Abstract
Periventricular white matter injury is the leading cause of cerebral palsy in premature infants for which no effective treatments are available. Our previous studies have demonstrated that pharmacological activation of the cAMP response element-binding protein (CREB) signaling pathway, before hypoxic-ischemia protected against neuronal injury in neonatal rats. We examined whether rolipram, a phosphodiesterase type IV inhibitor, treatment after hypoxic-ischemia is protective against white matter injury in neonatal rats. Rats were exposed to hypoxia-ischemia (HI) on P7 and then treated with daily injections of various doses of rolipram (P7–P11). Immunohistochemical staining for myelin basic protein, ED1, glial fibrillary acidic protein, CREB and O1 were examined on P11. We found that the periventricular white matter and deep cortical lesions were exacerbated by rolipram administration after HI injury. The lesions in the rolipram-treated group also showed increased astrogliosis and increased CREB phosphorylation in the activated microglia and astrocytes. Furthermore, the rolipram-posttreated HI group had markedly depleted preoligodendrocytes in the ipsilateral hemisphere, which may be related to decreased preoligodendrocytes proliferation after rolipram treatment per se. These data suggest that rolipram treatment after hypoxic-ischemia is not protective; in contrast, rolipram may exacerbate hypoxic-ischemic white matter injury in neonatal rat brains.
Similar content being viewed by others
Main
Nearly 90% of low-birth weight infants now survive with the advances in neonatal intensive care. Of the survivors, however, 10–15% have cerebral palsy, and 25–50% have manifest cognitive and behavioral deficits (1). Periventricular white matter injury, or leukomalacia (PVL), is the major form of brain injury in preterm babies. The neuropatholgical findings are characterized by distinct cystic white matter lesions and, commonly, a more diffuse loss of white matter volume and secondary ventriculomegaly (2). Notably, despite the significant long-term morbidity, there is currently no specific treatment for these disorders.
Although, the exact cause of PVL in human infants is currently unknown, hypoxia-ischemia (HI) is believed to be a significant cause (3). Cell-type specific factors are also likely to underlie the mechanisms of PVL. Data from a recent study demonstrated that PVL in humans was related to oxidative damage that particularly targeted cells of the oligodendrocyte lineage; whereas neuronal and glial cells were markedly more resistant (4). The timing of appearance of preoligodendrocytes (preOLs) coincides with the high-risk period for PVL (5). Considerable data demonstrate that preOLs are highly susceptible to oxidative stress and hypoxic-ischemia injury (6–9). Compared with mature oligodendrocytes, preOLs express lower levels of antioxidant enzymes (6). These data suggest that acceleration of preOLs maturation might be a feasible strategy to reduce the severity of PVL.
cAMP plays an important role in inducing oligodendrocyte differentiation and myelin synthesis (10,11). Furthermore, the transcription factor, cAMP response element-binding protein (CREB) is a key mediator of stimulus-induced cAMP-mediated nuclear responses that underlie survival of neurons. CREB is phosphorylated on Ser133 (pCREB) and consequently binds to the cAMP response element of target genes. Recent data have revealed that virus-mediated expression of a constitutive active form of CREB can protect preOLs from excitotoxicity (12). Rolipram has been shown to elevate cAMP levels by inhibiting c-AMP specific phosphodiesterases type IV (13). Our previous studies demonstrated that pharmacological activation of the cAMP-CREB signaling pathway before hypoxic-ischemia with rolipram protected against neuronal injury in neonatal rats (14,15). It has also been shown that rolipram treatment after spinal cord injury promotes axonal regeneration, attenuates glial scar formation, and enhances remyelination and functional recovery in adult rats (16,17). Therefore, in this study, we investigated whether pharmacological activation of the cAMP-CREB signaling pathway with rolipram after hypoxic-ischemia is protective against white matter injury in neonatal rats.
MATERIALS AND METHODS
All procedures were approved by and in accordance with the guidelines of the Animal Care Review Committee at the Chang Gung Memorial Hospital. Ten to 12 pups per dam were housed with a 12/12-h light/dark schedule. We used postpartum day 7 (P7) male Sprague-Dawley rat pups when the cerebral white matter at that stage is primarily populated by preOLs, which increased the vulnerability of white matter to hypoxic-ischemia brain injury (18).
