Abstract
Although a strong clinical association exists between congenital heart block (CHB) and an immune response to SSA/Ro and SSB/La proteins, a causative role of these antibodies in the pathogenesis is just emerging. In a preliminary report, we have demonstrated that IgG fractions isolated from the sera of mothers whose children have CHB are arrhythmogenic in the human fetal heart. To more precisely define the arrhythmogenic effect of anti-SSA/Ro-SSB/La antibodies, we used the readily available rat heart model to record: 1) ECGs from Langendorff beating hearts;2) action potentials from atrioventricular (AV) nodal preparations;3) L-type Ca currents, ICa at the whole-cell and single channel levels; and 4) other currents such as the transient outward K+ current,Ito, the inward rectifier K+ current,IK1, and the Na+ current,INa. Perfusion of hearts with purified IgG (800 µg/mL), isolated from the serum of a mother with SSA/Ro and SSB/La antibodies whose child had CHB, resulted in bradycardia associated with 2:1 AV block. Simultaneous action potentials were recorded from dissected atrial and AV nodal areas of the rat heart. Superfusion of these preparations with the same mother's IgG fraction resulted in 2:1 AV block followed by complete inhibition of AV nodal action potential. Because AV nodal electrogenesis is largely dependent on ICa, the effect of these antibodies on ICa was subsequently determined. Superfusion of myocytes with whole serum or purified IgG (80 µg/mL) from the same mother consistently inhibited whole cell ICa, ensemble average Ba2+ currents (IBa) and open state probability, po, without affecting the channel conductance. IgG had no significant effect on Ito,IK1, or INa. Whole sera and IgG fractions from a healthy mother with no detectable anti-SSA/Ro or SSB/La antibodies did not inhibit ICa or IBa. These results demonstrate that IgG containing anti-SSA/Ro and -SSB/La antibodies induces complete AV block in beating hearts and in multicellular preparations, thus implicating a preferential interaction of these autoantibodies with Ca channels and/or associated regulatory proteins. This is consistent with the observed inhibition of Ca channels that may be a critical factor contributing to the pathogenesis of CHB.
Similar content being viewed by others
Main
AV block, detected at or before birth in a structurally normal heart, is strongly associated with autoantibodies reactive with the intracellular soluble ribonucleoproteins 48-kD SSB/La, 52-kD SSA/Ro, and 60-kD SSA/Ro(1). CHB is presumed to be due to the transplacental passage of these IgG autoantibodies from the mother (who may have systemic lupus erythematosus, Sjogren's syndrome, or be entirely asymptomatic) into the fetal circulation(2). In addition to cardiac manifestations, other neonatal abnormalities affecting the skin, liver, and blood elements are also associated with anti-SSA/Ro and -SSB/La antibodies in the maternal and fetal circulation and are grouped under the heading of neonatal lupus syndromes (reviewed inRefs 3 and 4). Neonatal lupus was so termed because the cutaneous lesions of the neonate resembled those seen in systemic lupus erythematosus. To date, complete AV block is irreversible, although varying degrees of block have been noted, and second degree block has on rare occasion reverted to normal sinus rhythm(5). However, the noncardiac manifestations of neonatal lupus are transient, resolving at about 6 mo of life coincident with the disappearance of maternal autoantibodies from the neonatal circulation(3).
Our laboratory and others have molecularly characterized the maternal autoantibody responses(1,6–10) and cloned the genes expressing the cognate antigens. The 60-kD SSA/Ro contains an RNA-binding protein consensus motif(11,12), which could account for its direct interaction with small cytoplasmic hY-RNAs(13). It has been suggested that 60-kD SSA/Ro may function as part of a novel quality control or discard pathway for 5 S rRNA production in Xenopus oocytes(14). Anti-SSB/La antibodies recognize a 48-kD polypeptide that does not share antigenic determinants with either 52- or 60 kD SSA/Ro(15,16). SSB/La facilitates maturation of RNA polymerase III transcripts, directly binds a spectrum of RNAs, and associates at least transiently with 60-kD SSA/Ro(17,18). In addition to the well characterized 60-kD SSA/Ro and 48-kD SSB/La autoantigens, another target of the autoimmune response in mothers whose children have CHB is the 52-kD SSA/Ro protein(19). The full-length protein, 52α, has three distinct domains, an N-terminal region rich in cysteine/histidine motifs containing two distinct zinc fingers known as RING finger and B-box; a central region containing two coiled coils with heptad periodicity, one being a leucine zipper with potential for intramolecular dimerization; and a C-terminal "rfp-like" domain(20,21).
Although the molecular aspects of CHB have received considerable emphasis, the electrophysiologic aspects of CHB have been explored only recently. Two earlier reports(22,23) demonstrated that sera from patients with lupus and anti-SSA/Ro antibodies (with or without anti-SSB/La antibodies)(22) and from mothers of children with CHB(23) induce complete AV block in Langendorff perfused hearts and inhibit L-type Ca channels. Accordingly, an in-depth systematic characterization of the electrophysiologic effects of maternal anti-SSA/Ro-SSB/La antibodies was undertaken to precisely define the cellular basis for their arrhythmogenicity. This was accomplished using the readily available rat heart model in which whole hearts, multicellular AV nodal preparations, and isolated single myocytes were studied. In addition, the effects of antibodies on three other currents, Ito,IK1, and INa, which contribute to the cardiac action potential, were evaluated.
