Abstract
High tidal volume (VT) ventilation plays a key role in ventilator induced lung injury and bronchopulmonary dysplasia. However, little is known about the effect of high VT on expression of growth factors that are critical to lung development. In a previous study, we demonstrated that connective tissue growth factor (CTGF) inhibits branching morphogenesis. In this study, we investigated the effect of high VT on CTGF expression in newborn rat lungs. Newborn rats were ventilated with normal VT (10 mL/kg) or high VT (25 mL/kg) for 6 h. Nonventilated animals served as controls. We found that high VT upregulated CTGF expression. To identify the potential signaling pathways mediating high VT induction of CTGF, newborn rats were ventilated with high VT for 1 or 3 h. Temporal expression of TGF-βs, p-Smad2, Smad7, and CTGF was analyzed. High VT ventilation did not change gene expression of TGF-βs and Smad7 but induced rapid and sustained expression of p-Smad2 that precedes increased CTGF expression. CTGF and p-Smad2 were localized in bronchiolar epithelial cells, alveolar walls and septa. These data suggest that high Vt ventilation activates the Smad2 pathway, which may be responsible for downstream induction of CTGF expression in newborn rat lungs.
Similar content being viewed by others
Main
Mechanical ventilation is essential for managing prematurely born infants with respiratory failure. However, ventilation with high tidal volume (VT) can lead to ventilator induced lung injury (VILI) and bronchopulmonary dysplasia (BPD) (1–3). The lung pathology of BPD is characterized by fewer and larger alveoli, dysmorphic and decreased capillary network, and variable interstitial fibrosis, suggesting abnormal lung development and injury repair processes (4,5). Most of the studies in VILI and BPD have been focused on high VT induced lung proinflammatory response (6–9). Little is known about the effect of high VT on expression of growth factors that are key to lung development and injury repair in neonatal lungs.
Connective tissue growth factor (CTGF) belongs to the CCN family of early gene products with a high degree of amino acid sequence homology and 38 conserved cysteine residues (10,11). CTGF promotes fibroblast proliferation, extracellular matrix (ECM) production, myofibroblast differentiation, and cell adhesion and migration (12–16). CTGF is a potent profibrotic cytokine and its mRNA and protein levels have been correlated with the degree of lung fibrosis in bleomycin-treated mice and in human fibrotic lung disorders (17–19). Previous studies have demonstrated that mechanical stress drastically induces CTGF expression in cultured fibroblasts (20,21). CTGF is closely linked to TGF-β. Studies have demonstrated that TGF-β is a major inducer of CTGF expression in a variety of tissues and organs including the lung (11,22–24). Activation of the Smad pathway plays a key role in TGF-β induction of CTGF expression (25,26). TGF-β stimulation of fibroblast proliferation, collagen synthesis, and myofibroblast differentiation is mediated via a CTGF-dependent pathway (13–15). Recent data suggest that CTGF plays a role in lung development and neonatal lung injury. Using an embryonic lung explant model, we have demonstrated that endogenous expression of CTGF and TGF-β induced CTGF expression is mediated via the Smad2 pathway (27). Furthermore, addition of recombinant CTGF into the culture medium inhibited branching morphogenesis (27). A recent study in a neonatal rat model showed that hyperoxia exposure increased CTGF mRNA and protein expression, which precedes the fibrotic phase of lung injury (28). These data suggest that CTGF is a negative regulator for lung morphogenesis and may play a role in hyperoxia-induced lung injury and fibrosis in the neonatal lung. However, the role of CTGF in high VT induced lung injury in neonates is unknown.
We hypothesized that high VT ventilation induces CTGF expression in newborn rat lungs. To test this hypothesis, newborn rats were ventilated with normal or high VT. CTGF mRNA and protein expression were evaluated in the lungs of these animals and compared with control nonventilated animals. Temporal expression of TGF-βs, phosphorylated Smad2 (p-Smad2), a key intracellular transducer of TGF-β responses, and Smad7, a inhibitory Smad was also investigated to identify the potential signal transduction pathway mediating high VT induced CTGF expression in newborn rat lungs.
MATERIALS AND METHODS
Animal preparation and ventilator protocol.