Hypoxic-ischemia.
The animals were anesthetized with 2.5% halothane (balance, room air), and the right common carotid artery was surgically exposed and permanently ligated with 5–0 surgical silk. After surgery, the pups were returned to the dam for a 1-h recovery period before inducing hypoxia. During hypoxia, the rat pups were placed in airtight 500-mL containers partially submerged in a 37°C water bath through which humidified 6.5% oxygen (balance, nitrogen) was maintained at a flow rate of 3 L/min for 1 h. After completion of hypoxia, the rat pups were returned to their cages. For treatment trials, rat pups received daily intraperitoneal injection of rolipram (Sigma Chemical Co., St. Louis, MO) 0.5 mg/kg (Rol-0.5 group; n = 14), 1 mg/kg (Rol-1 group; n = 15) or 3 mg/kg (Rol-3 group; n = 12), or vehicle (Veh group; n = 15) from P7 to P11, commencing immediately after completion of hypoxia. There was no significant difference in mortality (an average of 15%) or body weight gain between the vehicle-, Rol-0.5, Rol-1 and Rol-3-treated groups.
Histologic preparation.
On P11, the rats were killed by injecting an overdose of sodium pentobarbitone. The brains were then perfused with saline followed by 4% paraformaldehyde. The brains were removed and immersed in the same fixative for 48 h. The brains were then dehydrated through a graded series of alcohols and finally embedded in paraffin. The coronal paraffin sections, 10 μm thick, were stained with hematoxylin and eosin.
Immunohistostaining.
Paraffin sections were dewaxed, hydrated through graded alcohols and placed in phosphate-buffered saline (PBS). Endogenous peroxidase was blocked for 30 min in 0.3% H2O2 in methanol. Antigen unmasking was performed by incubating the sections in sodium citrate at 95°C for 10 min. Nonspecific binding was blocked by incubating the sections in PBS buffer 5% goat serum for 1 h at room temperature. The sections were then incubated with various primary antibodies followed by a 60-min incubation at room temperature with secondary Ab (Santa Cruz Biotechnology, Santa Cruz, CA). The primary antibodies used were myelin basic protein 1: 500 (MBP, Chemicon, Temecular, CA); glial fibrillary acidic protein 1:200 (GFAP, DAKO, Glostrup, Denmark); ED1 1: 500 (Serotec, Raleigh, NC); and pCREB 1:1000 (Upstate Biotechnology, Lake Placid, VA). The sections were developed in 3′3-diaminobenzidine (Sigma Chemical Co.) with the Vectastatin ABC system (Vector Laboratories, Burlingame, CA). In every experiment, a control with the primary antibody omitted was used as a negative control.
Double-fluorescence immunocytochemistry.
After blocking for 1 h, the slides were incubated overnight at 4°C with a mixture of two of the following primary antibodies: GFAP (1:200), ED1 (1: 500), NeuN (1:200; Chemicon), and pCREB (1:200). The slides were washed three times with PBS and then incubated with Texas Red-conjugated anti-rabbit and fluorescein isothiocyanate-conjugated anti-mouse Ab (1:200; Jackson ImmunoResearch) for 1 h at room temperature. The fluorescence signals were detected using a Nikon E400 microscope at excitation-emission wavelengths of 596–615 nm (Texas Red) and 470–505 nm (fluorescein isothiocyanate).
Analysis of preOL proliferation.
Rats were treated with daily rolipram (3 mg/kg, n = 9) or vehicle (n = 9) on P7–P11 as stated above, except that hypoxic-ischemic insult was not induced. Animals received concurrent injections of daily BrdU (100 mg/kg, Sigma Chemical Co.) during the treatment protocol on P10 and P11 and killed on P11. Coronal sections were labeled with O4 Ab (chemicon), fixed, and processed for BrdU labeling (14). BrdU (+)-O4(+) cells were counted in the corpus callosum and external capsule of sections stereotactically similar to the region evaluated for injury.