METHODS
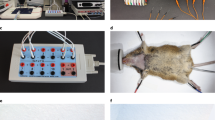
ECG recordings. Hearts were quickly removed from Wistar rats(200-250 g) and cannulated through the aorta for continuous perfusion of the coronary arteries with oxygenated (100% O2) Tyrode's solution at 37°C(23). Tyrode's solution contained (in mM): NaCl 117, KCl 5.7, CaCl2 1.8, NaHCO3 4.4, NaH2PO4 1.5, MgCl2 1.7, HEPES 20, glucose 11, creatine 10, and taurine 20. The pH was adjusted to 7.4 with NaOH. The hearts were then lowered into a double-jacketed beaker containing prewarmed Tyrode's solution. ECG tracings were obtained by conventional recording technique except for the use of silver wires (diameter ∼0.3 mm each) at the recording end of the leads(23). One wire was inserted in the right atrium, one in the left ventricle near the apex, and one in the Tyrode's solution (ground).
Action potential recordings. Modified Paes de Carvalho et al.(24) technique combined with the standard microelectrode technique(25) were used to record simultaneous action potentials(26) from the atria and AV nodal area. Briefly, the technique consists of quickly removing the heart from the chest and cutting the ventricles 5-7 mm below the AV groove. A round-edged steel cannula was inserted from the right ventricle through the superior vena cava. An incision was then performed along the cannula. The preparation was opened face up and pinned in the tissue bath to expose the sinus node, the crista terminalis, the AV nodal area, and part of the ventricle. The AV nodal area was recognized by its location between the tricuspid valve and the coronary sinus(27). The preparation was superfused with Tyrode's solution and allowed to recover for 30 min. Standard glass microelectrodes filled with 3 M KCl were used to record simultaneous action potentials(26) from the right atria and the AV node.
IgG purification. The isolation of total IgG was done using the ImmunoPure IgG purification kit (Pierce, Rockford, IL) according to the manufacturer's instructions. Sera were diluted 1:1 with ImmunoPure IgG binding buffer (pH 8) and applied to protein A columns. Protein A columns were then washed with 15 mL of the binding buffer. Elution of bound IgG was accomplished with elution buffer (pH 2.8), and the protein concentration was monitored by absorbance at 280 nm. Fractions with the highest absorbance were pooled and applied to an excellulose desalting column. Washes were done in PBS (pH 7.4). Fractions were again pooled, and quantification of the total IgG was done by nephelometry. Purity of the IgG preparations was verified by electrophoresis of the samples on 15% high ratio monomer:cross-linker acrylamide gels under reducing conditions. Coomassie Blue staining confirmed the presence of only two bands, one at 50 kD and one at 25 kD, representing the heavy and light chains, respectively. Throughout this study, we chose to characterize serum and IgG from one mother whose child had CHB. Her serum was known to contain 48-kD SSB/La, 52-kD SSA/Ro, and 60-kD SSA/Ro by immunoblot. In the "Results," this patient's serum is referred to as the positive serum and her IgG fraction as positive IgG. The concentrations of IgG used in this study were based on a previously published report(23). As a control, serum and purified IgG from a healthy mother with healthy children were used. This serum and IgG tested negative for anti-SSA/Ro and anti-SSB/La antibodies by ELISA and immunoblot and thus were called negative serum and negative IgG, respectively.
Isolation of cardiac myocytes. Cardiac myocytes were obtained from hearts of Wistar rats (200-250 g) by enzymatic dissociation as previously described(28,29). The heart was perfused with a HEPES-buffered solution containing (in mM): NaCl 117, KCl 5.7, NaHCO3 4.4, NH2PO4 1.5, MgCl2 1.7, HEPES 20, glucose 11, creatine 10, taurine 20, and 21 mU/mL insulin, and the pH was adjusted to 7.4 with NaOH. The heart was then perfused with fresh buffer mixed with 1.5 mg/mL collagenase type A or B (Boehringer Mannheim, Indianapolis, IN) and 20 µM Ca2+ for 40-50 min. The ventricles were then cut off and stirred to obtain cells. Cells were suspended in Petri dishes containing HEPES buffer with 1 mM CaCl2 and 0.5% BSA (pH 7.4). All solutions used for perfusion were gassed with 100% O2 and warmed to 37°C. After incubation for 30 min, a small aliquot of the medium containing single cells was transferred to a chamber mounted on the stage of an inverted microscope (Nikon Inc., Tokyo, Japan). Rod-shaped, noncontracting cells with clear striations were used for the whole cell voltage clamp studies. All experiments were carried out at temperatures of 22-24°C.
Solutions and drugs. The composition of external solutions to record whole cell L-type Ca current, ICa(29) in (mM): NaCl 132, CsCl 5.4, CaCl2 1.8, MgCl2 1.8, NaH2PO4 0.6, 4-amino-pyridine 5, HEPES 10, dextrose 5, Na-pyruvate 5, pH 7.4. Patch electrodes were filled with control internal solution containing (in mM): CsCl 139.8, potassium EGTA 10, MgCl2 4, CaCl2 0.062, Na2-creatine phosphate 5, HEPES 10, Na2 ATP 3.1, Na2GTP 0.42, adjusted to pH 7.1 with KOH. For single channel recording(28), the bath solution contained (in mM): potassium glutamate 120, KCl 25, MgCl2 2, ATP 1, EGTA 2, HEPES 10, pH 7.4 adjusted with KOH. The pipette solution contained (in mM): BaCl2 70, sucrose 110, HEPES 10, pH 7.4 adjusted with TEA-OH.
