Abstract
We have previously reported concordant changes in cerebral intravascular oxygenation measured by near infrared spectroscopy (NIRS) and mean arterial blood pressure (MAP) in premature infants. We hypothesized that the cerebral oxygenation changes are caused by MAP-induced alterations in cerebral blood flow (CBF) and studied these parameters in neonatal piglets (n = 6). Changes in cerebral intravascular oxygenation were measured by NIRS from the hemoglobin difference (HbD) signal (oxyhemoglobin-deoxyhemoglobin). CBF was measured by the radioactive microsphere technique. The cerebral circulation was also monitored by Doppler determinations of CBF velocity (time average mean velocity) in the anterior cerebral artery. Hypotension to <50% of baseline MAP was achieved by a ligature around the ascending aorta. Arterial oxygenation was maintained constant by mechanical ventilation. As observed in our studies of premature infants, cerebral HbD and MAP showed concordant changes. Hypotension was accompanied by significant decreases both in CBF (42.8 ± 12.5% of baseline p < 0.01) and HbD (-65.0 ± 22.0 µmol/L·dpf, p < 0.01). HbD was significantly correlated with MAP (p < 0.05) and time average mean velocity (p = 0.01). Importantly, decreases in cerebral total hemoglobin (HbT), a measure of cerebral blood volume, did not correlate significantly with decreases in MAP. We conclude that 1) decreases in cerebral intravascular oxygenation, as assessed by NIRS, observed with decreases in MAP reflect a decline in CBF, and hence oxygen delivery, 2) the HbD signal is more sensitive to changes in CBF than the HbT signal, and 3) NIRS recordings may have clinical utility in detecting cerebral ischemia.
Similar content being viewed by others
Main
Changes in CBF induced by changes in MAP may be an important cause of cerebral injury in premature infants (1,2). Intermittent measurements of CBF in infants have supported the concept of a "pressure passive" circulation in at least a subset of such infants (1,3). However, definition of a pressure passive circulation in the human infant has been hindered by the lack of a noninvasive, conveniently applied technique for the continuous assessment of cerebral perfusion. Using the bedside technique of NIRS, we have noted in premature infants concordant changes between MAP and cerebral intravascular oxygenation, the latter assessed by NIRS as the difference between the signals for Hbo2 and Hb, i.e. HbD = Hbo2 - Hb (4). These changes in cerebral HbD were particularly prominent during hypotensive episodes. We postulated that these changes in cerebral intravascular oxygenation were caused by MAP-induced changes in CBF and that continuous measurements of cerebral intravascular oxygenation by NIRS could be used to examine the relationship of CBF and MAP in the human infant. However, a relationship between the NIRS measurement of cerebral intravascular oxygenation and cerebral perfusion has not been established. Therefore, in this study of neonatal piglets subjected to hypotension we evaluated the relationship between simultaneous measurements of cerebral intravascular oxygenation (i.e. HbD as determined by NIRS), and CBF, as determined by radioactive microspheres. Additionally cerebral perfusion was monitored by the clinically used Doppler method for determination of CBF velocity.
METHODS
Animals. Six piglets (Charles River Laboratories, Wilmington, MA) were studied at 1-2 wk of age. The animals were obtained 1-2 d before the study and fasted for 12 h before surgery. The studies were performed in compliance with institutional and National Institutes of Health guidelines for laboratory animal care.
Surgical preparation. The animals were anesthetized with an intraperitoneal injection of ketamine (20 mg/kg), and after intubation were mechanically ventilated with 25-30% inspired O2 and a tidal volume and respiratory rate which produced an arterial Pco2 of 35-45 mm Hg and an arterial Po2 of greater than 90 mm Hg. Venous and arterial catheters were inserted through the surgically exposed right femoral vein and artery into the thoracic inferior vena cava and aorta, respectively. Anesthesia was maintained with 70-75% nitrous oxide, 0.5-1% halothane by inhalation, and pancuronium (0.1 mg/kg i.v. every hour). An ECG was continuously monitored by surface electrodes, and arterial pressure by a pressure transducer on the arterial catheter. MAP was electronically sampled and recorded concordantly with NIRS data every second. Temperature was monitored by a rectal temperature probe and maintained at 37-38°C by a warming blanket.
