recommended combinations in patients with concomitant depression and migraine are presented with regard to their proposed pharmacological mechanism of action and their potential interactions.







Similar content being viewed by others
References
Headache Classification Committee of the HIS. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 2004; 24 Suppl. 1: 24–36
Kelman L. The place of osmophobia and taste abnormalities in migraine classification: a tertiary care study of 1237 patients. Cephalalgia 2004; 24(11): 940–6
Kelman L. The aura: a tertiary care study of 952 migraine patients. Cephalalgia 2004; 24(9): 728–34
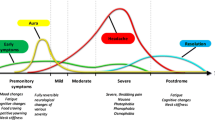
Silberstein SD, Saper JR, Freitag FG. Migraine: diagnosis and treatment. In: Silberstein SD, Lipton RB, Dalessio DJ, editors. Wolff’s headache and other head pain. 7th ed. New York: Oxford University Press, 2001: 121–238
Evers S, Afra J, Frese A, et al. EFNS guideline on the drug treatment of migraine: report of an EFNS task force. Eur J Neurol 2006; 13(6): 560–72
Carod-Artal FJ, Ribeiro LD, Braga H, et al. Prevalence of patent foramen ovale in migraine patients with and without aura compared with stroke patients: a transcranial Doppler study. Cephalalgia 2006; 26(8): 934–9
Gudmundsson LS, Thorgeirsson G, Sigfusson N, et al. Migraine patients have lower systolic but higher diastolic blood pressure compared with controls in a population-based study of 21 537 subjects: the Reykjavik Study. Cephalalgia 2006; 26(4): 436–44
Ifergane G, Buskila D, Simiseshvely N, et al. Prevalence of fibromyalgia syndrome in migraine patients. Cephalalgia 2006; 26(4): 451–6
Wolff HG. Headache and other head pain. 2nd ed. New York: Oxford University Press, 1963
Selby G, Lance JW. Observations on 500 cases of migraine and allied vascular headache. J Neurol Neurosurg Psychiatr 1960; 23(1): 23–32
Kashiwagi T, Wetzel RD, McClure JN. Headache and psychiatric disorders. Dis Nerv Syst 1972; 33(10): 659–63
Couch JR, Ziegler DK, Hassanein RS. Evaluation of relationship between migraine headache and depression. Headache 1975; 15(1): 41–50
Couch JR, Hassanein RS. Amitriptyline in migraine prophylaxis. Arch Neurol 1979; 36(11): 695–9
Breslau N, Davis GC, Andreski P. Migraine disorders, and suicide attempts: an epidemiologic study of young adults. Psychiatry Res 1991; 37(1): 11–23
Merikangas KR, Angst J, Isler H. Migraine and psychopathology: results of the Zurich cohort study of young adults. Arch Gen Psychiatry 1990; 47(9): 849–53
Molgat CV, Patten SB. Comorbidity of major depression and migraine: a Canadian population-based study. Can J Psychiatry 2005; 50(13): 832–7
Radat F, Swendsen J. Psychiatric comorbidity in migraine: a review. Cephalalgia 2005; 25(3): 165–78
Hamelsky SW, Lipton RB. Psychiatric comorbidity of migraine. Headache 2006; 46(9): 1327–33
Kalaydjian A, Merikangas K. Physical and mental comorbidity of headache in a nationally representative sample of US adults. Psychosom Med 2008; 70(7): 773–80
Fiane I, Haugland ME, Stovner LJ, et al. Sick leave is related to frequencies of migraine and non-migrainous headache: the HUNT study. Cephalalgia 2006; 26(8): 960–7
Breslau N, Lipton RB, Stewart WF, et al. Comorbidity of migraine and depression: investigating potential etiology and prognosis. Neurology 2003; 60(8): 1308–12
Tietjen GE, Herial NA, Hardgrove J, et al. Migraine comorbidity constellations. Headache 2007; 47(6): 857–65
Lepine JP, Briley M. The epidemiology of pain in depression. Hum Psychopharmacol 2004; 19: 3–7
Goadsby PJ, Lipton RB, Ferrari MD. Migraine: current understanding and treatment. N Engl J Med 2002; 346(4): 257–70
Goadsby PJ. Migraine pathophysiology. Headache 2005; 45: 14–24