Electrophysiology. The whole cell and cell-attached configuration of the patch-clamp technique was used(28–30). To record L-type ICa, all potassium currents were blocked with intracellular and extracellular Cs2+ and 4-aminopyridine(23,29). The fast Na current was blocked by a prepulse to -50 mV from a holding potential of -80 mV in the presence of tetrodotoxin (50 µM) to eliminate any residual INa. Cells were depolarized every 10 s from a holding potential of -80 mV to a prepulse level of -50 mV for 100 ms and subsequently to a test pulse of 0 mV for 300 ms. For potassium current recordings, NaCl was replaced by choline-Cl in the external solution to eliminate INa(31). Because only L-type Ca current (ICa) was found(29) and reported by others(32) in adult rat ventricular cells, the Ca channel blocker, nisoldipine (2 µM), was added to the external solution(31). The transient outward potassium current,Ito, was evoked by depolarizing pulses to 40 mV for 400 ms from a holding potential of -100 mV every 10 s(31). The inward rectifier K current (IK1) was recorded at hyperpolarized voltages from -40 to -140 mV(31). The fast Na current, INa, was recorded from holding potentials of-100 or -80 mV to depolarizing pulse of -30 and -20 mV for 50 ms every 5 s whereas K channels are blocked by Cs2+ (in and out of the cell) and Ca currents by 5 mM cobalt.
A programmable horizontal puller (model P-87, Sutter Instrument Co., Novato, CA) was used to pull the electrodes. The volume of the recording chamber was 0.5 mL, and the rate of superfusion was 3 mL/min. The junction potential was always compensated and was smaller than 5 mV. Membrane currents were recorded using a Dagan model 3900A patch clamp amplifier (Dagan Corp., Minneapolis, MN). Capacitive currents were elicited by a 10-mV depolarizing pulse from -80 mV and then compensated. Later on, the capacitive traces were fitted by a single exponential equation, and Cm was calculated according to the equation Cm =τc·Io/ΔEm, where Cm is the membrane capacitance, τc is the time constant for cell membrane charge, Io is the maximum capacitive current and ΔEm is the clamp voltage. The average Cm was 146.5 ± 69.4 pF (n = 84). Single channel recording was performed as previously described(28). Briefly, unitary currents were evoked by a 300-ms step depolarization to 0 mV from a holding potential of -50 mV at 0.5 Hz. Analysis of unitary currents was performed after digital subtraction of capacitive and leakage currents by averaging records without channel openings and subtracting the average from each record in the series. Measurements of open and closed times were made at 0 mV, and patches exhibiting more than one open channel current level were not included in the analysis. The ensemble mean current was obtained by averaging all subtracted current records of the series. The open-state probability (po) was determined by integrating over each sweep.
Data analysis. Membrane currents were digitally recorded and analyzed using pCLAMP software (Version 6.0.1, Axon Instruments Inc., Foster City, CA). Origin (Microcal Origin v3.7, Microcal Software Inc.) programs were used to generate figures. Data are presented as mean ± SEM. t test for paired data were used to compare control conditions with antibody treatment. A p value of <0.05 was considered statistically significant.
RESULTS
Positive IgG-induced conduction abnormalities in Langendorff perfused hearts. Figure 1 illustrates the effect of positive IgG on the ECG recording of an isolated rat heart perfused by the Langendorff technique. Recordings were done using a conventional ECG machine in lead I. Fig. 1A shows regular sinus rhythm (horizontal scale, 50 mm/s; vertical scale, 5 mm/mV) at 300 beats/min in Tyrode's solution. After 5 min of perfusion with positive IgG (800 µg/mL), there was bradycardia associated with 2:1 second degree AV block(Fig. 1B) that degenerated into complete AV block at about 15 min of perfusion (Fig. 1C). The QRS complex is absent but the P waves (indicated by the arrows) can be clearly seen. After 25 min of reperfusion with Tyrode's solution, only partial recovery was seen (Fig. 1D). Identical results were obtained in four separate experiments. In contrast, perfusion of the rat heart with negative IgG did not induce any conduction abnormalities(n = 4).
Effects of maternal antibodies on ECG recordings of isolated rat heart perfused by the Langendorff technique. ECG was recorded by the conventional ECG machine in lead I, except for the use of silver wires (diameter ≈ 0.3 mm each) at the recording end of the leads. One lead was inserted in the atrium, the second in the left ventricle near the apex, and the third in Tyrode's solution (ground). (A) Regular sinus rhythm (horizontal scale, 50 mm/s and vertical scale: 5 mm/mV) at 300 beats/min in Tyrode's solution. After 5 min of perfusion with positive IgG(800 µg/mL), there was bradycardia associated with a 2:1 second degree AV block (B) that degenerated into complete AV block by 15 min of IgG perfusion (C). Return to Tyrode's solution, resulted in only partial recovery (D). Arrows indicate the P waves.