The heart was exposed through a left thoracotomy. A cathered was inserted through pursestring sutures into the left atrium for injection of microspheres. A ligature of cloth umbilical tape was placed around the ascending aorta proximal to the carotid trunk. Tension on the ligature produced systemic arterial hypotension, which was measured via the arterial cathered positioned in the thoracic aorta. Varying tension on the ligature allowed both rapid (e.g. 30 s) and slow (e.g. 2-3 min) onset of hypotension. After each experiment, animals were killed while still under general anesthesia with an injection of euthanizing solution (pentobarbital and potassium chloride).
CBF measurement. CBF was measured by the radioactive microsphere technique (5). Microspheres (15-µm diameter) were labeled with 141Ce, 113Sn, 85Sr, 95Nb, or 46Sc. Approximately 2.5 × 106 microspheres were suspended in 0.5 mL of 10% dextran. The suspension was injected into the left atrial catheter. Commencing with the microsphere injection and continuing for 2 min, a measured quantity of blood (10 mL) was withdrawn at a constant rate by syringe pump (Dye dilution pump model 2603, Harvard Apparatus, South Natick, MA) from the catheter in the thoracic aorta. The blood samples served as a reference for the brain measurements. At the termination of the experiment, the brain was removed. The tissue sample volume for NIRS monitoring varies with the configuration of the light entry and exit points and the intensity of the light used (6). The spectrometer used in these experiments is capable of detecting Hbo2 and Hb signals in tissue with a separation between light entry and exit points of up to 6 cm. In addition, Monte Carlo mathematical modeling of photon travel in biologic scattering media suggests that NIRS used in these experiments should be sensitive to signals from a circular arc with diameter of at least 80% of the distance between the light entry and exit points (Hamamatsu Photonics, unpublished data). Hence, it is likely that our NIRS instrument sampled mainly from the cerebral hemispheres. Samples of the cerebral hemispheres corresponding to the area under the NIRS probes were removed and weighted. Radioactivity in the tissue samples and reference blood was counted in a gamma counter (Compugamma 1282, LKB Instruments Inc., Wallac, Finland). The tissue blood flow was calculated from the rate of withdrawal of the reference blood and the ratio of the tissue radioactivity to the reference blood. CBF was expressed as mL/min per 100 g of tissue.
Near infrared spectroscopy. For NIRS recordings, fiberoptic bundles for conveying near infrared light (NIRS optodes) were placed on each side of the ultrasound probe, 1.5 cm on each side of the sagittal suture midway between the orbits and the external auditory meatus. The optodes were positioned and held against the skull using a special clamp fixture. The interoptode space was 3.0 to 3.5 cm. After optode placement, the animal's head was covered with a light opaque drape.
NIRS recordings were made with a four-wavelength spectrometer (NIRO-500, Hamamatsu Photonics KK, Hamamatsu, Japan). Light was transmitted in sequential pulses through the skull at four wavelengths (776, 828, 848, and 913 nm). Photons emerging from the sample were collected by the second optode and counted by a photomultiplier tube. The difference between transmitted and received light intensity at each wavelength was used to determine OD changes at each wavelength. Computer calculations based on chromophore absorption spectra then determined changes in Hbo2 and Hb concentrations in (µmol/L)·dpf according to the modified Beer-Lambert law (7–9). The term "dpf" is the differential path length factor which corrects the measured optode separation distance for light scattering within the sample. The measured dpf is 4.39 in human neonates (10) and 4.34 in rats (7). Because the dpf for piglet brain is not specifically known, results are expressed in concentration change·dpf. The dpf was assumed to be constant in each experiment as previous investigators have shown that dpf remains constant even after death (11). The NIRS instrument made measurements of Hbo2 and Hb levels every 0.5 s and wrote the average value to a computer file every second.