The animal protocol was approved by the Animal Care and Use Committee of the University of Miami School of Medicine. Newborn Sprague–Dawley rats (7–14 d old) were anesthetized by intraperitoneal injection of ketamine (40 mg/kg) and xylazine (4 mg/kg) and tracheotomized. To compare the effects of normal VT and high VT on expression of CTGF, animals were randomly assigned to one of the following three groups:
-
Group 1: control (no-ventilation)
-
Group 2: ventilation with normal VT (10 mL/kg) for 6 h
-
Group 3: ventilation with high VT (25 mL/kg) for 6 h
The normal VT and high VT were based on a recent study of VILI in newborn rats (9). To determine the potential signal transduction pathways mediating CTGF expression, two additional groups of animals were studied:
-
Group 4: ventilation with high VT (25 mL/kg) for 1 h
-
Group 5: ventilation with high VT (25 mL/kg) for 3 h
The animals were ventilated using a time-cycled ventilator (Sechrist Infant Ventilator model iv-100B, Anaheim, CA) with positive end-expiratory pressure (PEEP) of 3 cm H2O, inspiratory time of 0.2 s, and 40% oxygen (O2). Airflow was measured by a heated pneumotachograph (Model 8430B, flow range 0–3 L/min, linearity 0.2%, Hans Rudolph, Inc. Kansas City, MI) placed between the tracheostomy tube and the ventilator circuit. The differential pressure output from the pneumotachograph was measured with a transducer (MP45, Validyne Engineering Co., Northridge, CA) and amplified by a pressure amplifier (Gould Instrument, Cleveland, OH). The flow signal was electronically integrated to obtain VT as described before (29). The peak inspiratory pressure (PIP) was adjusted to maintain a VT in the desired range. The end-tidal CO2 (ETCO2) was measured intermittently (every 30 min) by a Micro-Capnometer (Columbus Instrument, Columbus, OH) via the side port of the tracheostomy tube and was maintained at the same level for normal and high VT groups by adjusting the ventilator rate and dead space. Heart rate, airflow, VT, PIP, and PEEP were monitored continuously throughout the experiments. Body temperature was continuously monitored with a rectal thermal probe (Yellow Springs Instrument Co., Yellow Springs, OH), and maintained within the normal range for age (35.8–36.2°C) by using a servo-controlled radiant warmer. Control animals breathed air and received anesthesia and tracheotomy as described before euthanasia. At the end of the experiment, animals were euthanized with an overdose of pentobarbital and lungs were removed for subsequent analysis.
Lung histology.
The left lungs from control and 6 h ventilated animals were infused with 4% paraformaldehyde via a tracheal catheter under 20 cm H2O pressure and fixed overnight at 4°C. Fixed lung tissues were paraffin-embedded and 5 μm sections were stained by the standard hematoxylin and eosin (HE) method. Lung histology was examined by a pathologist unaware of the experimental conditions.
RNA isolation and quantitative real-time (RT)-PCR.
Total RNA was isolated from frozen right lung tissue using Trizol reagent (Invitrogen, Carsbad, CA) and then treated with DNase to remove possible DNA contamination. Two micrograms of total RNA was reverse-transcribed in a 20 μL reaction by using a first-strand cDNA synthesis kit according to the manufacturer's protocol (Invitrogen, Carsbad, CA). The quantitative real-time RT-PCR was performed on a Light-cycler (Roche, Indianapolis, IN). Each reaction included diluted first-strand cDNA, rat IL-6, TNF-α, CTGF, TGF-β1, TGF-β2, TGF-β3, or glyceraldehyde-3-phosphate dehydrogenase (GAPDH) primers, and RT2 Real-Time PCR SYBR Green master mix according to the manufacturer's instructions (Superarray, Frederick, MD). Real-time RT-PCR conditions were 95°C for 15 min, followed by 40 cycles of 95°C for 30 s, 55°C for 30 s, and 72°C for 30 s. RNase-free water was used as a negative control. For each target gene, a standard curve was established by performing a series dilution of first-strand cDNA. The mRNA expression levels of these factors were determined from the standard curve and normalized to GAPDH.
Northern blot analysis.