Positive IgG induced complete AV block in the AV node multicellular preparation. Induction of AV block in the whole heart by positive IgG suggests that conduction abnormalities should be reproduced in an AV nodal preparation. Therefore, the effects of positive IgG (800µg/mL) were then tested in spontaneously beating (180.5 ± 45.6 beats/min, n = 4) AV nodal preparations. Figure 2 demonstrates a representative recording in which the simultaneous action potential from the crista terminalis(Fig. 2A, upper tracing) and AV nodal area(lower tracing) were obtained without the addition of any IgG. Note the triangular shape of the action potential from the crista terminalis and the slow action potential with a phase 4 from the AV node area. Superfusion of the preparation with positive IgG for approximately 10 min resulted in 2:1 AV block indicated by the arrows. Longer IgG superfusion (10-15 min) resulted in almost complete inhibition of the AV node-action potential (Fig. 2B, bottom trace). These results are consistent with the ECG findings from the whole heart. Conduction abnormalities were not seen with negative IgG (n = 3).
Effects of maternal antibodies on an isolated multicellular AV nodal preparation. (A) Simultaneous control action potentials from the crista terminalis (upper tracing) and the AV node area (lower tracing). (B) Superfusion of the preparation with positive IgG (800 µg/mL) for 10 min resulted in 2:1 AV block (indicated by the arrows) which progressed to near complete inhibition of the AV node action potential by 15 min (B, bottom). Note the time scale difference between(A) and (B).
Positive IgG inhibited L-type Ica. Because conduction at the AV node is essentially dependent on Ca electrogenesis(33,34), the next logical approach was to test the effect of positive IgG on L-type Ca current. Positive IgG fractions (80µg/mL) significantly inhibited ICa (57.5 ± 12.6%, p < 0.05, n = 6).Figure 3 shows the time course of the ICa inhibition (A) and the current-voltage relations (B) during control and steady-state effect of 80µg/mL positive IgG. IgG resulted in 62% inhibition of ICa at 0 mV, and its effects were only partially reversible. However, negative IgG (80 µg/mL) induced no significant changes on ICa (Fig. 4).
Effects of maternal antibodies (IgG) on L-type ICa recorded from rat ventricular myocytes. (A) The time course of ICa inhibition by positive IgG (80µg/mL). IgG reduced ICa from 2057 to 765 pA (at 0 mV). Washout was only partial. (B) The current-voltage relations during control and after cell superfusion with positive IgG. Current-voltage relations of peak ICa were recorded every 8 s by a series of depolarizing pulses to -50 through 60 mV with 10-mV increments. IgG decreased ICa and scaled down the current-voltage relations.
Effects of negative IgG on L-type ICa recorded from a rat ventricular myocyte. IgG (80µg/mL), from a healthy female donor known to have healthy children and no circulating autoantibodies had no effect on L-type ICa. Two selected ICa tracings recorded during control and steady-state effect of negative IgG are shown.
Positive serum inhibited L-type Ica. The effects of positive and negative whole serum on ICa were also tested. Similar to IgG, positive serum (80 µg/mL) inhibited ICa at all voltages tested (Fig. 5A). For example, the average inhibition of ICa was 61.7± 9.5% (p < 0.05, n = 8). In contrast, negative serum had no significant effect on ICa (8.5± 3.4%, n = 5) as shown in Figure 5B.
Effects of maternal serum on L-type ICa recorded from rat ventricular myocytes. (A and B) Steady-state effect of positive and negative serum (80µg/mL) on current-voltage relations of ICa, respectively. Positive IgG inhibited ICa at all voltages. Selected tracings during control and after inhibition of ICa are shown in the inset. Negative serum had no significant effect on ICa, at all voltages. Selected tracings are shown in the inset.
Positive IgG inhibited single Ca channels. To gain insights into the biophysical mechanism(s) by which anti-SSA/Ro-SSB/La antibodies inhibit Ca currents, the effects of positive IgG were tested on unitary Ba2+ currents. Single channel currents were recorded in cell-attached configuration of the patch-clamp method(28,30). Depolarizing test pulses to 0 mV from holding potential of -50 mV elicited inward unitary currents in the presence of intrapipette Ba2+ (70 mM) as a charge carrier. These unitary currents were seen at potentials positive to-30 mV and were blocked by the Ca channel blocker, nisoldipine (2 µM)(28,23). Figure 6 shows unitary Ba2+ current sweeps during control and after addition of the positive IgG (80 µg/mL). Ensemble averaged currents were obtained from 170 and 161 consecutive tracings during control and positive IgG, respectively. IgG decreased peak ensemble averaged Ba2+ current by 47%. IgG produced a pronounced decrease in Ca channel activity. During control (absence of IgG), 69% of sweeps showed channel opening. In the presence of IgG, only 58% of sweeps exhibited channel activity. The open state probability calculated from all current sweeps was decreased by positive IgG from 0.095 ± 0.021 to 0.042 ± 0.015 (n = 6, p < 0.05). The analysis of open-close kinetics of the Ca channels was performed to produce histograms. In the control conditions, both the open and closed time histograms were best fitted by 2 exponentials(28). Open time fast and slow components values were 0.56 ± 0.05 ms and 7.2± 1.1 ms during control and 0.44 ± 0.05 ms and 4.2 ± 0.3 ms after positive IgG, respectively. Close time fast and slow components values were 1.0 ± 0.2 ms and 10.3 ± 0.7 ms during control and 1.0 ± 0.1 and 19.3 ± 1.5 ms after positive IgG, respectively. Positive IgG significantly (p < 0.05) accelerated the slow time constant of open time histogram and lengthened the slow time constant of closed time histogram. Figure 7, A and B, illustrates such effects. The shortening of the open time constant and the lengthening of the slow component of closed time may in part explain the inhibition of the whole cell ICa by the autoantibodies. Positive IgG did not affect the channel conductance as shown in Fig. 7C(27.5 ± 0.4 during control and 27.0 ± 0.5 after positive IgG). Negative IgG did not affect the kinetics of IBa.