The HbD was calculated as Hbo2 - Hb. Because hemoglobin oxygenation results in an increase in Hbo2 and a decrease in Hb, HbD increases with increased global cerebral hemoglobin oxygenation. Similarly, HbD decreases with global cerebral hemoglobin deoxygenation. HbT was calculated as the sum of Hbo2 plus Hb. If hematocrit is constant, changes in HbT are indicative of changes in cerebral blood volume.
Doppler ultrasonography. A high resolution ultrasound unit (Acuson XP-10, Mountain View, CA), equipped with a 7.0-MHz vector transducer was used for all imaging and Doppler studies. The anterior cerebral artery was identified in the interhemispheric fissure superior to the corpus callosum on coronal images using color Doppler imaging. The transducer was then fixed in position by a mechanical holder during the remainder of the experiment. A 1 × 1.5-mm cylindrical Doppler sample volume was used, and the angle of insonation was held constant at <45°. Angle-corrected TAV measurements were obtained every 10-20 s on velocity wave forms containing at least 10 cardiac cycles during blood pressure manipulation.
Experimental protocol. After stabilization on mechanical ventilation and general anesthesia, CBF was measured by microsphere injection. Hypotension to less than 50% of baseline MAP within 30-40 s was then induced by tension on the aortic ligature. HbD was observed to parallel changes in MAP. When both MAP and HbD signals were constant, hypotension was maintained for 3-4 min during which a second microsphere injection for CBF measurement was performed. The ligature was then released. After restoration of baseline blood pressure, Doppler TAV measurements were performed at baseline, during and after a second hypotensive episode of 4-5 min. During this hypotensive episode, MAP was decreased more gradually (e.g. over 2 min) to allow intermittent measurement of TAV. Mechanical ventilation and inspired oxygen concentrations were maintained constant from baseline measurements through the induced hypotensive episodes.
Data analysis. All values are reported as mean ± SD and were analyzed using a statistical analysis system (Systat, Systat Inc., Evanston, IL). The significance of observed changes between baseline and hypotension was calculated by paired t tests. The correlation of NIRS and Doppler data were analyzed by analysis of covariance. Significance levels of p < 0.05 were considered significant.
RESULTS
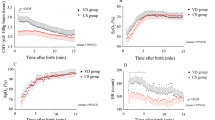
We first established conditions to cause a decrease in MAP to less than 50% of baseline. Thus, tension on the aortic ligature was adjusted to decrease the baseline MAP of 68.0 ± 11.2 to a hypotensive level of 31.2 ± 4.4 mm Hg. As a percentage, the hypotensive level of MAP was 46.5 ± 7.1% of baseline (p < 0.01) (Fig 1A).
A, reduction in blood pressure (MAP) during hypotensive episodes. The difference between baseline and hypotensive MAP values is significant at p < 0.01. B, reduction in CBF during hypotension. The difference between baseline and hypotensive CBF values is significant at p < 0.01. CBF was measured by the radioactive microsphere technique and is expressed in mL/min per 100 g of tissue.
CBF measured by the radioactive microsphere technique, declined similarly with the decline in MAP. Thus, CBF at baseline was 127.0 ± 33.6 mL min-1 100 g-1, and during hypotension, 52.6 mL min-1 100 g-1. As a percentage, the hypotensive level of CBF was 42.8 ± 12.5% of baseline (p < 0.01) (Fig 1B).
Cerebral intravascular oxygenation, as assessed by the NIRS-determined cerebral HbD value, decreased with the reduction in CBF and MAP (Fig. 2). The mean decrease in HbD was 65.0 ± 22.0 µmol/L·dpf (p < 0.01). Cerebral blood volume, as assessed by the NIRS-determined HbT signal, showed a smaller and less consistent decrease with hypotension (mean decrease = 11.4 ± 14.0 µmol/L·dpf, NS) (Fig. 2). An example of HbD and MAP recordings is shown in Fig. 3.