Twenty microgram of total RNA from each lung sample was electrophoresed on 1.2% agarose gel containing formaldehyde and transferred to a nylon membrane. A 1 kb human CTGF cDNA fragment that has been cloned into the pRc/CMV plasmid was used to generate radiolabeled CTGF probe. A 497 bp mouse GAPDH cDNA was prepared by RT-PCR using primers 5′-ACCACAGTCCATGCCATCAC-3′ (position 593–613) and 5′-TCCACCACCCTGTTGATGTA-3′ (position 1090–1110). The CTGF and GAPDH cDNAs were radiolabeled with [32P]dCTP using the DNA labeling kit and purified using Quick Spin Columns (Amersham Biosciences, Piscataway, NJ). The hybridization was first carried out with [32P]-labeled CTGF probe, then stripped and rehybridized with [32P]-labeled GAPDH probe as described (30). The intensities of mRNA bands on the autoradiography were quantified by Quantity One Imaging Analysis Program (Bio-Rad, Richmond, CA). The CTGF mRNA levels were determined after normalization to GAPDH.
Western blot analysis.
Total protein was extracted from frozen right lung tissues with a lysis buffer from Active Motif according to the manufacturer's protocol (Carsbad, CA). The protein concentrations were measured by BCA protein assay using commercial kits from Pierce Biotechnology Inc (Rockford, IL). Seventy-five micrograms of total protein was fractionated by SDS-PAGE on a 10% Tris-glycine precast gel (Bio-Rad) and then transferred to a nitrocellulose membrane (Amersham). The membrane was incubated with a primary antibody for CTGF (1:1000 dilution), total Smad2/3 (1:500 dilution), Smad7 (1:500) (Santa Cruz Biotechnology Inc, Santa Cruz, CA), p-Smad2 (1:500 dilution) (Chemicon, Temecula, CA) or 1:10000 diluted mouse anti-β-actin antibody (Sigma Chemical Co., St. Louis, MO) overnight at 4°C, then incubated for 1 h at room temperature with the respective HRP-conjugated secondary antibodies. Antibody bond proteins were detected using ECL chemiluminescence method (Amersham). The intensities of protein bands were quantified by Quantity One Imaging Analysis Program. The CTGF and Smad7 levels were determined after normalization to β-actin and p-Smad2 levels were normalized to total Smad2/3.
Immunohistochemistry.
Localization of CTGF, p-Smad2, or total Smad2/3 protein expression was determined by immunostaining with a rabbit CTGF antibody (Torrey Pines Biolabs, Huston, TX), a rabbit p-Smad2 antibody (Chemicon) or a goat total Smad2/3 antibody (Santa Cruz). The dilution for all three antibodies was 1:1000. These antibodies are specific and have been used in many published studies (31,32). Nonimmune IgG was used as the negative control. The antibody bond positive cells were detected with a biotinylated secondary antibody, streptavidin–biotin-peroxidase complexes and DAB substrate (Vector, Burlingame, CA).
Statistical analysis.
Data are presented as mean ± SD. Comparisons were performed using one-way ANOVA followed by the Student-Newman-Keuls test. A p value of less than 0.05 was considered significant.
RESULTS
Physiologic data.
As shown in Table 1, the control rats and 6-h ventilated animals had similar age and weight. As expected, the PIP for the high VT group was significantly higher than the PIP for the normal VT group. The ETCO2 was in the same range for both normal and high VT ventilated groups.
Lung histology.
The most striking finding was severe over-distension of the distal airspaces and thinning of the alveolar septum seen in the high VT ventilated lungs (Fig. 1). The normal VT lungs appeared similar to the control lungs.
Histology of control, normal, and high VT ventilated lungs. Lung tissue sections from control (A), normal VT (B), and high VT (C) ventilation for 6 h were stained by standard H&E method. The histology of normal VT lungs was similar to that of controls. Severe alveolar over-distension and thinning of the septa were noticed in the high VT ventilated lungs. Images were taken under 200× magnifications. Bars = 40 μm.
Expression of IL-6 and TNF-α mRNA.
Ventilation with normal or high VT for 6 h did not change mRNA expression of TNF-α compared with the control group (data not shown). However, high VT ventilation resulted in near threefold increase in IL-6 mRNA expression (3.12 ± 1.72) compared with the control group (1.11 ± 0.42) and normal VT group (1.45 ± 0.5) (p = 0.011).
Expression of CTGF mRNA.