Elementary currents through a single Ca channel recorded from a rat ventricular myocyte. The pipette contained 70 mM BaCl2. Single Ca channel activity was elicited by consecutive 300-ms depolarizing pulses to 0 mV from a holding potential of -50 mV. Linear leak and capacity currents were subtracted. (A and B) Ten consecutive current tracings in the absence (control) and presence of positive IgG (80 µg/mL). The bottom tracings show the ensemble average current obtained from the average of 170 sweeps during control (left panel) and 161 sweeps in the presence of positive IgG (right panel).
Histograms of the open times, closed times, and the conductance of the Ca channel. The same patch was used to generate histograms during control (A), and IgG (80 µg/mL,B) in a rat ventricular myocyte. The data were collected from 200 sweeps for each histogram and were best fitted by the sum of two exponential components, fast (τf) and slow (τs). Open event durations were binned at 0.2 ms. (C) Channel conductance during control and after IgG (80 µg/mL). Channel conductance was measured from the slope of the relationship between single channel current amplitude and membrane potential during step depolarizations between -20 to 10 mV. Unitary current amplitudes varied with applied potentials, the current-voltage relationship being linear with a channel conductance of 27.7 pS during control and 27.6 pS with IgG.
Positive IgG had no effect on Ito, IK1, and INa. Because currents other than ICa contribute to the action potential generated in the heart, the effects of positive IgG on the transient outward current, Ito, the inward rectifier,IK1, and the fast Na current,INa, were studied. As shown in Figure 8A, there was no effect of positive IgG (80µg/mL) on Ito at three selected potentials of 50, 60, and 70 mV. Figure 8B shows current-voltage relations of Ito generated by applying 12 depolarizing pulses from a holding potential of -80 to -20 through 70 mV for 800 ms with 10-mV increments. The amplitude of Ito was normalized by cell capacitance at each voltage and the average data from six experiments was plotted as a function of the depolarizing voltages.
Effect of positive IgG on transient outward current, Ito recorded from rat ventricular myocytes. (A) Ito tracings recorded by the protocol shown on top, during control and steady-state effect of positive IgG(80 µg/mL). (B) Current-voltage relations of peak Ito, during control and after steady-state effect of IgG. Positive IgG had no significant effect on Ito.
Hyperpolarization to -150 mV from a holding potential of -40 produced a time-independent inward current, IK1, which was blocked by CsCl2(31). Figure 9A shows two IK1 tracings recorded at -90 mV and -120 mV during control and steady-state effect of positive IgG (80 µg/mL). As observed with Ito, positive IgG did not alter IK1 at voltages between -40 to -150 mV (Fig. 9B).
Effect of positive IgG on inward rectifier K current, IK1 recorded from rat ventricular myocytes. (A) Two selected IK1 tracings at -90 and -120 mV during control and steady-state effect of IgG (80 µg/mL).(B) Current-voltage relations of peak IK1, during control and steady-state effect of IgG. Positive IgG did not alter IK1.
Figure 10 shows that positive IgG (80 µg/mL) also had no effect on INa in a cell that was depolarized every 5 s to -20 mV from a holding potential of -80 mV. The corresponding tracings shown in Fig. 10 were obtained in the presence of 5 mM cobalt to block ICa; K+ has been replaced in and out of the cell by CsCl2.
DISCUSSION
The data presented in this study consistently demonstrated that whole serum and IgG fractions, isolated from a mother known to have anti-SSA/Ro and anti-SSA/La antibodies and a child with CHB, significantly inhibited whole cell and single unitary L-type Ca channels. Analysis of single channel kinetics indicates that this inhibition was the result of shorter open times, longer closed times, and decreased channel availability. This could, in part, explain the basis of the whole cell ICa inhibition by the autoantibodies. These findings correlate with the ECG and the microelectrode data and could account for the conduction abnormalities seen in vitro, thereby providing a cellular and ionic basis for the arrhythmogenicity of the antibodies. In contrast, this same IgG fraction did not alter Ito, IK1, and INa further indicating that Ca channels and/or associated regulatory proteins are the primary ion channel target for the maternal autoantibodies. These results establish a strong functional association of autoantibodies with Ca channels and are consistent with previous reports(22,23).