To assess the temporal coupling of changes in MAP, HbD, and a measure of cerebral perfusion, NIRS and blood pressure data points were compared with corresponding Doppler ultrasound measurements of CBF velocity. Analysis of covariance between the changes in HbD and MAP showed a significant correlation (p < 0.05). CBF velocity was also significantly decreased with induced hypotension (Fig. 4). Baseline TAV was 9.7 ± 3.4 cm/s and during hypotension, 3.5 ± 2.5 cm/s (p = 0.002). Analysis of covariance between the NIRS-determined HbD changes and the Doppler-determined TAV changes showed a significant correlation of HbD and TAV (p = 0.01) (Fig. 5).
Correlation of HbD and TAV throughout hypotensive episodes. Data points from multiple animals are shown. Regression lines corresponding to each animal's data points are also shown. Absolute values of TAV vary between animals due to differences in blood vessel diameter and relative baseline flow velocities. However, HbD and TAV are highly correlated for each animal (r2 range 0.64-0.90).
DISCUSSION
NIRS is a noninvasive monitoring technique that can provide bedside assessments of cerebral Hbo2 and Hb levels (12). Quantitative determinations of the changes in these two substances can be made continuously with this methodology. This study suggests that NIRS is able to detect changes in CBF induced by hypotension.
Hypotension in this piglet model to a MAP of less than 50% of baseline was associated with a corresponding decrease in CBF measured by the radioactive microsphere technique. The rapid and severe decreases in blood pressure most likely exceeded the ability of the animals to maintain CBF by cerebral vasodilation, thereby resulting in proportional decreases in cerebral perfusion. Under these conditions, NIRS measurements of cerebral intravascular oxygenation, as assessed by the HbD signal also decreased significantly.
Doppler ultrasound measurements of CBF velocity in the anterior cerebral arteries were conducted during separate hypotensive episodes to assess more closely the temporal coupling of HbD, MAP, and CBF velocity. During hypotensive episodes, HbD decreased in parallel with declines in MAP and CBF velocity. Flow velocity in a cerebral artery of fixed caliber is proportional to CBF in the brain tissue perfused by that artery. Doppler velocity measurements of the anterior cerebral arteries have been shown to correlate with CBF (13). Hence, we believe that decreases in cerebral perfusion caused by hypotension can be detected by NIRS as a decrease in cerebral intravascular oxygenation.
Cerebral blood volume, as assessed by the HbT signal, showed a smaller, less significant decrease with hypotension. HbT has shown some correlation with CBF in previous NIRS studies (14). Changes in HbT are largely indicative of changes in cerebral blood volume (8,15). If CBF increases due to cerebral arterial vasodilation, cerebral blood volume will also increase. However, changes in CBF that are caused largely by changes in CBF velocity may not produce significant changes in cerebral blood volume. In addition, slowing of flow velocity due to venous congestion will result in decreased CBF but increased cerebral blood volume. Hence, HbD may be a more sensitive indicator of CBF than HbT.
The correlation of HbD with CBF is physiologically plausible. If cerebral arterial oxygen saturation and cerebral metabolic rate for oxygen are constant, changes in CBF will produce decreases in cerebral venous oxygen saturation by the Fick principle. Because NIRS is sensitive to all vascular compartments, and venous blood is approximately 80% of total cerebral blood volume (16), HbD will be highly sensitive to changes in cerebral venous oxygen saturation. Therefore, HbD is expected to vary with CBF during periods of constant cerebral arterial oxygen saturation and oxygen consumption.