Moskowitz MA. Genes proteases, cortical spreading depression and migraine: impact on pathophysiology and treatment. Funct Neurol 2007; 22(3): 133–6
Durham PL. Inhibition of calcitonin gene-related peptide function: a promising strategy for treating migraine. Headache 2008; 48(8): 1269–75
Goadsby PJ, Edvinsson L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann Neurol 1993; 33(1): 48–56
Rudolf K, Eberlein W, Engel W, et al. Development of human calcitonin gene-related peptide (CGRP) receptor antagonists: 1, potent and selective small molecule CGRP antagonists — 1-[N-2-[3,5-dibromo-N-[[4-(3,4-dihydro-2(1H)-oxoquinazolin-3-yl)-1-piperidinyl]carbonyl]-D-tyrosyl]-L-lysyl]-4-(4-pyridinyl)piperazine: the first CGRP antagonist for clinical trials in acute migraine. J Med Chem 2005; 48(19): 5921–31
Olesen J, Diener H, Husstedt IW, et al. Calcitonin gene-related peptide receptor antagonist BIBN4096BSfor the acute treatment of migraine. NEJM 2004; 350(11): 1104–10
Ho TW, Mannix LK, Fan X, et al. Randomized controlled trial of an oral CGRP receptor antagonist, MK-0974, in acute treatment of migraine. Neurology 2008; 70(16): 1304–12
Degnan AP, Chaturvedula PV, Conway CM, et al. Discovery of (R)-4-(8-fluoro-2-oxo-1,2-dihydroquinazolin-3(4H)-yl)-N-(3-(7-methyl-1H-indazol-5-yl)-1-oxo-1-(4-(piperidin-1-yl) piperidin-1-yl)propan-2-yl)piperidine-1-carboxamide (BMS-694153): a potent antagonist of the human calcitonin gene-related peptide receptor for migraine with rapid and efficient intranasal exposure. J Med Chem 2008; 51(16): 4858–61
Burstein R, Cutrer MF, Yarnitsky D. The development of cutaneous allodynia during a migraine attack: clinical evidence for the sequential recruitment of spinal and supraspinal nociceptive neurons in migraine. Brain 2000; 123: 1703–9
Peroutka SJ. Drugs effective the therapy of migraine. In: Hardman JG, Limbird LE, Molinoff PB, et al., editors. Goodman & Gilman’s the pharmacological basis of therapeutics. 9th ed. New York: McGraw-Hill, 1996: 488–502
Ferrari MD, Saxena PR. On serotonin and migraine: a clinical and pharmacological review. Cephalalgia 1993; 13(3): 151–65
Peroutka SJ. 5-Hydroxytryptamine receptor subtypes: molecular, biochemical physiological characterization. Trends Neurosci 1988; 11(11): 496–500
Barnes NM, Sharp T. A review of central 5-HT receptors and their function. Neuropharmacology 1999; 38(8): 1083–152
Watling KJ. The RBI handbook of receptor classification and signal transduction. 3rd ed. Natick (MA): Sigma-Aldrich Research Biochemicals Inc., 1998
Sicuteri F. Prophylactic and therapeutic properties of 1-methyl-lysergic acid butanolamide in migraine. Int Arch Allergy Appl Immunol 1959; 15(4–5): 300–7
Sicuteri F, Anselmi B, Testi A. Biochemical investigations in headache-increase in hydroxyindoleacetic acid excretion during migraine attacks. Int Arch Allergy Appl Immunol 1961; 19(1): 55
Lance JW. Advances in biology and pharmacology of headache. Neurology 1993; 43(6): 5
Hamel E. Serotonin and migraine: biology and clinical implications. Cephalalgia 2007; 27(11): 1295–300
Benkert O, Hippius H. Kompendium der Psychiatrischen Pharmakotherapie. Berlin: Springer, 2000
Pederson V. Psychotropics 2002/2003. Allerod: Lundbeck Institute, 2003
Bánk J. A comparative study of amitriptyline and fluvoxamine in migraine prophylaxis. Headache 1994; 34(8): 476–8
Lance JW, Curran DA. Treatment of chronic tension headache. Lancet 1964; 1(734): 1236–9
Gomersall JD, Stuart A. Amitriptyline in migraine prophylaxis: changes in pattern of attacks during a controlled clinical trial. J Neurol Neurosurg Psychiatry 1973; 36(4): 684–90
Ziegler DK, Hurwitz A, Hassanein RS, et al. Migraine prophylaxis: a comparison of propranolol and amitriptyline. Arch Neurol 1987; 44(5): 486–9
