Abstract
To evaluate the metabolic effects of long-term treatment with recombinant human (rh) GH in short children with chronic renal failure (CRF), annual oral glucose tolerance tests (oGTT) during rhGH therapy for up to 5 y in 53 prepubertal children with CRF on conservative treatment, dialysis, and after renal transplantation were compared with that of 12 age-matched children treated with rhGH for idiopathic short stature. At the start of rhGH treatment, fasting values of glucose, insulin, glycosylated Hb A(HbA1C), triglycerides, cholesterol, glucose, and insulin responses during oGTT were significantly elevated in all patient groups compared with control subjects (p < 0.001). In the total population, fasting and 2-h postprandial glucose concentrations were inversely correlated with GFR and positively with age and methylprednisolone dosage in transplanted patients. Fasting insulin levels were positively correlated with body mass index and inversely with GFR. RhGH treatment was not associated with a change in fasting or stimulated glucose concentrations in any treatment group throughout the observation period. In contrast, serum insulin levels increased during the first treatment year in all groups, resulting in a more marked elevation of integrated insulin levels in transplant (1402 ± 179 pM) and dialysis (1025 ± 114 pM) patients compared with conservatively treated patients (829 ± 94 pM), and control subjects (719 ± 89 pM) (p < 0.01). Hyperinsulinemia persisted in all treatment groups for up to 5 y of follow-up. In conclusion, age, renal function, and obesity are the major independent predictors of glucose tolerance in children with CRF. Long-term rhGH treatment does not affect glucose tolerance, but aggravates the preexisting hyperinsulinemia in children with end-stage renal disease. In concert with the dyslipidemia of uremia, the rhGH-promoted hyperinsulinemia may contribute to the long-term risk for premature atherosclerosis in patients with childhood onset CRF.
Similar content being viewed by others
Main
RhGH has been proven to be effective in promoting growth in short children with CRF before(1–6) and after renal transplantation(7–9). However, the high prevalence of insulin resistance(10–12) in patients with CRF, together with the potent antiinsulinergic effects of GH(13, 14) raise concerns that prolonged rhGH treatment may aggravate the alterations of carbohydrate and lipid metabolism typically encountered in uremic children. Moreover, concomitant glucocorticoid treatment after renal transplantation adds a further risk factor for glucose intolerance(15). Finally, insulin sensitivity in childhood is apparently influenced by age and obesity(11, 16, 17), factors that need to be accounted for in longitudinal analyses of glucose tolerance in uremic children treated with rhGH. In this study we present an analysis of the effects of age, obesity, and renal function on metabolic parameters in 53 prepubertal children with CRF and 12 short normal children followed for up to 5 y by oral glucose tolerance tests during rhGH treatment.
METHODS
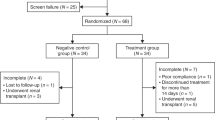
Patients. The data reported in the present analysis were collected by the German Study Group for GH treatment in CRF. The inclusion criteria of this multicenter study have been published previously(18). Briefly, patients were included with a height SD score (SDS) of ≤ -2.0 and/or a height velocity below the 25th percentile, a GFR <60 mL/min/1.73 m2 in children on conservative treatment, and a GFR >20 mL/min/1.73 m2 in patients after renal transplantation. Exclusion criteria were GH deficiency, hypothyroidism, diabetes mellitus, cystinosis, Addison's disease, malignancy, major cardiopulmonary disease, or severe general diseases. The study protocol was approved by the Ethics Committee of the University of Heidelberg. Written informed consent was obtained from the parents and patients.