The observed decreases in HbD are unlikely to be a result of altered arterial oxygenation. During hypotensive episodes, inspired oxygen concentration and mechanical ventilation parameters were held constant at levels sufficient to highly saturate arterial hemoglobin (arterial Po2 > 90 mm Hg). Although we did not measure arterial oxygen saturation continuously, NIRS measurements in human infants have also shown correlation between HbD and MAP during periods of constant arterial oxygen saturation as measured by pulse oximetry (4). Similarly, altered cerebral oxygen consumption is unlikely to explain the observed changes in HbD because other than MAP, experimental conditions were held constant (e.g. anesthetic dose, temperature).
The ability to preserve CBF during hypotensive episodes is known to vary in different regions of the brain (1,2). Regions farthest from major arterial vessels are more vulnerable to ischemia, and brainstem CBF is better preserved than is cortical CBF. Although our NIRS instrument does not provide spatially resolved data, the optode configuration used should sample mainly from the cerebral hemispheres (17). Hence, we believe that the changes in HbD observed do correspond to the measured values for CBF taken from the cerebral hemispheres and the Doppler ultrasound data measured from the anterior cerebral arteries. The recent development of spatially resolved NIRS measurements may allow regional assessment of cerebral ischemia induced by hypotension (18).
The current study and our premature infant NIRS study were conducted with a continuous wave NIRS instrument that cannot quantitate path length directly. Although path length is constant for any given study subject after optodes are applied (10), the inability to quantitate path length prevents absolute quantitation of Hbo2 and Hb concentrations. Newer NIRS instruments currently under development and evaluation are likely to overcome this limitation. Instruments based on phase-modulated spectroscopy and time-of-flight spectroscopy may allow quantitation of global cerebral hemoglobin oxygen saturation (12,18–20). HbD is proportional to global cerebral hemoglobin oxygen saturation. Hence these newer instruments should also detect changes in cerebral oxygenation caused by hypotension-induced decreases in CBF. Quantitation of cerebral hemoglobin oxygen saturation would allow development of normative data for different populations of patients and comparison of NIRS data during different recording sessions or on different patients. Continuous measurement of global cerebral hemoglobin oxygen saturation by NIRS could thus provide rapid warning of cerebral ischemia during blood pressure fluctuations, and help guide therapeutic interventions.
Abbreviations
- CBF:
-
cerebral blood flow
- MAP:
-
mean arterial blood pressure
- TAV:
-
time average mean velocity
- NIRS:
-
near infrared spectroscopy
- dpf:
-
differential path length factor
- Hbo2:
-
oxygenated hemoglobin
- Hb:
-
deoxygenated hemoglobin
- HbT:
-
total hemoglobin
- HbD:
-
hemoglobin difference signal
REFERENCES
Pryds O 1991 Control of cerebral circulation in the high-risk neonate. Ann Neurol 30: 321–329
Volpe JJ 1995 Neurology of the Newborn, 3rd Ed. WB Saunders, Philadelphia, 297–298.