When compared with the control group, ventilation with normal VT for 6 h did not affect CTGF mRNA expression. However, ventilation with high VT for 6 h significantly upregulated CTGF mRNA expression compared with both control and normal VT groups (Fig. 2).
Induction of CTGF mRNA expression by mechanical ventilation is VT- dependent. A, Representative autoradiographs from Northern blot analysis. C: control; N: normal VT for 6 h; H: high VT for 6 h. B, Densitometric quantification of Northern blot analysis. Data are mean ± SD from seven animals in each group. Increased CTGF mRNA was detected in high VT ventilated lungs. *p < 0.001 compared with control and normal VT ventilation.
Expression of CTGF protein.
Consistent with CTGF mRNA expression, normal VT ventilation for 6 h did not change CTGF protein expression compared with the control group. However, high VT ventilation for 6 h significantly increased CTGF protein expression compared with both control and normal VT groups (Fig. 3).
High VT ventilation upregulates CTGF protein expression. CTGF protein was detected by Western blot with a CTGF specific antibody in control, normal VT and high VT ventilated lungs (6 h) and normalized by β-actin. A, Representative Western blot images. S: CTGF standard. B, Densitometric quantification of Western blot analysis. Results are mean ± SD from control (n = 6), normal VT (n = 5) and high VT (n = 4) groups. High VT increased CTGF protein expression compared with both control and normal VT group. *p < 0.001.
Localization of CTGF protein expression.
As shown in Fig. 4, CTGF protein was sparsely detected with moderate intensity in alveolar walls and septa, and weak intensity in bronchiolar epithelial cells in control and normal VT ventilated lungs (Fig. 4A,B). However, CTGF protein was abundantly detected with strong intensity in alveolar walls and septa, and bronchiolar epithelial cells in high VT ventilated lungs (Fig. 4C).
Localization of CTGF protein by immunohistochemistry. Lung tissue sections were immunostained with a CTGF specific antibody. CTGF positive cells (brown color) are indicated by arrows. A, control; B, normal VT ventilation (6 h); C, high VT ventilation (6 h); D, negative control stained with nonimmune IgG. CTGF was detected with stronger intensity and more abundance in high VT ventilated lungs when compared with control and normal VT ventilated lungs. Images were taken under 400× magnifications. Bar = 20 μm.
Temporal effect of high VT on mRNA expression of TGF-β1, TGF-β2, TGF-β3, and CTGF.
There was no significant difference in mRNA expression of the three TGF-βs among control and the groups ventilated with high VT (Table 2). High VT ventilation for 1 or 3 h did not change CTGF mRNA expression, but increased CTGF mRNA expression at 6 h (Table 2) which was also demonstrated by Northern blot analysis described above (Fig. 2). Active TGF-β1 was measured by ELISA (without activation) in protein extracts from control and high VT ventilated lungs and there was no difference among the groups (data not shown).
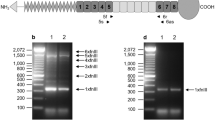
Expression of Smad7 and p-Samd2 in response to high VT ventilation.
Western blot analysis revealed that high VT ventilation did not change Smad7 expression at any time point (control: 0.45 ± 0.18; 1 h: 0.48 ± 0.07; 3 h: 0.51 ± 0.07; 6 h: 0.35 ± 0.13, p = 0.37). In contrast, high VT ventilation induced rapid and sustained p-Smad2 expression. As demonstrated in Fig. 5, high VT significantly induced p-Smad2 expression as early as 1 h and this lasted for up to 6 h. These results suggest that activation of Smad2 precedes CTGF induction by high VT. On immunohistochemistry, p-Smad2 was detected with weak intensity in alveolar walls and septa and bronchiolar epithelial cells in control lungs (Fig. 6A). However, p-Smad2 was detected with strong intensity in alveolar walls and septa, and bronchiolar epithelial cells in 6 h high VT ventilated lungs (Fig. 6C). In contrast, total Smad-2 was detected with similar intensity in both control (Fig. 6B) and high VT (Fig. 6D) ventilated lungs. The localization of p-Smad2 was similar to that of CTGF.
High VΤ upregulates p-Smad2 expression. Expression of p-Smad2 was determined by Western blot analysis using a p-Smad2 specific antibody and normalized by total Smad2 in high VT ventilated lungs. A, Representative Western blot images. Ventilation durations (h) are indicated on the top of the images. B, Densitometric quantification of Western blot analysis. Results are mean ± SD from four animals in each group. High VT ventilation increased p-Smad2 expression from 1 to 6 h compared with control groups. *p < 0.001.