Relation to previous work. Garcia et al.(22) demonstrated that perfusion of adult rabbit hearts with IgG from anti-SSA/Ro positive sera resulted in heart block. One serum, which induced heart block, also contained anti-SSB/La antibodies. Curiously, the degree of block progressed over time despite removal of the antibodies. It is intriguing that postnatal progression of AV block from second to third degree has been reported in one case of neonatal lupus(35). Consistent with the results reported herein, Garcia et al.(22) also observed that anti-SSA/Ropositive sera induced a reduction in ICa of isolated rabbit ventricular myocytes. Because conduction in the AV node is essentially dependent on Ca electrogenesis, AV block would be expected to result from treatments leading to reduction in the ICa. L-type Ca channels are largely responsible for the propagation of the action potential in the AV node and are present in ventricular myocytes, thus supporting the view that results obtained in isolated ventricular myocytes correlate with those obtained using the whole heart. These findings suggest a direct interaction between the autoantibodies and Ca channel proteins and/or an indirect association with Ca channels via recognition of regulatory proteins such as previously described for neutransmitter receptors(36), resulting in perturbation of transmembrane signaling and Ca fluxes across the membrane.
It is noteworthy that normal IgG lacking anti-Ro/SSA and anti-La/SSB antibodies did not affect Ca channels, suggesting that it is unlikely that other unidentified components of IgG may contribute to the observed effects. However, because we did not use affinity-purified antibodies in this study, we cannot completely rule out the contribution of unidentified components of IgG (containing anti-Ro/SSA and anti-La/SSB antibodies) in the observed effects.
Autoantibodies and pathogenesis. Although the association of autoantibodies with CHB is widely accepted, the precise mechanism by which these antibodies cause cardiac conduction abnormalities remains to be defined. Several explanations have been proposed. The initial lesion may be a global pancarditis with inflammation of the pericardium, myocardium, and endocardium resulting in subsequent fibrosis of the conducting system clinically manifest as permanent heart block. An inflammatory component is supported by the finding of a mononuclear cell infiltration in the myocardium of a fetus dying in utero at 18 wk of gestation(37) and the demonstration of patchy lymphoid aggregates throughout the myocardium of an infant delivered at 30 wk and dying in the immediate postnatal period(38). Moreover, immunofluorescent studies have shown deposition of IgG, complement (including C1q, C4, C3d, C6, and C9), and fibrin(38,39). Litsey et al.(39) identified IgG deposits in the epicardial, myocardial, and endocardial tissue of the right atrium on postmortem analysis of a neonate with CHB. Specific vulnerability of the conducting system with virtual replacement of the AV node by varying degrees of fibrosis and fatty tissue in some autopsy studies is unexplained(40).
Albeit published literature on serial echocardiograms in mothers at high risk of a pregnancy complicated by CHB is limited to nonexistent, it has been the general experience that the first clinically detectable abnormality in cardiac function is not myocarditis (i.e. effusions and/or, ventricular dysfunction) but bradycardia. This infers that early inflammation is not clinically detectable and/or AV nodal injury occurs independent of an inflammatory pancarditis. It is presently unknown whether the antibodies have several pathologic effects with one being the interference with Ca channels. Prolonged exposure of fetal cardiac Ca channels to maternal antibodies could result in down-regulation of these channels by internalization, leading to cell death as suggested in other autoimmune diseases(41). This is supported by the fact that AV block is irreversible despite clearance of the maternal autoantibodies from the infant's circulation by 6-8 mo after birth.
Autoantibodies and sinus node. Although this study did not focus on determining the possible effects of autoantibodies on sinus node function, it is tempting to speculate that IgG from mothers of CHB children could also affect Ca channels and/or other currents responsible for the automaticity or action potential genesis at the sinus node. This is further supported by the data from the mouse model of CHB(23) where pups from mothers immunized with 52-kD recombinant protein and from mothers passively injected with human IgG from patients of affected children(manuscript in preparation); in both models significant sinus bradycardia was seen in addition to AV conduction abnormalities. Furthermore, clinical autopsy studies have shown abnormalities of the SA node in fetuses and neonates with CHB(40). Further work investigating the possible interaction of these antibodies with sinus node ion channels is necessary to clarify these hypotheses.
In summary, autoantibodies to components of SSA/Ro-SSB/La system are strongly, if not universally, present in isolated heart block detected at or before birth, which has greatly facilitated the identification of mothers at risk for this problem. However, there is no maternal antibody to a single component of this system which is unique to those whose children develop the disease. The target antigens are associated with RNA and not known to be expressed on cell surface membranes, raising issues of accessibility of antigen to cognate antibody. The study reported herein provides electrophysiologic evidence supporting causality and suggests that the maternal autoantibodies are not simply "clinical markers" of disease but truly pathogenetic. Serum and purified IgG from a mother whose child has CHB induced AV block both in an isolated Langendorff perfused heart and in multicellular AV nodal preparations. No arrhythmogenic effects could be demonstrated using serum and purified IgG from a normal volunteer with healthy children. These findings correlate with the inhibition of whole cell and single unitary calcium channel activity responsible for electrogenesis at the AV node. The putative Ca channel-blocking properties of the candidate autoantibodies and their induction of complete AV block in the whole heart provide a critical lead in a disease in which current available therapies are largely refractory.