The analysis presented here was restricted to 53 children who were prepubertal (defined as Tanner B/G stage I]) at the start of rhGH therapy and remained prepubertal throughout the observation period. Twenty-nine patients with preterminal CRF on conservative treatment, 14 patients with end-stage renal disease (seven on continuous peritoneal dialysis, seven on hemodialysis), and 10 patients with functioning renal allografts were investigated. Baseline clinical data are shown in Table 1. All transplanted children were on triple immunosuppressive therapy with cyclosporin A, azathioprine, and daily methylprednisolone (median dosage 5.1, range 3.6-9.1 mg/m2/d). Underlying renal diseases were renal dysplasia or hypoplasia (n = 20), obstructive and/or reflux uropathies(n = 14), glomerular diseases (n = 10), and hereditary nephropathies and various other renal diseases (n = 9).
Controls. Twelve healthy prepubertal children participating in a multicenter trial on growth hormone treatment for idiopathic short stature(study coordinator D. K. Schönberg) served as control subjects. All children were followed at the endocrine outpatient clinic of Heidelberg University Children's Hospital. The study protocol was approved by the Ethics Committee of the University of Heidelberg. Written informed consent was obtained from the parents and patients. Control subjects had normal fasting serum glucose and insulin levels, and no family history or evidence of diabetes mellitus or any other disease. All control children were below the third percentile for height, and had normal birth weight and length. GH deficiency had been excluded by serum GH levels equal to or above 10 ng/mL in nocturnal GH profiles and in a GH stimulation test with arginine. Their basic clinical data are shown in Table 1.
Treatment regimen. The CRF patients received rhGH at a weekly dose of 28-30 IU/m2 body surface area (Genotropin®, supplied by Pharmacia and Upjohn, Stockholm, Sweden) given in daily evening s.c. injections. Control subjects were treated with rhGH at a weekly dosage of 24 IU/m2 body surface area (Norditropin®, supplied by Novo Nordisc A/S, Denmark). The dose of rhGH was adjusted at 3-mo intervals during the study period as body size increased.
Physical assessments. To obtain age-independent estimates of body size and mass, height, height velocity, and BMI were converted to SD score values, related to age- and gender-specific means and SD of European reference populations(19, 20). To account for the growth retardation, height age rather than chronologic age was used in the calculation of BMI SDS to assign each individual to an age class in the reference population. Bone age was assessed using the Tanner-Whitehouse radioulnar score(21).
Laboratory studies. Biochemical examinations were performed in the local centers by standard procedures at least every 3 mo. HbA1c concentrations were measured centrally by the microcolumn technique according to Friedmann and Humbert(22). GFR was estimated by the calculated creatinine clearance, using the age-specific K values published by Schwartz et al.(23). Standard oGTTs (1.75 g of glucose/kg of body weight; maximum 75 g) after an overnight fast were performed before the start of treatment and at annual intervals during rhGH treatment. The time interval between the last rhGH injection and the oGTT was between 11 and 13 h. During the course of the test, serum glucose(glucose oxidase method by autoanalyzer) and insulin (solid phase RIA, Biermann, Bad Nauheim, Germany; intra- and interassay coefficients of variation were 3.7 and 8.5%, respectively) concentrations were measured at 0, 30, 60, 90, and 120 min. The areas under the glucose and insulin concentration curves during oGTT were calculated according to the method of Haffner et al.(24). Impaired glucose tolerance was defined according to the pediatric standards proposed by the National Diabetes Group of the National Institutes of Health: fasting venous serum glucose concentration <7.8, but 2-h glucose level >7.8 mmol/L (140 mg/dL)(25). This report emphasizes fasting insulin as a measure of insulin resistance and the ratio of the 30-min change in insulin to the 30-min change in glucose (ΔI30/ΔG30) during the oGTT as a measure of pancreatic secretory capacity(26).