Localization of p-Smad2. Lung tissue sections were stained with a p-Smad2 or a total Smad2 specific antibody. Positive cells for p-Smad2 and total Smad2 (brown color) are indicated by arrows. A, control stained with a p-Samd2 antibody; B, control stained with a total Smad2 antibody; C, high VT ventilated lung stained with a p-Smad2 antibody; D, high VT ventilated lung stained with a total Smad2 antibody. P-Smad2 was strongly detected in bronchiolar epithelial cells and alveolar walls and septa in high VT ventilated lungs. Images were taken under 400× magnifications. Bar = 20 μm.
DISCUSSION
The data of this study demonstrate that high VT ventilation results in alveolar over-distension and upregulation of CTGF expression in newborn rat lungs. High VT ventilation also induces rapid and sustained p-Smad2 expression that precedes CTGF induction. To the best of our knowledge, this is the first report to demonstrate that high VT ventilation is associated with activation of the Smad2 pathway and induction of CTGF expression in an in vivo neonatal animal model.
Despite the fact that aggressive ventilation is a major contributor in the pathogenesis of BPD, little is known about the molecular basis of volume induced lung injury in the immature lung. Although many studies in volume induced lung injury and BPD have been conducted in large animal models such as baboons and lambs, these animals are difficult to maintain and expensive (33,34). The lung developmental stage of premature infants at risk for BPD is at the prealveolar stage, i.e., later canalicular and saccular stages (35,36). The lungs of newborn rats are at the saccular stage that rapidly progresses to the alveolar stage in the first 2 weeks after birth (37,38). Although the newborn rat lung is not surfactant deficient, its structure closely resembles the lung structure of premature infants at risk for BPD. We ventilated newborn rats (7–14 d) to investigate the effect of high VT on lung expression of CTGF mRNA and protein. Consistent with our hypothesis, high VT ventilation dramatically upregulated expression of CTGF mRNA and protein in newborn rat lung. In vitro studies have demonstrated that the CTGF gene is one of the most striking genes induced by mechanical stress (20,21). CTGF is a multifunctional cytokine that promotes fibroblast proliferation, ECM production, and myofibroblast differentiation (13–15). Overexpression of CTGF is associated with pulmonary fibrosis in adult human and animal models (17–19). Our data suggest that high VT induced CTGF expression may cause profibrotic responses in the neonatal lung.
Previous studies have indicated that TGF-β is a key inducer of CTGF expression in a variety of tissues and organs (11,22–24). In the present study, we took a step further to identify the potential upstream signal transduction pathway that mediates high VT induced CTGF expression by focusing on the TGF-β and Smad2 axis. TGF-β is a family of closely related peptides including TGF-β1, TGF-β2, and TGF-β3. TGF-βs initiate their action by binding to the TGF-β receptors on the cell membrane and phosphorylate Smad2/3. The p-Smad2/3 forms a complex with Smad4, translocates to the nucleus and binds to the target gene promoters to activate gene transcription (39). Smad7 is an inducible intracellular inhibitor that decreases Smad2/3 phosphorylation by blocking their access to TGF-β receptors (39). Studies have indicated that TGF-β activated Smad2/3 signal transduction pathway plays a key role in TGF-β induction of CTGF expression (25,26). We have previously shown that TGF-β induces CTGF expression via the Smad2-dependent pathway during early embryonic lung development (27). In the present study, we examined the temporal relationship of Smad7, TGF-βs, Smad2, and CTGF in response to high VT ventilation in newborn rat lungs. We demonstrated that high VT induction of CTGF expression is independent of decreased inhibitory Smad7. Although mRNA expression of TGF-βs and active TGF-β1 were not altered by high VT at any time point, rapid and sustained expression of p-Smad2 was induced by high VT and that preceded CTGF mRNA and protein expression. We also showed that p-Smad2 and CTGF are expressed in similar locations. These data demonstrate a temporal and spatial association of p-Smad2 and CTGF expression suggesting that high VT ventilation may activate the Smad2 signal transduction pathway which in turn results in upregulation of CTGF expression. Further studies are needed to determine whether high VT activation of the Smad2 pathway is TGF-β-dependent or TGF-β-independent and if Smad2 activation mediates CTGF induction.