Abbreviations
- AV :
-
atrioventricular
- CHB :
-
congenital heart block
- I Na :
-
sodium current
- I Ca :
-
L-type Ca current
- I to :
-
transient outward K current
- I K1 :
-
inward rectifier K current
References
Waltuck J, Buyon J 1994 Autoantibody-associated congenital heart block: outcome in mothers and children. Ann Int Med 120: 544–551.
Buyon JP, Winchester RJ 1990 Complete congenital heart block: a model of passively acquired autoimmunity. Arthritis Rheum 33: 609–614.
Buyon JP 1992 Neonatal lupus syndromes. In: Lahita R (ed) Systemic Lupus Erythematosus. Churchill Livingstone, New York, 419–435.
Lee LA 1990 Maternal autoantibodies and pregnancy. II. The neonatal lupus syndrome. In: Parke AL (ed) Bailliere's Clinical Rheumatology, Pregnancy and the Rheumatic Diseases. WB Saunders, Philadelphia 69–84.
Copel J, Buyon J, Kleinman C 1995 Successful in utero therapy of fetal heart block. Am J Obstet Gynecol 173: 1384–1390.
Buyon JP, Ben-Chetrit E, Karp S, Roubey RAS, Pompeo L, Reeves WH, Tan EM, Winchester R 1989 Acquired congenital heart block: pattern of maternal antibody response to biochemically defined antigens of the SSA/Ro-SSB/La system in neonatal lupus. J Clin Invest 84: 627–634.
Silverman ED, Mamula MJ, Hardin JA, Laxer RM 1991 The importance of the immune response to the Ro/La particle in the development of complete heart block and neonatal lupus erythematosus. J Rheumatol 18: 120–124.
Lee LA, Frank MB, McCubbin VR, Reichlin M 1994 The autoantibodies of neonatal lupus erythematosus. J Invest Dermatol 102: 963–966.
Julkunen H, Siren MK, Kaaja R, Kurki P, Friman C, Koskimies S 1995 Maternal HLA antigens and antibodies to SS-A/Ro and SS-B/La. Comparison with systemic lupus erythematosus and primary Sjogren's syndrome. Br J Rheumatol 34: 901–907.
Brucato A, Franceschini F, Gasparini M, De Juli E, Ferraro G, Quinzanini M, Vignati G, Bortolon C, Ghessi A, Possoli R 1995 Isolated congenital complete heart block: longterm outcome of mothers, maternal antibody specificity and immunogenetic background. J Rheumatol 22: 533–540.
Deutscher SL, Harley JB, Keene JD 1988 Molecular analysis of the 60 kD human Ro ribonucleoprotein. Proc Natl Acad Sci USA 85: 9479–9483.
Ben-Chetrit E, Gandy BJ, Tan EM, Sullivan KF 1989 Isolation and characterization of a cDNA clone encoding the 60-kD component of the human SS-A/Ro ribonucleoprotein autoantigen. J Clin Invest 83: 1284–1292.
Lerner MR, Boyle JA, Hardin JA, Steitz JA 1981 Two novel classes of small ribonucleoproteins detected by antibodies associated with lupus erythematosus. Science 211: 400–402.
O'Brien CA, Wolin SL 1994 A possible role for the 60 kD Ro autoantigen in a discard pathway for defective 5s rRNA precursors. Genes Dev 8: 2891–2903.
Chan EKL, Sullivan KF, Tan EM 1989 Ribonucleoprotein SS-B/La belongs to a protein family with consensus sequences for RNA-binding. Nucleic Acids Res 17: 2233–2244.
Chambers JC, Kenan D, Martin BJ, Keene JD 1988 Genomic structure and amino acid sequence domains of the human La autoantigen. J Biol Chem 263: 18043–18051.
Gottlieb E, Steitz JA 1989 Function of the mammalian La protein: evidence for its action in transcription termination by RNA polymerase III. EMBO J 8: 851–861.
Boire B, Craft J 1990 Human Ro ribonucleoprotein particles: characterization of native structure and stable association with the La polypeptide. J Clin Inv 85: 1182–1190.
Ben-Chetrit E, Chan EKL, Sullivan KF, Tan EM 1988 A 52 kD protein is a novel component of the SS-A/Ro antigenic particle. J Exp Med 162: 1560–1571.
Chan EKL, Hamel JC, Buyon JP, Tan EM 1991 Molecular definition and sequence motifs of the 52-kD component of human SS-A/Ro autoantigen. J Clin Invest 87: 68–76.
Itoh K, Itoh Y, Frank MB 1991 Protein heterogeneity in the human Ro/SSA ribonucleoproteins. J Clin Invest 87: 177–186.
Garcia S, Nascimento JHM, Bonfa E, Levy R, Oliveira SF, Tavares AV, Campos deCarvalho AC 1994 Cellular mechanism of the conduction abnormalities induced by serum from anti-Ro/SSA-positive patients in rabbit hearts. J Clin Invest 93: 718–724.
Boutjdir M, Chen L, Zhang Z, Tseng C, DiDonato F, Rashbaum W, Morris A, El-Sherif N, Buyon JP 1997 Arrhythmogenicity of IgG and anti-52 kD SSA/Ro affinity purified antibodies from mothers of children with congenital heart block. Circ Res 80: 354–362.