Statistical analysis. Statistical analyses were performed using PC-SAS, version 6.11 (SAS Institute Inc., Cary, NC). Results are expressed as means ± SEM. Comparisons between groups were performed by ANOVA, followed by Duncan's multiple range test. Longitudinal within-group differences were assessed by one-way ANOVA for repeated measurements. Those parameters that were not normally distributed, as defined by the Shapiro-Wilks test, were logarithmically transformed before analysis. Associations between variables were evaluated by univariate and multivariate regression analysis. Univariate linear regression analysis was performed to identify possible factors influencing oGTT results, i.e. age at study, sex, GFR (in dialysis patients a GFR of 5 mL/min/1.73 m2 was assumed), height SDS, height velocity SDS, BMI SDS, and methylprednisolone dosage in transplanted patients. Thereafter, multiple regression analysis with stepwise inclusion of the variables identified in the univariate regression was performed. Statistical significance was accepted for p < 0.05.
RESULTS
Baseline results before rhGH treatment. Before rhGH treatment, fasting levels of HbA1C and glucose as well as the glucose responses during oGTT (Fig. 1A) were significantly (p < 0.01) elevated in all patient groups compared with controls(Table 2). There was no significant difference with respect to baseline oGTT data between children on hemo- and peritoneal dialysis. Three out of 29 patients on conservative treatment, and three out of 14 children on dialysis, but none of the 13 transplanted patients showed impaired oral glucose tolerance. Fasting and integrated glucose concentrations were significantly (p < 0.05) higher in dialyzed patients compared with patients on conservative treatment or after renal transplantation (Table 2). GFR (inverse correlation,Fig. 2A) and age (positive correlation,Fig. 3A) were identified as independent predictors of fasting and stimulated glucose concentration by multiple regression analysis(Table 3). In transplanted patients, fasting (r= 0.48, p < 0.05) and 2-h postprandial glucose response during oGTT (Fig. 3B) were positively correlated with the daily methylprednisolone dosage.
(A) Glucose responses during oGTT at baseline(left) and after 1 y of rhGH treatment (right) in CRF patients compared with controls. Data are the mean ± SEM; CT, conservative treatment; annotations indicate significant (p < 0.05) difference of CT (+), dialysis (#), or transplant ($) group from controls (ANOVA). (B) Insulin responses during oGTT at baseline(left) and after 1 y of rhGH treatment (right) in CRF patients compared with controls. Data are the mean ± SEM; CT, conservative treatment; annotations indicate significant (p < 0.05) difference of CT (+), dialysis (#) or transplant ($) group from controls(ANOVA).
(A) Correlation between fasting serum glucose concentration and GFR in children with CRF on conservative treatment (○) and after renal transplantation (•) before rhGH treatment. (○),r = -0.50, p < 0.01; (•), r = -0.81,p < 0.01. (B) Correlation between fasting serum insulin concentration and GFR in children with CRF on conservative treatment (○) and after renal transplantation (•) before rhGH treatment. (○),r = -0.32, p = 0.12; (•) r = -0.79,p < 0.01.
(A) Relationship between age at study and 2-h glucose response during oGTT before start of rhGH treatment in all subjects combined (r = 0.51, p < 0.0001). Symbols denote patients on conservative treatment (○), dialysis (▵), after renal transplantation (•), and controls (▪). (B) Relationship between methylprednisolone dosage and 2-h glucose response to oGTT before start of rhGH treatment in transplanted patients (r = 0.65,p < 0.05).
Fasting serum insulin concentrations were significantly (p < 0.01) elevated in all patient groups compared with controls, being highest in the transplant group (Table 2). Serum insulin levels during oGTT were significantly (p < 0.01) elevated in the transplant group, and tended to be elevated in patients on conservative treatment and dialysis (Fig. 1B). Fasting insulin concentrations were negatively correlated with GFR (Fig. 2B) and positively correlated with BMI SDS (Table 3). Similarly, the 2-h insulin response during oGTT was positively correlated with BMI SDS. No association was found between fasting or stimulated insulin concentrations and methylprednisolone dosage in the transplant group. Baseline cholesterol and triglycerides serum levels were significantly (p< 0.01) elevated compared with controls in all patient groups[cholesterol/triglycerides (mmol/L): conservative treatment, 6.0 ± 0.3/1.8 ± 0.1; dialysis, 6.7 ± 0.6/2.3 ± 0.3; transplant, 7.0 ± 0.4/2.2 ± 0.5; controls, 4.6 ± 0.2/1.0 ± 0.2].
