Abstract
Background
Intraoperative parathyroid hormone (ioPTH) monitoring (IPM) is vital to minimally invasive parathyroidectomy. Techniques vary in assay sampling, potentially affecting predictive accuracy of operative success. Initial guidelines were established using peripheral sites, but central sites may be preferred or necessary when peripheral access is not feasible. We hypothesize that changing collection sites from preexcision peripheral sites to postexcision central sites would not affect IPM accuracy.
Methods
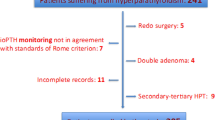
Analysis of 64 consecutive patients who underwent parathyroidectomy for primary hyperparathyroidism was undertaken. PTH assays were collected simultaneously from a peripheral vein (PV) and central vein (CV) preexcision and at a 10-min interval after initial parathyroid excision. IPM success was defined as PTH decrease ≥50% 10 min after initial excision. Predictive accuracy was determined by the need to resect another abnormal gland and biochemical normalization in the postoperative clinic. Receiver operating characteristic (ROC) method with area under the curve (AUC) compared diagnostic accuracy of different assay approaches.
Results
Centrally, a statistically higher mean pre- and postexcision ioPTH of 391 pg/ml and 58 pg/ml was found compared with peripheral means of 156 pg/ml and 49 pg/ml, respectively (p < 0.001). The AUC when changing from a PV preexcision to a CV postexcision ioPTH was 0.89, comparable to AUC for peripheral or central assay collections alone (AUC = 0.83 and 0.85, respectively).
Conclusions
This study suggests that altering collection sites does not alter assay validity. In cases where peripheral sampling is compromised, changing from a peripheral to central sites will not likely alter the predictive accuracy of IPM significantly.

Similar content being viewed by others
References
Clark OH. Surgical treatment of primary hyperparathyroidism. Adv Endocrinol Metab. 1995;6:1–16.
Libutti SK, Alexander HR, Bartlett DL, et al. Kinetic analysis of the rapid intraoperative parathyroid hormone assay in patients during operation for hyperparathyroidism. Surgery. 1999;126(6):1145–50; discussion 1150–1.
Bieglmayer C, Prager G, Niederle B. Kinetic analyses of parathyroid hormone clearance as measured by three rapid immunoassays during parathyroidectomy. Clin Chem. 2002;48(10):1731–8.
Irvin GL 3rd, Dembrow VD, Prudhomme DL. Clinical usefulness of an intraoperative “quick parathyroid hormone” assay. Surgery. 1993;114(6):1019–22; discussion 1022–3.
Chiu B, Sturgeon C, Angelos P. Which intraoperative parathyroid hormone assay criterion best predicts operative success? A study of 352 consecutive patients. Arch Surg. 2006;141(5):483–7; discussion 487–8.
Carneiro DM, Solorzano CC, Nader MC, et al. Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: which criterion is the most accurate? Surgery. 2003;134(6):973–9; discussion 979–81.
Gordon LL, Snyder WH 3rd, Wians F Jr, et al. The validity of quick intraoperative parathyroid hormone assay: an evaluation in seventy-two patients based on gross morphologic criteria. Surgery. 1999;126(6):1030–5.
Woodrum DT, Saunders BD, England BG, et al. The influence of sample site on intraoperative PTH monitoring during parathyroidectomy. Surgery. 2004;136(6):1169–75.
Beyer TD, Chen E, Ata A, et al. A prospective evaluation of the effect of sample collection site on intraoperative parathormone monitoring during parathyroidectomy. Surgery. 2008;144(4):504–9; discussion 509–10.
Broome JT, Schrager JJ, Bilheimer D, et al. Central venous sampling for intraoperative parathyroid hormone monitoring: are peripheral guidelines applicable? Am Surg. 2007;73(7):712–6.
Urquhart AC, Wiley C. Arterial and venous parathyroid hormone levels in minimally invasive surgery. Arch Otolaryngol Head Neck Surg. 2005;131(2):137–9.
Pepe MS. Receiver operating characteristics methodology. J Am Stat Assoc. 2000;95(449):308–11.
Zweig MH, Campbell G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem. 1993;39(8):561–77.
Disclosures
No financial disclosures associated with producing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdel-Misih, S.R.Z., Broome, J.T., Li, X. et al. Changing Intraoperative Parathyroid Hormone Collection Sites from Peripheral to Central Does Not Affect Predictive Accuracy during Minimally Invasive Parathyroidectomy. Ann Surg Oncol 18, 771–776 (2011). https://doi.org/10.1245/s10434-010-1375-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-010-1375-7