Analysis.
Using IMAGE PRO software (Image Pro, Boston), under a microscope (Nikon, Japan), the areas of parietal cortex (area between the rhinal sulcus, the cingulum, and the external boundaries of the corpus callosum), hippocampus, thalamus, striatum, as well as the area of positive MBP immunostaining between rhinal sulcus and cingulum were measured. Additionally, the ratio of each area (ipsilateral to contralateral hemisphere) was calculated. The degree of neuronal damage was scored by hematoxylin and eosin staining: mild (few damaged neurons), moderate (moderate numbers of damaged neurons), and severe (extensive number of damaged neurons) (19). The degree of neuronal damage was assessed on three separate sections at the level of the striatum, the dorsal hippocampus, and the ventral hippocampus.
Statistics.
Statistical significance (p < 0.05) was determined using one-way analysis of variance (SPSS Inc., Chicago, IL). Post hoc comparisons were made using the Mann-Whitney U test. Continuous data were expressed as mean ± standard error of the mean unless indicated otherwise.
RESULTS
Selective vulnerability of immature white matter to moderate hypoxic ischemia in rat pups.
Four days after moderate hypoxic-ischemia in P7 rat pups, there was subtle atrophy in the cortex and striatum of the cerebral hemisphere ipsilateral to carotid artery ligation, although overall tissue integrity was preserved. Seventy-five percent of the rat pups had small histopatholgical changes manifesting as a conical loss of cells in the deep cortical layers of the ipsilateral parietal cortex. No overt pathologic changes in the thalamus, dorsal hippocampus, or striatum were observed in bilateral hemisphere. There was a nonsignificant trend of decreased right-to-left (R/L) ratios in the parietal cortex, striatum and thalamus in the hypoxic-ischemia group compared with the naïve control. No differences in the dorsal hippocampus areas were found between the hypoxic-ischemia and control groups (data not shown).
There was substantially decreased MBP immunoreactivity in the ipsilateral periventricular white matter and external capsule in 80% of the rat pups with hypoxic-ischemia. Decreased MBP immunostaining in the ipsilateral internal capsule and striatum was also observed in 75% of these rat pups. Compared with the naïve group, a significant reduction in R/L ratio of MBP-positive areas was observed in the hypoxic-ischemia group (data not shown).
Postinsult treatment of rolipram exacerbates deep cortical and white matter injury in immature rats.
Although, the overall tissue integrity was preserved (Fig. 1A and B), postischemia treatment with rolipram increased neuronal cell death in the deep cortex of the ipsilateral hemisphere (Fig. 1C and D). There were no significant differences in the R/L ratio of cortical areas between the naïve and the rats posttreated with rolipram or vehicle (Fig. 1G). Further scoring revealed that the vehicle-treated group had mild cortical neuronal damage, but most of the rolipram-treated groups had moderate to severe neuronal damage (Fig. 1H, p < 0.05).