Ziegler DK, Hurwitz A, Preskorn S, et al. Propranolol and amitriptyline in prophylaxis of migraine: pharmacokinetic and therapeutic effects. Arch Neurol 1993; 50(8): 825–30
Snow V, Weiss K, Wall EM, et al., American Academy of Family Physicians; American College of Physicians-American Society of Internal Medicine. Pharmacologic management of acute attacks of migraine and prevention ofmigraine headache. Ann Intern Med 2002; 137(10): 840–9
Silberstein SD. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000; 55(6): 754–62
Krymchantowski AV, Silva MT, Barbosa JS, et al. Amitriptyline versus amitriptyline combined with fluoxetine in the preventative treatment of transformed migraine: a double-blind study. Headache 2002; 42(6): 510–4
Rampello L, Alvano A, Chiechio S, et al. Evaluation of the prophylactic efficacy of amitriptyline and citalopram, alone or in combination, in patients with comorbidity of depression, migraine, and tension-type headache. Neuropsychobiology 2004; 50(4): 322–8
Evers S, Mylecharane EJ. Nonsteroidal anti-inflammatory and miscellaneous drugs in migraine prophylaxis. In: Olesen J, Goadsby PJ, Ramadan NM, et al., editors. The headaches. 3rd edition. Philadelphia (PA): Lipincott Williams & Wilkins, 2006: 560
Hershey AD, Powers SW, Bentti AL, et al. Effectiveness of amitriptyline in the prophylactic management of childhood headaches. Headache 2000; 40(7): 539–49
Lewis DW, Diamond S, Scott D, et al. Prophylactic treatment of pediatric migraine. Headache 2004; 44(3): 230–7
Victor S, Ryan SW. Drugs for preventing migraine headaches in children. Cochrane Database Syst Rev 2003; (4): CD002761
Berilgen MS, Bulut S, Gonen M, et al. Comparison of the effects of amitriptyline and flunarizine on weight gain and serum leptin, C peptide and insulin levels when used as migraine preventive treatment. Cephalalgia 2005; 25(11): 1048–53
Koch HJ. Steady state plasma levels during antidepressant therapy with amitriptyline and amitriptylinoxide. Israel J Psychiatry Rel Sci 1990; 27(1): 48–53
Koch HJ. Alteration of the ECG and blood pressure during treatment with amitriptyline and amitriptylinoxide: a study with plasma levels. Irish J Psychiatry 1990; 11(2): 12–6
Moja PL, Cusi C, Sterzi RR, et al. Selective serotonin re-uptake inhibitors (SSRIs) for preventing migraine and tension-type headaches. Cochrane Database Syst Rev 2005; (3): CD002919
Gray AM, Pache DM, Sewell RDE. Do alpha(2)-adrenoceptors play an integral role in the antinociceptive mechanism of action of antidepressant compounds? Eur J Pharmacol 1999; 378(2): 161–8
Punay NC, Couch JR. Antidepressants in the treatment of migraine headache. Curr Pain Headache Rep 2003; 7(1): 51–4
Koch HJ. Relation between plasma levels and ECG after antidepressant treatment with amitriptyline and amitriptylinoxide [thesis]. Mainz: Medical Faculty, Johannes Gutenberg University, 1986
Shin JG, Park JY, Kim MJ, et al. Inhibitory effects of tricyclic antidepressants (TCAs) on human cytochrome P450 enzymes in vitro: mechanism of drug interaction between TCAs and phenytoin. Drug Metab Dispos 2002; 30(10): 1102–7
Wong SL, Cavanaugh J, Shi H, et al. Effects of divalproex sodium on amitriptyline and nortriptyline pharmacokinetics. Clin Pharmacol Ther 1996; 60(1): 48–53
Langohr HD, Gerber WD, Koletzki E, et al. Clomipramine and metoprolol in migraine prophylaxis: a double-blind crossover study. Headache 1985; 25(2): 107–13
Noone JF. Clomipramine in the prevention of migraine. J Int Med Res 1980; 8 Suppl. 3: 49–52
Mørland TJ, Storli OV, Mogstad TE. Doxepin in the prophylactic treatment of mixed “vascular” and tension headache. Headache 1979; 19(7): 382–3