Effect of rhGH treatment. Whereas fasting and oGTT response of glucose did not change throughout the observation period in any group, fasting and stimulated insulin levels were 2-fold increased compared with baseline after the first year of rhGH therapy in the dialysis and transplant patients, as well as in controls, and remained elevated at a constant level throughout the further follow-up (Table 2, Fig. 1B). In patients on conservative treatment, a less marked rise in insulin levels during oGTT was noted, which became significant only after the second treatment year(Table 2). Fasting and stimulated insulin was significantly higher (p < 0.01) in the dialysis and transplant groups compared with controls after the first and second treatment year. Those five patients on conservative treatment who completed 5 y of follow-up had a mean integrated insulin concentration of 536 ± 68 pmol/L at baseline, increased to a maximum of 774 ± 81 pmol/L after 2 y of treatment, and remained consistently elevated until the 5-y oGTT (749 ± 94 pmol/L). In the dialysis and transplant group the ΔI30/ΔG30 ratio was significantly increased compared with baseline from the first treatment year onward.
In five out of six children who had impaired oral glucose tolerance before the start of rhGH therapy, serum glucose levels during oGTT returned to the normal range after 1-3 y of rhGH treatment. In the other patient impaired glucose tolerance did not worsen during 3 treatment years. Four patients (two on conservative treatment, one on dialysis, one transplanted) developed a transient impairment of oral glucose tolerance. None of the patients developed overt diabetes mellitus. No significant change occurred with respect to HbA1c (Table 2), cholesterol or triglycerides (not given) serum levels during rhGH treatment in any treatment group. Multiple regression analysis of glucose and insulin responses during oGTT revealed similar results after 1 y of rhGH treatment as observed at baseline.
DISCUSSION
This report compares the severity of insulin insensitivity in patients with different treatment modalities for CRF and short normal children both before the start of treatment and during long-term rhGH treatment. At baseline, fasting and glucose-stimulated insulin secretion and serum lipid levels were increased to a similar degree in CRF patients on conservative treatment, dialysis, and after renal transplantation compared with control subjects. Multiple regression analysis identified age, GFR, degree of obesity, and glucocorticoid dosage as independent predictors of insulin sensitivity. Long-term rhGH treatment provoked a sustained increase in fasting and stimulated serum insulin levels in all children, which was most marked in patients on dialysis and after renal transplantation.
In view of the well known insulin insensitivity in uremic patients, but also in patients after renal transplantation, careful surveillance is essential when such children are treated over prolonged periods of time with rhGH, a hormone with known hyperglycemic properties. The studies published so far on safety aspects of rhGH treatment in children with CRF(1–9, 18, 27–29) were compromised by lack of oGTT data or small patient numbers, lack of control groups, short observation periods, and a disregard of the confounding effects of puberty, which started in many patients during the period of observation. Puberty is physiologically associated with a reduced insulin sensitivity, both in normal subjects and in patients with CRF(11, 16). Therefore, we used the data of a multicenter trial on rhGH treatment in CRF and after renal transplantation to specifically analyze the long-term evolution of glucose tolerance in patients who remained prepubertal throughout the observation period.