Postinsult treatment of rolipram exacerbates deep cortical and white matter injury in immature rats. After hypoxia-ischemia (HI), rat pups were treated with rolipram 0.5 mg/kg (Rol-0.5 group), 1 mg/kg (Rol-1) or 3 mg/kg (Rol-3), or vehicle (Veh). Compared with the vehicle-treated HI rats (A), the overall tissue integrity is preserved but the ventricle is dilated in rolipram-treated HI groups (B). HE stain reveals that the eosinophilic cells in columns extend from the deep cortical layers into the middle layers in the ipsilateral cortex of the rolipram-treated HI group rats (C). In the most severely damaged cortex of rolipram-treated HI rats, the lesions extend sidewise, leading to confluence of necrosis in the deeper layers rather than extending into the external layers (D). Myelin-basic protein (MBP) immunostaining is less intense in rats treated with rolipram (F) than in rats treated with vehicle (E). There were no significant differences in the R/L ratio of cortical areas between the naïve and the rats posttreated with rolipram or vehicle (G). The cortical neuronal damage was scored as mild (white column), moderate (gray column) and severe (black column). There was a significant difference in the distribution of cortical lesion severity between the vehicle-and rolipram-treated HI groups. The rolipram-treated HI groups had a higher rate of moderate to severe cortical lesions than the vehicle-treated HI group (*p < 0.05, compared with vehicle-treated group, one-way ANOVA, n = 9/group). There was no dose-related effect on the severity of cortical lesions among the rolipram-treated HI groups (H). The right-to-left (R/L) ratio of MBP immunoreactivity revealed that there were significant differences between the vehicle- and rolipram-treated HI groups (*p < 0.05, one-way ANOVA test, n = 9/group). There was no significant difference in the MBP immunoreactivity ratio between the Rol-0.5, Rol-1 and Rol-3 groups (I). The degree of ventriculomegaly was significantly higher in the rolipram-treated HI groups than in the vehicle-treated HI group (**p < 0.001, nonparametric Mann-Whitney U test after one way ANOVA, n = 9/group). Furthermore, the degree of ventriculomegaly was significantly higher in the Rol-3 group than in the naïve, vehicle, Rol-0.5, and Rol-1groups (J) (p < 0.05). Scale bar: 500 μm in A and B, 50 μm in C and D, 500 μm in insets, 100 μm in E and F.
We observed significant decreases in MBP immunostaining in the ipsilateral periventricular, external capsule and striatum areas after hypoxic ischemia injury in the rolipram-treated groups compared with those areas in the vehicle-treated group (Fig. 1E and F). There was a significant difference in right-to-left ratio of MBP immunoreactivity between the vehicle-treated and rolipram-treated groups (Fig. 1I, p < 0.05). Rolipram-treated rats also had significantly a higher degree of ventriculomegaly in the ipsilateral cerebral hemisphere than the vehicle-treated rats (Fig. 1J, p < 0.001). Furthermore, there was a significant difference in ventriculomegaly between the rolipram-treated groups. The degree of ventriculomegaly was significantly higher in the Rol-3 group than in the Rol-1 and Rol-0.5 groups (p < 0.05).
Postinsult treatment with rolipram exacerbated reactive astrogliosis.
The vehicle-treated group had increased numbers of GFAP-(+) cells within the deep cortical layers and the underlying white matter in the ipsilateral hemisphere and very few astrocytes in the contralateral hemisphere. The levels of GFAP expression in the corpus callosum, deep cortical layer, external capsule and internal capsule in the ipsilateral hemisphere were markedly higher and more diffuse in the rolipram-treated groups than in the vehicle-treated group. The astrocytes in the rolipram-treated groups had larger cell bodies and thicker processes than those in the vehicle-treated group (Fig. 2A and B). There was no significant difference in the GFAP immunoreactivity between the Rol-0.5, Rol-1 and Rol-3 groups.
Postinsult treatment with rolipram increased the degree of reactive astrogliosis in the ipsilateral hemisphere. GFAP immunostaining in the vehicle-treated group shows more GFAP-(+) cells within the ipsilateral deep cortical layers and white matter (A) than within the contralateral hemisphere. Rolipram treatment markedly and diffusely increases the expression of GFAP in the ipsilateral corpus callosum, deep cortical layer, external capsule and internal capsule (B). The astrocytes in rolipram-treated rats have larger cell bodies and thicker processes than those in the vehicle-treated rats (insets). The vehicle-treated group has increased numbers of ED1-(+) cells in the ipsilateral hemisphere (C). Rolipram treatment markedly increases microglia activation, characterized by large round cell bodies with reduced, thick processes (insets), within the ipsilateral middle and deep parietal cortex and underlying corpus callosum (D). Scale bar: 200 μm in A–D, 100 μm in insets.
In the vehicle-treated group, there were some ED1-(+) cells in the deep parietal cortex and corpus callosum in the ipsilateral hemisphere; in contrast, very few ED1-(+) cells were seen in the contralateral hemisphere. Compared with vehicle treatment, rolipram treatment prominently increased the number of ED1-(+) cells within the ipsilateral deep parietal cortex and underlying corpus callosum. These activated ED1-(+) microglia was characterized by large round cell bodies with reduced and thick processes (Fig. 2C and D). There was no significant difference in the ED1 immunoreactivity between the Rol-0.5, Rol-1 and Rol-3 groups.