The present study was not designed to evaluate the effect of O2 concentration on CTGF expression. All animals were ventilated with 40% O2 which is necessary to keep their hemodynamic function stable during the 6 h experiments. The fact that the animals ventilated with normal VT did not exhibit any change in lung histology or CTGF expression suggests that the increased CTGF was caused by high VT and not by O2.
We did not measure arterial blood gases due to the difficulty to obtain sufficient blood for such analysis. However, we closely monitored the ETCO2, which was kept in the same range between the normal VT and high VT groups by adjusting the dead space and ventilator rates. This eliminated the possible effect of different PaCO2 and pH on the results.
TNF-α is known for its ability to inhibit the TGF-β dependent Smad2/3 pathway and CTGF expression (40). A recent study has demonstrated that antenatal endotoxin exposure increases expression of TGF-β and p-Smad2 but decreases CTGF expression in lungs of preterm lambs (41). The decreased CTGF expression was explained by the concurrent elevation of TNF-α. In the present study, high VT ventilation did not increase TNF-α expression. This may explain why high VT ventilation induced significant expression of p-Smad2 and CTGF in newborn rat lungs.
Our model did not intend to identify the downstream CTGF effects in response to high VT because of the relatively short duration of ventilation. Recent data from our laboratory indicate that CTGF is a negative regulator of lung branching morphogenesis (27). CTGF is associated with TGF-β induced fibroblast to myofibroblast differentiation that may interfere with secondary septal formation and alveolar development (15). In addition, CTGF is also a profibrotic cytokine that may result in interstitial fibrosis (13,14). We speculate that prolonged overexpression of CTGF in the alveolar septa may inhibit alveolar development, produce interstitial fibrosis and result in BPD-like architecture in the immature lung.
In conclusion, the present study demonstrates that high VT ventilation activates the Smad2 pathway and induces CTGF expression in newborn rat lungs. These results suggest an important role of this pathway in high VT induced lung injury in neonates.
Abbreviations
- BPD:
-
bronchopulmonary dysplasia
- CTGF:
-
connective tissue growth factor
- ECM:
-
extracellular matrix
- ETCO2:
-
end-tidal CO2
- GAPDH:
-
glyceraldehyde-3-phosphate dehydrogenase
- HE:
-
hematoxylin and eosin
- PEEP:
-
positive end-expiratory pressure
- PIP:
-
peak inspiratory pressure
- p-Smad2:
-
phosphorylated Smad2
- VILI:
-
ventilator induced lung injury
- V T :
-
tidal volume
References
Jobe AH, Bancalari E 2001 Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163: 1723–1729
Attar MA, Donn SM 2002 Mechanisms of ventilator-induced lung injury in premature infants. Semin Neonatol 7: 353–360
Donn SM, Sinha SK 2003 Can mechanical ventilation strategies reduce chronic lung disease?. Semin Neonatol 8: 441–448
Husain AN, Siddiqui NH, Stocker JT 1998 Pathology of arrested acinar development in postsurfactant bronchopulmonary dysplasia. Hum Pathol 29: 710–717
Jobe AJ 1999 The new BPD: an arrest of lung development. Pediatr Res 46: 641–643
Jonsson B, Tullus K, Brauner A, Lu Y, Noack G 1997 Early increase of TNF alpha and IL-6 in tracheobronchial aspirate fluid indicator of subsequent chronic lung disease in preterm infants. Arch Dis Child Fetal Neonatal Ed 77: F198–F201
Kotecha S, Wilson L, Wangoo A, Silverman M, Shaw RJ 1996 Increase in interleukin (IL)-1α and IL-6 in bronchoalveolar lavage fluid obtained from infant with chronic lung disease of prematurity. Pediatr Res 40: 250–256
Cao L, Liu C, Cai B, Jia X, Kang L, Speer CP, Sun B 2004 Nuclear factor-kappa B expression in alveolar macrophages of mechanically ventilated neonates with respiratory distress syndrome. Biol Neonate 86: 116–123
Copland IB, Martinez F, Kavanagh BP, Engelberts D, Mckerlie C, Belik J, Post M 2004 High tidal volume ventilation causes different inflammatory responses in newborn versus adult lung. Am J Respir Crit Care Med 169: 739–748