Elser JM, Woody RC. Migraine headache in the infant and young-child. Headache 1990; 30(6): 366–8
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th edition, text revision. Washington, DC: American Psychiatric Association, 2000
Landy S, McGinnis J, Curlin D, et al. Selective serotonin reuptake inhibitors for migraine prophylaxis. Headache 1999; 39(1): 28–32
Hays P. Paroxetine prevents migraines. J Clin Psychiatry 1997; 58(1): 30–1
Black KJ, Sheline YI. Paroxetine as migraine prophylaxis. J Clin Psychiatry 1995; 56(7):330–1
Zeeberg I, Orholm M, Nielsen JD, et al. Femoxetine in the prophylaxis of migraine: a randomised comparison with placebo. Acta Neurol Scand 1981; 64(6): 452–9
Orholm M, Honoré PF, Zeeberg I. A randomized general practice group-comparative study of femoxetine and placebo in the prophylaxis of migraine. Acta Neurol Scand 1986; 74(3): 235–9
Stankewitz A, May A. Cortical excitability and migraine. Cephalalgia 2007; 27(12): 1454–6
Ozkul Y, Bozlar S. Effects of fluoxetine on habituation of pattern reversal visually evoked potentials in migraine prophylaxis. Headache 2002; 32(7): 582–7
Oguzhanoglu A, Sahiner T, Kurt T, et al. Use of amitriptyline and fluoxetine in prophylaxis of migraine and tension-type headaches. Cephalalgia 1999; 19(5): 531–2
Saper JR, Silberstein SD, Lake III AE, et al. Double-blind trial of fluoxetine: chronic daily headache and migraine. Headache 1994; 34(9): 497–502
Adly C, Straumanis J, Chesson A. Fluoxetine prophylaxis of migraine. Headache 1992; 32(2): 101–4
d’Amato CC, Pizza V, Marmolo T, et al. Fluoxetine for migraine prophylaxis: a double-blind trial. Headache 1999; 39(10): 716–9
Steiner TJ, Ahmed F, Findley LJ, et al. S-Fluoxetine in the prophylaxis of migraine: a phase II double-blind randomized placebo-controlled study. Cephalalgia 1998; 18(5): 283–6
Bickel A, Kornhuber J, Maihofner C, et al. Exacerbation of migraine attacks during treatment with the selective serotonin reuptake inhibitor sertraline: a case report. Pharmacopsychiatry 2005; 38(6): 327–8
Munera PA, Goldstein A. Migraine and sertraline. J Am Acad Child Adolesc Psychiatry 2001; 40(10): 1125–6
Delva NJ, Horgan SA, Hawken ER. Valproate prophylaxis for migraine induced by selective serotonin reuptake inhibitors. Headache 2000; 40(3): 248–51
Levy E, Margolese HC. Migraine headache prophylaxis and treatment with low-dose mirtazapine. Int Clin Psychopharmacol 2003; 18(5): 301–3
Brannon GE, Rolland PD, Gary JM. Use of mirtazapine as prophylactic treatment for migraine headache. Psychosomatics 2000; 41(2): 153–4
Gorman JM. Mirtazapine: clinical overview. J Clin Psychiatry 1999; 60 Suppl. 17: 9–13; discussion 46-8
WebMD Inc. RxList: the internet drug index [online]. Available from URL: http://www.rxlist.com/script/main/hp.asp [Accessed 2008 Sep 2]
Monro P, Swade C, Coppen A. Mianserin in the prophylaxis of migraine: a double-blind study. Acta Psychiatr Scand 1985; 320 Suppl.: 98–103
Martucci N, Manna V, Porto C, et al. Migraine and the noradrenergic control of vasomotricity: a study with alpha-2 stimulant and alpha-2 blocker drugs. Headache 1985; 25(2): 95–100
Saper JR, Lake AE, Tepper SJ. Nefazodone for chronic daily headache prophylaxis: an open-label study. Headache 2001; 41(5): 465–74
Greene DS, Barbhaiya RH. Clinical pharmacokinetics of nefazodone. Clin Pharmacokinet 1997; 33(4): 260–75
Choi S. Nefazodone (serzone) withdrawn becuase of hepatotoxicity. CMAJ 2003; 169(11): 1187
FDA/Center for Drug Evaluation and Research. Drugs@ FDA [online]. Available from URL: http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction = Search. Overview&DrugName = NEFAZODONE%20HYDRO CHLORIDE [Accessed 2008 Sep 2]