Postinsult treatment of rolipram caused diffuse CREB phosphorylation.
There was a marked bilateral increase in pCREB immunoreactivity in the cortex in the rolipram-treated group, which contrasted with the weak pCREB immunoreactivity in the vehicle-treated group (Fig. 3A and B). Double immunofluorescence analysis in the rolipram-treated group showed that pCREB was expressed in the activated microglia and astrocytes, as well as neurons in the ipsilateral hemisphere (Fig 3C–K).
Postinsult treatment with rolipram diffusely increased CREB phosphorylation. There is a marked increase in pCREB immunoreactivity in the cortex and hippocampus in the ipsilateral (A) hemispheres in the rolipram-treated group. In contrast, only weak pCREB immunoreactivity is observed in the vehicle-treated group (B). Immunofluorescent analysis in the rolipram posttreated groups shows that pCREB is expressed in the microglia, neurons and astrocytes of the ipsilateral cerebral cortex; the pCREB-(+) cells co-localize with ED1 (C–E), NeuN (F–H) or GFAP (I–K). Scale bar: 200 μm in A and B, 100 μm in insets and C–K.
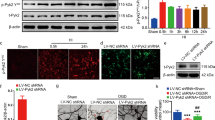
Rolipram treatment decreased the proliferation of preOLs.
In the vehicle-treated HI group, there was a substantial decrease in O1 immunoreactivity in the periventricular white matter and external capsule in the ipsilateral hemisphere after hypoxic-ischemia, as compared with the contralateral hemisphere. There was markedly less O1 immunostaining in the ipsilateral periventricular areas in the rolipram-treated HI groups than in the vehicle-treated HI group (Fig. 4A and B).
Rolipram treatment decreases the proliferation of preoligodendrocytes. Compared with vehicle-treated hypoxia-ischemia (HI) group (A), rolipram-treated HI groups have markedly decreased O1 immunodensity in the ipsilateral hemisphere (B). To examine the effect of rolipram per se on normal white matter development, the proliferating preoligodendrocytes with co-localization of BrdU (red) and O4 (green) (C) were counted in periventricular white matter. There are no significant differences in the O4(+) cells between the rolipram- and vehicle-treated rats (D). The number of O4(+)-BrdU(+) cells in the periventricular white matter is markedly lower in the rolipram-treated group than in the vehicle-treated group (E) (*p < 0.05, unpaired t test, n = 4/group). Scale bar: 50 μm in A and B, 10 μm in C.
To examine the effect of rolipram per se on normal white matter development, rat pups were treated with 3 mg/Kg rolipram or vehicle, concurrent with injection of BrdU, but without HI injury. There were no significant differences in the O4(+) cells between the rolipram-and vehicle-treated rats (Fig. 4D). The number of O4(+)-BrdU(+) cells in the periventricular areas, however, was markedly lower in the rolipram-treated group than in the vehicle-treated group (p < 0.05, Fig. 4C and E).
DISCUSSION
The present study shows that unilateral carotid artery ligation in combination with moderate hypoxia results in selective white matter injury with relatively cortical sparing. Although, the level of CREB phosphorylation increased, rolipram administered after hypoxic-ischemic injury exacerbated the degree of periventricular white matter injury and led to an increase of deep cortical lesions. There was also increased astrogliosis in the ipsilateral periventricular areas and deep cortical layer in the rolipram-treated hypoxic-ischemic group, with increased CREB phosphorylation in these activated microglia and astrocytes. Furthermore, the rolipram-treated hypoxic-ischemic groups had markedly depleted preOLs in the ipsilateral hemisphere, which may be related to decreased preOLs proliferation after rolipram treatment per se. These data suggest that rolipram treatment after hypoxic-ischemia is not protective; in contrast, it may exacerbate neuronal and white matter injury in the neonatal rat brains.