Lou HC, Lassen NA, Friis-Hansen B 1979 Impaired autoregulation of cerebral blood flow in the distressed newborn infant. J Pediatr 94: 118–121
Tsuji M, duPlessis A, Eichenwald E, Naruse H, Volpe J 1995 Cerebral oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatr Res 37: 241A( abstr)
Heymann MA, Payne BD, Hoffman JIE, Rudolph AM 1977 Blood flow measurements with radionuclide-labeled particles. Prog Cardiovasc Dis 20: 55–79
Faris F, Thorniley M, Wickramsinghe Y, Houston R, Rolfe P, Livera N, Spencer A 1991 Non-invasive in vivo near-infrared optical measurement of the penetration depth in the neonatal head. Clin Phys Physiol Meas 12: 353–358
Wray S, Cope M, Delpy DT, Wyatt JS, Reynolds EOR 1988 Characterization of the near infrared absorption spectra of cytochrome aa3 and haemoglobin for the non-invasive monitoring of cerebral oxygenation. Biochim Biophys Acta 933: 184–192
Wyatt JS, Cope M, Delpy DT, Wray S, Reynolds EO 1986 Quantification of cerebral oxygenation and haemodynamics in sick newborn infants by near infrared spectrophotometry. Lancet 2: 1063–1066
Van der Zee P, Delpy DT 1988 Methods of quantitating cerebral near infrared spectroscopy data. Adv Exp Med Biol 222: 183–189
Wyatt JS, Cope M, Delpy DT, Van der Zee P, Arridge S, Edwards AD, Reynolds EOR 1990 Measurement of optical pathlength for cerebral near-infrared spectroscopy in newborn infants. Dev Neurosci 12: 140–144
Delpy DT, Cope M, Van der Zee P, Arridge S, Wray S, Wyatt JS 1988 Estimation of optical pathlength through tissue direct time of flight measurement. Physics Med Biol 33: 1433–1442
Tsuji M 1996 Cerebral monitoring by near infrared spectroscopy. J Intensive Care Med 11: 162–172
Taylor GA, Short BL, Walker LK, Traystman RJ 1990 Intracranial blood flow: quantification with duplex Doppler and color Doppler flow US. Radiology 176: 231–236
Pryds O, Greisen L, Skov L, Friis-Hansen B 1990 Carbon dioxide-related changes in cerebral blood volume and cerebral blood flow in mechanically ventilated preterm neonates: comparison of near infrared spectrophotometry and xenon 133 clearance. Pediatr Res 27: 445–449
Brazy JE, Lewis DV 1986 Changes in cerebral blood volume and cytochrome aa3 during hypertensive peaks in preterm infants. J Pediatr 108: 983–987
Mchedlishvili G 1986 Cerebral arterial behavior providing constant cerebral blood flow, pressure, and volume. In: Bevan JA (ed) Arterial Behavior and Blood Circulation in the Brain. Plenum Press, New York, 42–95.
Tsuji M, Naruse H, Volpe J, Holtzman D 1995 Reduction of cytochrome aa3 measured by near-infrared spectroscopy predicts cerebral energy loss in hypoxic piglets. Pediatr Res 37: 253–259
Benaron DA, Stevenson DK 1993 Optical time-of-flight and absorbance imaging of biologic media. Science 259: 1463–1466
Benaron DA, Benitz WE, Ariagno RL, Stevenson DK 1992 Noninvasive methods for estimating in-vivo oxygenation. Clin Pediatr 31: 258–273
Wilson BC, Sevick EM, Patterson BC 1992 Time-dependent optical spectroscopy and imaging for biomedical applications. Proc IEEE 80: 918–930
Acknowledgements
The authors thank Mark Cioffi and Milan Stankovic for technical assistance.
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health Research Grants NS32570 and HD18655 (J.J.V), HD01010 (M.T.), and NS01721 (A.D). The near infrared spectroscopy instrument was provided by Hamamatsu Photonics, KK, Hamamatsu, Japan.
Rights and permissions
About this article
Cite this article
Tsuji, M., Duplessis, A., Taylor, G. et al. Near Infrared Spectroscopy Detects Cerebral Ischemia during Hypotension in Piglets. Pediatr Res 44, 591–595 (1998). https://doi.org/10.1203/00006450-199810000-00020
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199810000-00020
This article is cited by
-
Watching synchronous mitochondrial respiration in the retina and its instability in a mouse model of macular degeneration
Scientific Reports (2021)
-
Epinephrine’s effects on cerebrovascular and systemic hemodynamics during cardiopulmonary resuscitation
Critical Care (2020)
-
Cerebral venous volume changes and pressure autoregulation in critically ill infants
Journal of Perinatology (2020)
-
Validation of Near-Infrared Spectroscopy for Monitoring Cerebral Autoregulation in Comatose Patients
Neurocritical Care (2017)
-
Baroreflex dysfunction in sick newborns makes heart rate an unreliable surrogate for blood pressure changes
Pediatric Research (2016)