Bork P 1993 The modular architecture of a new family of growth regulator related to connective tissue growth factor. FEBS Lett 327: 125–130
Grotendorst GR 1997 Connective tissue growth factor: a mediator of TGF-beta action on fibroblasts. Cytokine Growth Factor Rev 8: 171–179
Leask A, Abraham DJ 2003 The role of connective tissue growth factor, a multifunctional matricellular protein, in fibroblast biology. Biochem Cell Biol 81: 355–363
Kothapalli D, Frazier KS, Welply A, Segarini PR, Grotendorst GR 1997 Transforming growth factor beta induces anchorage-independent growth of NRK fibroblasts via a connective tissue growth factor-dependent signaling pathway. Cell Growth Differ 8: 61–68
Duncan MR, Frazier KS, Abramson S, Williams S, Klapper H, Huang X, Grotendorst GR 1999 Connective tissue growth factor mediates transforming growth factor beta-induced collagen synthesis: down-regulation by cAMP. FASEB J 13: 1774–1786
Grotendorst GR, Rahmanie H, Duncan MR 2004 Combinatorial signaling pathways determine fibroblast proliferation and myofibroblast differentiation. FASEB J 18: 469–479
Crean JK, Finlay D, Murphy M, Moss C, Godson C, Martin F, Brady HR 2002 The role of p42/44 MARK and protein kinase B in connective tissue growth factor induced extracellular matrix protein production, cell migration, and actin cytoskeletal rearrangement in human mesangial cells. J Biol Chem 277: 44187–44194
Lasky JA, Ortiz LA, Tonthat B, Hoyle GW, Corti M, Athas G, Lungarella G, Brody A, Friedman M 1998 Connective tissue growth factor mRNA expression is upregulated in bleomycin-induced lung fibrosis. Am J Physiol 275: L365–L371
Allen JT, Knight RA, Bloor CA, Spiteri MA 1999 Enhanced insulin-like growth factor binding protein-related protein 2 (Connective tissue growth factor) expression in patients with idiopathic pulmonary fibrosis and pulmonary sarcoidosis. Am J Respir Cell Mol Biol 21: 693–700
Sato S, Nagaoka T, Hasegawa M, Tamatani T, Nakanishi T, Takigawa M, Takehara K 2000 Serum level of connective tissue growth factor are elevated in patients with systemic sclerosis: association with extent of skin sclerosis and severity of pulmonary fibrosis. J Rheumatol 27: 149–154
Kessler D, Dethlefsen S, Haase I, Plomann M, Hirche F, Krieg T, Eckes B 2001 Fibroblasts in mechanically stressed collagen lattices assume a “synthetic” phenotype. J Biol Chem 276: 36575–36585
Schild C, Trueb B 2002 Mechanical stress is required for high-level expression of connective tissue growth factor. Exp Cell Res 274: 83–91
Grotendorst GR, Okochi H, Hayashi N 1996 A novel transforming growth factor beta response element controls the expression of the connective tissue growth factor gene. Cell Growth Differ 7: 469–480
Blom IE, Goldschmeding R, Leask A 2002 Gene regulation of connective tissue growth factor: new targets for antifibrotic therapy?. Matrix Biol 21: 473–482
Kelly M, Kolb M, Bonniaud P, Gauldie J 2003 Re-evaluation of fibrogenic cytokines in lung fibrosis. Curr Pharm Des 9: 39–49
Holmes A, Abraham DJ, Sa S, Xu S, Black CM, Leask A 2001 CTGF and SMADs, maintenance of scleroderma phenotype is independent of SMAD signaling. J Biol Chem 276: 10594–10601
Leask A, Holmes A, Black CM, Abraham DJ 2003 Connective tissue growth factor gene regulation. Requirements for its induction by transforming growth factor-beta 2 in fibroblasts. J Biol Chem 278: 13008–13015
Wu S, Peng J, Duncan MR, Kasisomayajula K, Grotendorst G, Bancalari E 2007 ALK-5 Mediates Endogenous and TGF-{beta}1-induced Expression of CTGF in Embryonic Lung. Am J Respir Cell Mol Biol 36: 552–561
Chen CM, Wang LF, Chou HC, Lang YD, Lai YP 2007 Up-regulation of connective tissue growth factor in hyperoxia-induced lung fibrosis. Pediatr Res 62: 128–133
Lessa A, Suguihara C, Xianyu S, Hehre D, Devia C, Bancalari E The effect of pentoxifyline on the pulmonary response to high tidal volume ventilation in rats. Pulm Pharmacol Ther (in press).