Spielmans GI. Duloxetine does not relieve painful physical symptoms in depression: a meta-analysis. Psychother Psychosom 2008; 77(1): 12–6
Taylor AP, Adelman JU, Freeman MC. Efficacy of duloxetine as a migraine preventive medication: possible predictors of response in a retrospective chart review. Headache 2007; 47(8): 1200–3
Volpe FM. An 8-week, open-label trial of duloxetine for comorbid major depressive disorder and chronic headache. J Clin Psychiatry. Epub 2008 Jul 15
Nascimento ED. Prophylaxis of migraine: open study with venlafaxine in 42 patients. Arq Neuropsiquiatr 1998; 56(4): 744–6
Adelman LC, Adelman JU, Von Seggern R, et al. Venlafaxine extended release (XR) for the prophylaxis of migraine and tension-type headache: a retrospective study in a clinical setting. Headache 2000; 40(7): 572–80
Bulut S, Berilgen MS, Baran A, et al. Venlafaxine versus amitriptyline in the prophylactic treatment of migraine: randomized, double-blind, crossover study. Clin Neurol Neurosurg 2004; 107(1): 44–8
Ozyalcin SN, Talu GK, Kiziltan E, et al. The efficacy and safety of venlafaxine in the prophylaxis of migraine. Headache 2005; 45(2): 144–52
Diamond S, Pepper BJ, Diamond ML, et al. Serotonin syndrome induced by transitioning from phenelzine to venlafaxine: four patient reports. Neurology 1998; 51(1): 274–6
World Health Organization. Safety of venlafaxine. In: WHO Drug Information, vol 12, no 2. Geneva: WHO, 1998: 82
Ferrari A, Sternieri E, Ferraris E, et al. Emerging problems in the pharmacology of migraine: interactions between triptans and drugs for prophylaxis. Pharmacol Res 2003; 48(1): 1–9
Anthony M, Lance JW. Monoamine oxidase inhibition in the treatment of migraine. Arch Neurol 1969; 21(3): 263–8
Mann AM, Laing WA. Tranylcypromine cephalgia. Can Med Assoc J 1963; 89: 1115–8
Meienberg O, Amsler F. Moclobemide in the prophylactic treatment of migraine: a retrospective analysis of 44 cases. Eur Neurol 1996; 36(2): 109–10
Meienberg O, Amsler F. Preventive treatment of migraine and chronic tension headache with moclobemide. Praxis (Bern 1994) 1997; 86(27–28): 1107–12
Yoon MS, Savidou I, Diener HC, et al. Evidence-based medicine in migraine prevention. Expert Rev Neurother 2005; 5(3): 333–41
Fuseau E, Petricoul O, Moore KH, et al. Clinical pharmacokinetics of intranasal sumatriptan. Clin Pharmacokinet 2002; 41(11): 801–11
Brewerton TD, Murphy DL, Mueller EA, et al. Induction of migrainelike headaches by the serotonin agonist m-chlorophenylpiperazine. Clin Pharmacol Ther 1988; 43(6): 605–9
Van Haarst AD, Van Gerven JM, Cohen AF, et al. The effects of moclobemide on the pharmacokinetics of the 5-HT1B/1D agonist rizatriptan in healthy volunteers. Br J Clin Pharmacol 1999; 48(2): 190–6
Buchan P, Wade A, Ward C, et al. Frovatriptan: a review of drug-drug interactions. Headache 2002; 42 Suppl. 2: 63–73
Fleishaker JC, Ryan KK, Jansat JM, et al. Effect of MAO-A inhibition on the pharmacokinetics of almotriptan, an antimigraine agent in humans. Br J Clin Pharmacol 2001; 51(5): 437–41
Rolan P. Potential drug interactions with the novel antimigraine compound zolmitriptan (Zomig, 311C90). Cephalalgia 1997; 17 Suppl. 18: 21–7
Merikangas KR, Stevens DE, Merikangas JR, et al. Tyramine conjugation deficit in migraine, tension-type headache, and depression. Biol Psychiatry 1995; 38(11): 730–6
Goodman JF. Treatment of headache with bupropion [letter]. Headache 1997; 37(4): 256
Pinsker W. Treatment of headache with bupropion [letter]. Headache 1998; 38(1): 58
Akerman S, Goadsby PJ. Dopamine and migraine: biology and clinical implications. Cephalalgia 2007; 27(11): 1308–14
Modell JG, Katholi CR, Modell JD, et al. Comparative sexual side effects of bupropion, fluoxetine, paroxetine, and sertraline. Clin Pharmacol Ther 1997; 61(4): 476–87