The baseline examinations before rhGH treatment revealed a high degree of insulin insensitivity in the CRF patients. The area under the curves of glucose and insulin during the oGTT as well as HbA1c levels were elevated to a similar degree in patients on conservative treatment, dialysis, and after renal transplantation. It should be emphasized that, despite the comparable degree of insulin resistance in the three patient groups, different pathomechanisms are responsible for this disorder in uremic and transplant patients. In uremia, insulin-stimulated glucose disposal is suppressed, and the insulin-mediated suppression of hepatic gluconeogenesis is insufficient(12, 30). Certain endocrine alterations(1,25-vitamin D deficiency, hyperparathyroidism, hyperglucagonemia), metabolic acidosis, and effects of as yet undefined substances accumulating in uremia may underlie this disorder(31). After successful renal transplantation, impaired insulin sensitivity is mainly a consequence of glucocorticoid treatment(15). Thus, regardless of its etiology, insulin insensitivity appears to be an inevitable complication of CRF, which may not be corrected by renal transplantation. In view of the increasingly recognized pathogenetic role of hyperinsulinemia in the development of atherosclerosis(32, 33), the persistence of this condition is particularly relevant for children. Clinical and in vitro studies have recently provided evidence that insulin per se contributes to a state of hypercoagulability by stimulating thrombin activity and synthesis of endogenous inhibitors of the thrombolytic system(32, 34–36). A further suspected risk factor for premature atherosclerosis in patients with childhood onset CRF is the uremia associated dyslipidemia. In this study, hypercholesterinemia and hypertriglyceridemia were not aggravated by rhGH treatment. However, we recently observed a rise in lipoprotein(a) serum levels, a powerful risk factor for cardiovascular morbidity(37), during rhGH treatment in children with CRF(38).
In keeping with previous results using glucose clamp techniques(11), we observed an inverse relationship between insulin resistance and GFR. Interestingly, we also found an inverse correlation between postprandial glucose concentration and age. Although a decreased insulin sensitivity has been demonstrated in normal and uremic pubertal compared with prepubertal subjects(11, 16), this is the first time that an age effect even in the prepubertal period is demonstrated in CRF patients. This finding, which confirms one previous report in normal and obese prepubertal children(17), suggests caution when interpreting oGTT results in children differing in age. Another factor influencing glucose tolerance across the treatment groups was the degree of obesity as expressed by BMI SDS. The role of glucocorticoid-induced obesity in the renal transplant patients is evident from the observed interrelationship of the daily glucocorticoid dosage, relative obesity, and the parameters of glucose tolerance.
The antiinsulinergic effects of GH are characterized by an interference with glycolysis and stimulation of gluconeogenesis at the postreceptor level(13, 14), resulting in impaired glucose tolerance in 30-60% and overt diabetes mellitus in 20% of patients with GH-producing tumors(39, 40). On the other hand, in vitro studies showed that GH has a direct stimulatory effect on pancreatic insulin synthesis and secretion(41, 42), which in the long run may lead to an exhaustion of the pancreatic β cells. Whereas we did not observe a change in glucose tolerance throughout the course of rhGH treatment over 5 y in any treatment group, a marked rise of fasting and stimulated serum insulin concentrations occurred during the first year of treatment in all children, without further changes during the subsequent treatment years. This rise was most pronounced in the transplant group.
Our short- and long-term results on carbohydrate metabolism are in line with some(2, 4, 8, 9, 18), but at variance with other reports(28, 29) in CRF patients. Only one study, limited by small patient numbers and using a lower rhGH dosage, failed to show the increase in insulin secretion during the first treatment year(28). The less marked increase in insulin levels during rhGH treatment in CRF patients reported by the North American multicenter trial in comparison with our study might be explained by the only mild impairment of renal function compared with our study population and/or by differences in age(29).
In the absence of glucose clamp studies, the observed selective increase in insulin secretion, which is not accompanied by an aggravation of oral glucose intolerance, is difficult to interpret. In principle, two explanations are possible: rhGH treatment may disturb glucose disposal, but development of overt glucose intolerance is prevented by a compensatory increase in insulin secretion. Alternatively, there may be no change in insulin sensitivity, and the observed increase in insulin secretion may be a specific effect of long-term rhGH treatment on the pancreatic secretory capacity. The finding of an increased ΔI30/ΔG30 ratio is in favor of the latter hypothesis. This effect was particularly pronounced in the transplanted patients. In addition, euglycemic clamp studies in short normal subjects after 1 y of therapy with a relatively high rhGH dose (i.e. 8 IU/m2/d) did not show an impairment of insulin-stimulated glucose disposal compared with baseline(43).