Paes de Carvalho A, De Mello W, Hoffman BF 1959 Electrophysiological evidence for specialized fiber types in rabbit atrium. Am J Physiol 196: 483–488.
Le Heuzey JY, Guize L, Valty J, Moutet JP, Kouz S, Lavergne T, Boutjdir M, Peronneau P 1986 Intracellular and extracellular recordings of sinus node activity: comparison with estimated sinoatrial conduction times during pacemaker shifts in rabbit heart. Cardiovasc Res 20: 81–88.
Boutjdir M, El Sherif N 1991 α1-Adrenoceptor regulation of delayed afterdepolarizations and triggered activity in subendocardial Purkinje fibers surviving 1 day of myocardial infarction. J Mol Cell Cardiol 23: 83–90.
Hancox J, Levi AJ, Lee CO, Heap P 1993 A method for isolating rabbit atrioventricular node myocytes which retain normal morphology and function. Am J Physiol 265:H755–H766.
Chen L, El-Sherif N, Boutjdir M 1996 α1-Adrenergic activation inhibits Beta-adrenergic stimulated unitary Ca current in cardiac ventricular myocytes. Circ Res 79: 184–193.
Zhang ZH, Johnson JA, El-Sherif N, Mochly-Rosen D, Boutjdir M 1997 C2 region-derived peptides of protein kinase C regulates cardiac Ca2+ channels. Circ Res 80: 720–729.
Hamill OP, Marty A, Neher E, Sakmann B, Sigworth FJ 1981 Improved patch-clamp techniques for high-resolution current recording from cell and cell-free membrane patches. Pflugers Arch 391: 85–100.
Zhang ZH, Boutjdir M, El-Sherif N 1994 Ketanserin inhibits depolarization-activated outward potassium current in rat ventricular myocytes. Circ Res 75: 711–721.
Scamps F, Legssyer A, Mayoux E, Vassort G 1990 The mechanism of positive inotropy induced by adenosine triphosphate in rat heart. Circ Res 67: 1007–1016.
Zipes DP, Mendez C 1973 Action of manganese ions and tetrodotoxin on atrioventricular nodal transmembrane potentials in isolated rabbit hearts. Circ Res 32: 447–454.
Hancox J, Levi AJ 1994 L-type calcium current in rod- and spindle-shaped myocytes isolated from rabbit atrioventricular node. Am J Physiol 267:H1670–H1680.
Geggel RL, Tucker L, Szer I 1988 Postnatal progression from second- to third-degree heart block in neonatal lupus syndrome. J Pediatr 113: 1049–1052.
Bacman S, Sterin-Borda L, Camusso JJ, Hubscher O, Arana R, Sterin-Borda E 1994 Circulating antibodies against neurotransmitter receptor activities in children with congenital heart block and their mothers. FASEB J 8: 1170–1176.
Herreman G, Galezewski N 1985 Maternal connective tissue disease and congenital heart block [Letter]. N Engl J Med 312: 1329
Lee LA, Coulter S, Erner S, Chu H 1987 Cardiac immunoglobulin deposition in congenital heart block associated with maternal anti-Ro antibody. Am J Med 83: 793–796.
Litsey SE, Noonan JA, O'Conner WN, Cottrill CM, Mitchell B 1985 Maternal connective tissue disease and congenital heart block. N Engl J Med 312: 98–100.
Ho YS, Esscher E, Anderson RH, Michaelsson M 1986 Anatomy of congenital complete heart block and relation to maternal anti-Ro antibodies. Am J Cardiol 58: 291–294.
Delbono O, Garcia J, Appel SH, Stefani E 1991 Calcium current and charge movement of mammalian muscle action of amyotrophic lateral sclerosis immunoglobulins. J Physiol 444: 723–742.
Acknowledgements
The authors thank the animal laboratory staff at the Veterans Administration Medical Center for their technical assistance.
Author information
Authors and Affiliations
Additional information
Supported by National Heart, Lung and Blood Institute Grant HL-55401(M.B.), Veterans Administration Medical Research Funds (M.B.), Grant AR-42455 from the National Institute of Arthritis, Musculoskeletal, and Skin Diseases(J.P.B.), and a grant-in-aid from the American Heart Association, New York Affiliate (J.P.B.).
Rights and permissions
About this article
Cite this article
Boutjdir, M., Chen, L., Zhang, ZH. et al. Serum and Immunoglobulin G from the Mother of a Child with Congenital Heart Block Induce Conduction Abnormalities and Inhibit L-Type Calcium Channels in a Rat Heart Model. Pediatr Res 44, 11–19 (1998). https://doi.org/10.1203/00006450-199807000-00002
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199807000-00002
This article is cited by
-
Autoimmune channelopathies as a novel mechanism in cardiac arrhythmias
Nature Reviews Cardiology (2017)
-
Neonatal congenital heart block
Indian Pediatrics (2013)
-
Congenital heart block: evidence for a pathogenic role of maternal autoantibodies
Arthritis Research & Therapy (2012)
-
Pregnancy Outcomes in Patients with Autoimmune Diseases and Anti-Ro/SSA Antibodies
Clinical Reviews in Allergy & Immunology (2011)
-
Congenital heart block in neonatal lupus: The pediatric cardiologist’s perspective
The Indian Journal of Pediatrics (2002)