Jacobs H. A trial of opipramol in the treatment of migraine. J Neurol Neurosurg Psychiatry 1972; 35(4): 500–4
Battistella PA, Ruffilli R, Cernetti R, et al. A placebo-controlled crossover trial using trazodone in pediatric migraine. Headache 1993; 33(1): 36–9
Pies R. Trazodone and intractable headaches. J Clin Psychiatry 1983; 44(8): 317
Maes M, Vandoolaeghe E, Desnyder R. Efficacy of treatment with trazodone in combination with pindolol or fluoxetine in major depression. J Affect Disord 1996; 41(3): 201–10
Costa E, Silva JA, Ruschel SI, et al. Placebo-controlled study of tianeptine in major depressive episodes. Neuropsychobiology 1997; 35(1): 24–9
Ferrari A, Ottani A, Bertolini A, et al. Adverse reactions related to drugs for headache treatment: clinical impact. Eur J Clin Pharmacol 2005; 60(12): 893–900
Spina E, Santoro V, D’Arrigo C. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther 2008; 30(7): 1206–27
FDA/Center for Drug Evaluation and Research. Combined use of 5-hydroxytryptamine receptor agonists (triptans), selective serotonin reuptake Inhibitors (SSRIs) or selective serotonin/norepinephrine reuptake inhibitors (SNRIs) may result in life-threatening serotonin syndrome [online]. Available from URL: http://www.fda.gov/Cder/Drug/advisory/SSRI_SS200607.htm [Accessed 2008 Sep 5]
Evans RW. Triptans and serotonin syndrome. Cephalalgia 2008; 28(5): 573–4; author reply 574-5
Sternbach H. The serotonin syndrome. Am J Psychiatry 1991; 148(6): 705–13
Dunkley EJ, Isbister GK, Sibbritt D, et al. The Hunter serotonin toxicity criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM 2003; 96(9): 635–42
Shapiro RE, Tepper SJ. The serotonin syndrome, triptans, and the potential for drug-drug interactions. Headache 2007; 47(2): 266–9
Putnam GP, O’Quinn S, Bolden-Watson CP, et al. Migraine polypharmacy and the tolerability of sumatriptan: a large-scale, prospective study. Cephalalgia 1999; 19(7): 668–75
Dahlof CG, Boes-Hansen S, Cederberg CG, et al. How does sumatriptan nasal spray perform in clinical practice? Cephalalgia 1998; 18(5): 278–82
Fleishaker JC, Herman BD, Carel BJ, et al. Interaction between ketoconazole and almotriptan in healthy volunteers. J Clin Pharmacol 2003; 43(4): 423–7
Mathew NT, Tietjen GE, Lucker C. Serotonin syndrome complicating migraine pharmacotherapy. Cephalalgia 1996; 16(5): 323–7
Hewer W. Akut- und Notfallsituationen durch unerwünschte Arzneimittelwirkungen (UAW). In: Hewer R, Rössler W, editors. Das Notfallpsychiatrie Buch. München: Urban Schwarzenberg, 1998: 498–534
Yap YG, Camm AJ. Drug induced QT prolongation and torsade de pointes. Heart 2003; 89(11): 1363–72
Arizona Center for Education and Research on Therapeutics. QT drug lists [online]. Available from URL: http://www.azcert.org/medical-pros/drug-lists/drug-lists.cfm [Accessed 2008 Sep 2]
Witchel HJ, Hancox JC, Nutt DJ. Psychotropic drugs, cardiac arrhythmia, and sudden death. J Clin Psychopharmacol 2003; 23(1): 58–77
Bareggi SR, Mundo E, Dell’Osso B, et al. The use of escitalopram beyond major depression: pharmacological aspects, efficacy and tolerability in anxiety disorders. Expert Opin Drug Metab Toxicol 2007; 3(5): 741–53
Mula M, Sander JW. Negative effects of antiepileptic drugs on mood in patients with epilepsy. Drug Saf 2007; 30(7): 555–67
Nickel C, Lahmann C, Tritt K, et al. Topiramate in treatment of depressive and anger symptoms in female depressive patients: a randomized, double-blind, placebo-controlled study. J Affect Disord 2005; 87(2–3): 243–52
Keskinbora K, Aydinli I. A double-blind randomized controlled trial of topiramate and amitriptyline either alone or in combination for the prevention of migraine. Clin Neurol Neurosurg 2008; 110(10): 979–84