In conclusion, we observed a selective increase in fasting and glucose-stimulated insulin secretion without a change in glucose tolerance in patients with CRF, after renal transplantation but also in short normal children in response to rhGH therapy. This phenomenon was exaggerated in patients on dialysis and after renal transplantation and persisted for up to 5 y of rhGH treatment. Although the absence of increased glucose intolerance during long-term rhGH treatment is reassuring with respect to the diabetogenic potential of rhGH, the persisting hyperinsulinemia, combined with the dyslipidemia associated with CRF, raises concern that rhGH therapy may contribute to the long-term risk for premature atherosclerosis in patients with childhood-onset CRF.
Abbreviations
- BMI:
-
body mass index
- CRF:
-
chronic renal failure
- oGTT:
-
oral glucose tolerance test
- ΔI30/ΔG30:
-
change in insulin/glucose ratio over the first 30 min of oGTT
- SDS:
-
SD score
- rhGH:
-
recombinant human GH
References
Koch VH, Lippe BM, Nelson PA, Boechat MI, Sherman BM, Fine RN 1989 Accelerated growth after recombinant human growth hormone treatment of children with chronic renal failure. J Pediatr 115: 365–371.
Tönshoff B, Mehls O, Heinrich U, Blum WF, Ranke MB, Schauer A 1990 Growth-stimulating effects of recombinant human growth hormone in children with end-stage renal disease. J Pediatr 116: 561–566.
Rees L, Rigden SPA, Ward G, Preece MA 1990 Treatment of short stature in renal disease with recombinant human growth hormone. Arch Dis Child 65: 856–860.
Fine RN, Kohaut EC, Brown D, Perlman AJ, For The Genentech Cooperative Study Group 1994 Growth after recombinant human growth hormone treatment in children with chronic renal failure: report of a multicenter randomized double blind placebo-controlled study. J Pediatr 124: 374–382.
Haffner D, Wühl E, Tönshoff B, Mehls O, for the German Study Group for Growth Hormone Treatment in Chronic Renal Failure 1994 Growth hormone (GH) treatment in short children with chronic renal failure(CRF): 5-year experience. Nephrol Dial Transplant 9: 960–961.
Fine RN, Kohaut E, Brown D, Kuntze J, Attie KM 1996 Long-term treatment of growth retarded children with chronic renal insufficiency, with recombinant human growth hormone. Kidney Int 49: 781–785.
Van Es A 1991 Growth hormone treatment in short children with chronic renal failure and after renal transplantation: combined data from European clinical trials. Acta Paediatr Scand Suppl 379: 42–48.
Tönshoff B, Haffner D, Mehls O, Dietz M, Ruder H, Blum W F, Heinrich U, Stoever B, Members of the German Study Group for GH Treatment in Children with Renal Allografts 1993 Efficacy and safety of growth hormone treatment in short children with renal allografts: three year experience. Kidney Int 44: 199–207.
Hokken-Koelega ACS, Stijnen T, De J, Donckerwolke RA, Groothoff JW, Wolff ED, Blum WF, de Muinck Keizer-Schrama SMPF, Drop SLS 1996 A placebo controlled double blind trial of growth hormone treatment in prepubertal children after renal transplant. Kidney Int 49 ( suppl 53): 128–134.
Schaefer F, Mehls O 1994 Endocrine, metabolic and growth disorders. In: Holliday MA, Barrat TM, Avner ED (eds) Pediatric Nephrology. Williams & Wilkins, Baltimore, pp 1241–1286.
Mak RHK, Haycock GB, Chantler C 1983 Glucose intolerance in children with chronic renal failure. Kidney Int 24 ( suppl 15): 22–26.