Wu S, Moomaw CR, Tomer KB, Falck JR, Zeldin DC 1996 Molecular cloning and expression of CYP2J2, a human cytochrome P450 arachidonic acid epoxygenase highly expressed in heart. J Biol Chem 271: 3460–3468
Ruperez M, Lorenzo O, Blanco-Colio LM, Esteban V, Egido J, Ruiz-Ortega M 2003 Connective tissue growth factor is a mediator of angiotensin II-induced fibrosis. Circulation 108: 1499–1505
Dong C, Zhu S, Wang T, Yoon W, Goldschmidt-Clermont PJ 2002 Upregulation of PAI-1 is mediated through TGF-beta/Smad pathway in transplant arteriopathy. J Heart Lung Transplant 21: 999–1008
Coalson JJ, Winter VT, Siler-Khodr T, Yoder BA 1999 Neonatal chronic lung disease in extremely immature baboons. Am J Respir Crit Care Med 160: 1333–1346
Bland RD, Xu L, Ertsey R, Rabinovitch M, Albertine KH, Wynn KA, Kumar V, Ryan RM, Swartz DD, Csiszar K, Fong KS 2007 Dysregulation of pulmonary elastin synthesis and assembly in preterm lambs with chronic lung disease. Am J Physiol Lung Cell Mol Physiol 292: L1370–L1384
Massaro GD, Massaro D 1996 Formation of pulmonary alveoli and gas-exchange surface area: quantitation and regulation. Annu Rev Physiol 58: 73–92
Coalson JJ 2006 Pathology of bronchopulmonary dysplasia. Semin Perinatol 30: 179–184
Burri PH 1997 Postnatal development and growth. In: Crystal RG, West JB (eds) The Lungs: Scientific Foundations. 2nd ed. Lippincott-Raven Publishers, Philadephia, pp 1013–1026
Zoetis T, Hurtt ME 2003 Species comparison of lung development. Birth Defects Res B Dev Reprod Toxicol 68: 121–124
Heldin CH, Miyazono K, Dijke P 1997 TGF-beta signaling from cell membrane to nucleus through SMAD proteins. Nature 390: 465–471
Leask A, Abraham DJ 2004 TGF-β signaling and the fibrotic response. FASEB J 18: 816–827
Kunzmann S, Speer CP, Jobe AH, Kramer BW 2007 Antenatal inflammation induced TGF-beta1 but suppressed CTGF in preterm lungs. Am J Physiol Lung Cell Mol Physiol 292: L223–L231
Acknowledgements
We thank Ms. Brenda Roberts for her excellent technical support on tissue preparation and immunohistochemistry.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by funding from NIH grant K08 HD046582, the Project New Born University of Miami, and a grant from Bank of America Charitable Foundation, INC.
Rights and permissions
About this article
Cite this article
Wu, S., Capasso, L., Lessa, A. et al. High Tidal Volume Ventilation Activates Smad2 and Upregulates Expression of Connective Tissue Growth Factor in Newborn Rat Lung. Pediatr Res 63, 245–250 (2008). https://doi.org/10.1203/PDR.0b013e318163a8cc
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e318163a8cc
This article is cited by
-
Perinatal origins of bronchopulmonary dysplasia—deciphering normal and impaired lung development cell by cell
Molecular and Cellular Pediatrics (2023)
-
S-endoglin expression is induced in hyperoxia and contributes to altered pulmonary angiogenesis in bronchopulmonary dysplasia development
Scientific Reports (2020)
-
Preterm birth and sustained inflammation: consequences for the neonate
Seminars in Immunopathology (2020)
-
Inflammatory Response of Pulmonary Artery Smooth Muscle Cells Exposed to Oxidative and Biophysical Stress
Inflammation (2018)
-
Recombinant CCN1 prevents hyperoxia-induced lung injury in neonatal rats
Pediatric Research (2017)