Keller S, Frishman WH. Neuropsychiatric effects of cardiovascular drug therapy. Cardiol Rev 2003; 11(2): 73–93
Gerstman BB, Jolson HM, Bauer M, et al. The incidence of depression in new users of beta-blockers and selected antihypertensives. J Clin Epidemiol 1996; 49(7): 809–15
Toda N, Tfelt-Hansen P. Calacim antagonists in migraine prophylaxis. In: Dlesen J, Goadsby PJ, Ramadan et al., editors. The headaches. 3rd edition. Philadelphia (PA): Lippincott Williams & Wilkins, 2006: 539–44
Keam SJ, Goa KL, Figgitt DP. Almotriptan: a review of its use in migraine. Drugs 2002; 62(2): 387–414
Fava M. Weight gain and antidepressants. J Clin Psychiatry 2000; 61 Suppl. 11: 37–41
Krymchantowski A, Tavares C. Weight variations in patients receiving topiramate migraine prophylaxis in a tertiary care setting. Med Gen Med 2004; 6(3): 48
Altman DG, Schulz KF, Moher D, et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 2001; 134(8): 663–94
Tfelt-Hansen P, Block G, Dahlof C, et al. Guidelines for controlled trials of drugs in migraine. 2nd ed. Cephalalgia 2000; 20(9): 765–86
American Academy of Neurology (AAN). Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology [online]. Available from URL: http://www.neurology.org/cgi/reprint/55/6/754.pdf [Accessed 2008 Dec 22]
Deutsche Gesellschaft für Neurologie (DGN). Therapie der Migräneattacke und Migŕáneprophylaxe [online]. Available from URL: http://www.dgn.org/images/stories/dgn/leitlinien/migraene.pdf [Accessed 2008 Oct 4]
Johnson ES, Kadam NP, Hylands DM, et al. Efficacy of feverfew as prophylactic treatment of migraine. BMJ (Clin Res Ed) 1985; 291(6495): 569–73
Grossmann M, Schmidramsl H. An extract of Petasites hybridus is effective in the prophylaxis of migraine. Int J Clin Pharmacol Ther 2000; 38(9): 430–5
Rossi P, Di Lorenzo G, Malpezzi MG, et al. Prevalence, pattern and predictors of use of complementary and alternative medicine (CAM) in migraine patients attending a headache clinic in Italy. Cephalalgia 2005; 25(7): 493–506
Hu Z, Yang X, Ho PC, et al. Herb-drug interactions: a literature review. Drugs 2005; 65(9): 1239–82
Kalin P. The common butterbur (Petasites hybridus): portrait of a medicinal herb. Forsch Komplementarmed Klass Naturheilkd 2003; 10 Suppl. 1: 41–4
Abebe W. Herbal medication: potential for adverse interactions with analgesic drugs. J Clin Pharm Ther 2002; 27(6): 391–401
Busch V, Gaul C. Exercise in migraine therapy: is there any evidence for efficacy? A critical review. Headache 2008; 48(6): 890–9
Campbell JK, Penzien DB, Wall EM, et al. Headache Consortium. Evidenced-based guidelines for migraine headache: behavioral and physical treatments [online]. Available from URL: http://www.aan.com/professionals/practice/pdfs/gl0089.pdf [Accessed 2008 Oct 4]
Strohle A. Physical activity, exercise, depression and anxiety disorders. J Neural Transm. Epub 2008 Aug 23
Boerlin HL, Gitlin MJ, Zoellner LA, et al. Bipolar depression and antidepressant-induced mania: a naturalistic study. J Clin Psychiatry 1998; 59(7): 374–9
Sachs GS, Gardner-Schuster EE. Adjunctive treatment of acute mania: a clinical overview. Acta Psychiatr Scand 2007; 434 Suppl.: 27–34
Acknowledgements
No sources of funding were used in the preparation of this article. Dr Jürgens has received honoraria from GlaxoSmithKline and grants from Merck Sharpe & Dohme. Dr Koch has no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koch, H.J., Jürgens, T.P. Antidepressants in Long-Term Migraine Prevention. Drugs 69, 1–19 (2009). https://doi.org/10.2165/00003495-200969010-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200969010-00001