Smith D, DeFronzo RA 1982 Insulin resistance in uremia is mediated by postbinding defects. Kidney Int 22: 54–62.
Rosenfeld RG, Wilson DM, Dollar LA, Bennet A, Hintz RL 1982 Both human pituitary growth hormone and recombinant DNA derived human growth hormone cause insulin-resistance at a postreceptor level. J Clin Endocrinol Metab 55: 973–981.
Bratusch-Marrain RR, Smith D, DeFronzo RA 1982 The effect of growth hormone on glucose metabolism and insulin secretion in man. J Clin Endocrinol Metab 54: 1033–1038.
Fennel RS, Van Deusen J, Riley WL 1983 Steroid-induced diabetes in pediatric renal transplant recipients. In J Pediatr Nephrol 4: 103–107.
Amiel SA, Sherwin RS, Simonson DC, Lauritano AA, Tamborlane WV 1986 Impaired insulin action in puberty. N Engl J Med 315: 215–219.
Deschamps I, Giron BJ, Lestradet H 1977 Blood glucose, insulin, and free fatty acid levels during oral glucose tolerance tests in 158 obese children. Diabetes 26: 89–93.
Tönshoff B, Dietz M, Haffner D, Tönshoff C, Stöver B, Mehls O, and Members of the German Study Group for Growth Hormone Treatment in Chronic Renal Failure 1991 Effects of 2 years of growth hormone treatment in short children with renal disease. Acta Paediatr Scand Suppl 379: 33–41.
Prader A, Largo RH, Molinari L, Issler C 1988 Physical growth of Swiss children from birth to 20 years of age. Helv Paediatr Acta Suppl 52: 1–125.
Rolland-Cachera MF, Cole TJ, Sempe M, Tichet J, Rossignol C, Charraud A 1991 Body mass index variations: centiles from birth to 87 years. Eur J Clin Nutr 45: 13–21.
Tanner JM, Whitehouse RH, Cameron N, Marshall WA, Healy MJR, Goldstein H 1983 Assessment of Skeletal Maturity and Prediction of Adult Height (TW2 Method), 2nd Ed. Academic Press, New York, pp 50–103.
Friedman S, Humbert JR 1979 A simple microchromatographic column for determination of hemoglobin A1a+b and A1c . Hemoglobin 3: 411–428.
Schwartz GJ, Haycock GB, Edelman CM 1976 A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58: 259–263.
Haffner SM, Stern MP, Hazuda HP, Pugh JA, Patterson JK 1986 Hyperinsulinemia in a population at high risk for non-insulin dependent diabetes mellitus. N Engl J Med 315: 220–224.
National Diabetes Data Group 1979 Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 28: 1039–1057.
Haffner SM, Miettinen H, Gaskill SP, Stern MP 1995 Decreased insulin secretion and increased insulin resistance are independently related to the 7-year risk of NIDDM in Mexican-Americans. Diabetes 44: 1386–1391.
Tönshoff B, Tönshoff C, Mehls O, Pinkowski J, Blum WF, Heinrich U, Stöver B, Gretz N 1992 Growth hormone treatment over one year in children with preterminal chronic renal failure: no adverse effect on glomerular filtration rate. Eur J Pediatr 151: 601–607.
Van Dop C, Donohoue PA, Jabs KL, Bock GH, Fivush BA, Harmon WE 1991 Glucose tolerance in children with renal allografts and effect of growth hormone treatment. J Pediatr 118: 708–714.
Saenger P, Attie KM, DiMartino-Nardi J, Fine RN, The Genentech Collaborative Group 1996 Carbohydrate metabolism in children receiving growth hormone for five years. Pediatr Nephrol 10: 261–263.
Schmitz O 1985 Insulin mediated glucose uptake in non-dialyzed and dialyzed uremic insulin-dependent diabetic subjects. Diabetes 34: 1152–1159.
Schmitz O 1991 Glucose metabolism in non-diabetic and insulin-dependent diabetic subjects with end-stage renal failure. Dan Med Bull 38: 36–52.