It has been well documented that the cAMP-CREB signaling pathway plays an important neuroprotective role in both immature and mature brains (15,20). Rolipram pretreatment in rat pups has been shown to protect against hypoxic-ischemic neuronal injury via CREB activation (15). It has also been shown that virus-mediated overexpression of CREB protected preOLs from excitotoxicity in vitro and in vivo (12). However, in our study, rolipram posttreatment increased the periventricular white matter and deep cortical neuronal injury. We observed diffuse CREB phosphorylation in activated microglia and astrocytes, in addition to neurons, in the ipsilateral hemisphere after rolipram posttreatment. Previous studies have shown transient neuronal but persistent astroglial CREB activation after focal brain injury, suggesting a crucial role of CREB in perilesional reactive astrogliosis (21). Recent studies suggested that the induction of proinflammatory genes, such as interleukin-6 and tumor necrosis factor-α is mediated via activation of NF-kB and CREB in neonatal glial cells (22). Therefore, differential modulation of target genes by transcription factors, which is region, cell type and time specific, may explain these divergent results for CREB activation (23). Furthermore, rolipram can increase cAMP, which in turn regulates many important intracellular metabolic processes besides its effect on CREB. Many cAMP-dependent and cAMP binding effectors have been identified, and several alternative pathways have been discovered (24). The cellular compartment in which cAMP is released is also of prime importance as it determines which downstream effectors are activated (25). Differential modulation of these targets may explain the divergent effects observed in the various pharmacological agents used in rat models (26).
The deleterious effects of rolipram posttreatment on hypoxic-ischemic white matter injury in neonatal rat brain may be related to the inhibitory effects of rolipram per se on preOLs proliferation. We found that the numbers of preOLs incorporating BrdU in the white matter were significantly lower in rats treated with rolipram than in those treated with vehicle. Oligodendrocytes undergo a series of sequential and well-defined changes in their phenotypic characteristics, gradually evolving from proliferative immature precursors into postmitotic mature cells (27). cAMP-elevating agents can promote preOLs lineage progression and differentiation but may inhibit their proliferation (17,28,29). Although mature oligodendrocytes are more resistant to hypoxic-ischemic injury than preOLs (6–9), rolipram treatment may in fact deplete the number of proliferating preOLs after hypoxic-ischemic injury, as demonstrated in our study.
Much evidence points to a pathologic contribution of microglia toward periventricular white matter damage (30,31). Therefore, anti-inflammatory therapy, such as antenatal betamethasone treatment (32), represents a potential treatment of this disorder. Rolipram has been shown to prevent immune cell activation and proinflammatory cytokine production (17). This does not appear to be the case in the present study, because the degree of astroglosis was significantly higher in the rolipram-treated group than in the vehicle-treated group.
Although PVL is the most recognized injury and the major antecedent to cerebral palsy in preterm babies, clinical magnetic resonance imaging reveals subtle decreases in cortical and deep gray nuclei volume in addition to white matter loss (2). Accordingly, cognitive and learning deficits are prevalent in this population. The present model induced subtle deep cortical neuronal injury associated with a nonsignificant trend of brain atrophy. The deep cortical columnar pattern of damage, rather than laminar damage seen in rats after severe hypoxic-ischemia, is likely to be a reflection of the developmental vulnerability at this stage of cerebral maturation. In addition, this columnar injury is thought to be related to the distribution of immature penetrator vessels in the developing cortex (33). There is growing recognition that oligodendroglial injury in the immature nervous system may have profound adverse effects on neuronal development. This model does not produce overt necrotic lesions as commonly noted in severe hypoxic-ischemic injury of P7 rat pups (16,17), but leads to a PVL-like phenotype that includes subsequent myelination alterations and deep cortical organization defects.
The finding that rolipram posttreatment had a deleterious effect on hypoxic ischemia-induced white matter injury in immature brains was unexpected. Several studies have shown that rolipram treatment after spinal cord injury in adult rats promoted axonal regeneration, enhanced remyelination and functional recovery (16,17). However, studies have shown that the immature brain responds differently than the mature brain to treatment. In the mature nervous system, adenosine exerts protective effects against HI injury. But A1 adenosine receptor activation has deleterious effects on white matter in immature brains (34). It is, therefore, essential to take into consideration that therapy designed to ameliorate brain injury in adults may worsen outcomes in the developing brain.