Sobel BE 1996 Potentiation of vasculopathy by insulin. Implications from an NHLBI clinical alert. Circulation 93: 1613–1615.
Perry IJ, Wannamethee SG, Whincup PH, Shaper AG, Walker MK, Alberti KG 1996 Serum insulin and incident coronary heart disease in middle-aged British men. Am J Epideminol 144: 224–234.
Marongiu F, Conti M, Mameli G, Sorano GG, Cossu E, Cirillo R, Balestrieri A 1990 Is the imbalance between thrombin and plasmin activity in diabetes related to the behavior of antiplasmin activity?. Thromb Res 58: 91–99.
McGill JB, Schneider DJ, Arfken CL, Lucore CL, Sobel BE 1994 Factors responsible for impaired fibrinolysis in obese patients and NIDDM patients. Diabetes 43: 104–109.
Nordt TK, Sawa H, Fujiii S, Sobel BE 1995 Induction of plasminogen activator inhibitor type-1 (PAI-1) by proinsulin and insulinin vivo. Circulation 91: 764–770.
Cressman MD, Heyka RJ, Paganini EP, O'Neil J, Sibinski CI, Hoff HF 1992 Lipoprotein(a) is an independent risk factor for cardiovascular disease in hemodialysis patients. Circulation 86: 475–482.
Querfeld U, Haffner D, Wühl E, Wingen AM, Wolter K, Friedrich B, Michalk DV, Mehls O 1996 Treatment with growth hormone increases lipoprotein(a) serum levels in children with chronic renal insufficiency. Eur J Pediatr 155: 913–918.
Sonksen PH, Greenwood FC, Ellis JP, Lowy C, Rutherford A, Nabarro JDN 1967 Changes of carbohydrate tolerance in acromegaly with progress of the disease and in response to treatment. J Clin Endocrinol Metab 27: 1418–1423.
Rizza RA, Mandarino JL, Gerich JE 1982 Effects of growth hormone on insulin action in man. Mechanisms of insulin resistance, impaired suppression of glucose production, and impaired stimulation of glucose utilization. Diabetes 31: 663–669.
Formby B, Ullrich A, Coussens L, Walker L, Petersen CM 1982 Growth hormone stimulates insulin gene expression in cultured human fetal pancreatic islet. J Clin Endocrinol Metab 66: 1075–1080.
Rabinovitch A, Quigley C, Rechler MM 1983 Growth hormone stimulates islet B-cell replication in neonatal rat pancreatic monolayer cultures. Diabetes 32: 307–312.
Walker J, Chaussain JL, Bougneres PF 1989 Growth hormone treatment of children with short stature increases insulin secretion but does not impair glucose disposal. J Clin Endocrinol Metab 69: 253–258.
Acknowledgements
RhGH was kindly provided by Pharmacia and Upjohn, Stockholm, Sweden (CRF patients) and Novo Nordisc A/S, Denmark(control subjects). We are indebted to Dr. Gudrun Cimander, Pharmacia and Upjohn, Erlangen, Germany, for valuable assistance in coordinating the study.
Author information
Authors and Affiliations
Consortia
Rights and permissions
About this article
Cite this article
Haffner, D., Nissel, R., Wühl, E. et al. Metabolic Effects of Long-Term Growth Hormone Treatment in Prepubertal Children with Chronic Renal Failure and after Kidney Transplantation. Pediatr Res 43, 209–215 (1998). https://doi.org/10.1203/00006450-199802000-00009
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199802000-00009
This article is cited by
-
Clinical practice recommendations for growth hormone treatment in children with chronic kidney disease
Nature Reviews Nephrology (2019)
-
Growth hormone therapy in children with CKD after more than two decades of practice
Pediatric Nephrology (2016)
-
New-onset diabetes after kidney transplant in children
Pediatric Nephrology (2015)