Abbreviations
- CREB:
-
cAMP response element-binding protein
- MBP:
-
myelin basic protein
- preOLs:
-
pre-oligodendrocytes
- PVL:
-
periventricular leukomalacia
References
Volpe JJ 2001 Neurobiology of periventricular leukomalacia in the premature infant. Pediatr Res 50: 553–562
Huppi PS, Murphy B, Maier SE, Zientara GP, Inder TE, Barnes PD, Kikinis R, Jolesz FA, Volpe JJ 2001 Microstructural brain development after perinatal cerebral white matter injury assessed by diffusion tensor magnetic resonance imaging. Pediatrics 107: 455–460
Volpe JJ 2001 Perinatal brain injury: from pathogenesis to neuroprotection. Ment Retard Dev Disabil Res Rev 7: 56–64
Back SA, Luo NL, Mallinson RA, O'Malley JP, Wallen LD, Frei B, Morrow JD, Petito CK, Roberts CT Jr Murdoch GH, Montine TJ 2005 Selective vulnerability of preterm white matter to oxidative damage defined by F2-isoprostanes. Ann Neurol 58: 108–120
Back SA, Luo NL, Borenstein NS, Levine JM, Volpe JJ, Kinney HC 2001 Late oligodendrocyte progenitors coincide with the developmental window of vulnerability for human perinatal white matter injury. J Neurosci 21: 1302–1312
Baud O, Haynes RF, Wang H, Folkerth RD, Li J, Volpe JJ, Rosenberg PA 2004 Developmental up-regulation of MnSOD in rat oligodendrocytes confers protection against oxidative injury. Eur J Neurosci 20: 29–40
Jensen FE 2006 Developmental factors regulating susceptibility to perinatal brain injury and seizures. Curr Opin Pediatr 18: 628–633
Deng W, Wang H, Rosenberg PA, Volpe JJ, Jensen FE 2004 Role of metabotropic glutamate receptors in oligodendrocyte excitotoxicity and oxidative stress. Proc Natl Acad Sci USA 101: 7751–7756
Rosenberg PA, Dai W, Gan XD, Ali S, Fu J, Back SA, Sanchez RM, Segal MM, Follett PL, Jensen FE, Volpe JJ 2003 Mature myelin basic protein-expressing oligodendrocytes are insensitive to kainate toxicity. J Neurosci Res 71: 237–245
Afshari FS, Chu AK, Sato-Bigbee C 2001 Effect of cyclic AMP on the expression of myelin basic protein species and myelin proteolipid protein in committed oligodendrocytes: differential involvement of the transcription factor CREB. J Neurosci Res 66: 37–45
Sato-Bigbee C, Chan EL, Yu RK 1994 Oligodendroglial cyclic AMP response element-binding protein: a member of the CREB family of transcription factors. J Neurosci Res 38: 621–628
Deng W, Neve RL, Rosenberg PA, Volpe JJ, Jensen FE 2006 Alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionate receptor subunit composition and cAMP-response element-binding protein regulate oligodendrocyte excitotoxicity. J Biol Chem 281: 36004–36011
O'Donnell JM, Zhang HT 2004 Antidepressant effects of inhibitors of cAMP phosphodiesterase (PDE4). Trends Pharmacol Sci 25: 158–163
Chang YC, Tzeng SF, Yu L, Huang AM, Lee HT, Huang CC, Ho CJ 2006 Early-life fluoxetine exposure reduced functional deficits after hypoxic-ischemia brain injury in rat pups. Neurobiol Dis 24: 101–113
Lee HT, Chang YC, Wang LY, Wang ST, Huang CC, Ho CJ 2004 cAMP response element-binding protein activation in ligation preconditioning in neonatal brain. Ann Neurol 56: 611–623
Nikulina E, Tidwell JL, Dai HN, Bregman BS, Filbin MT 2004 The phosphodiesterase inhibitor rolipram delivered after a spinal cord lesion promotes axonal regeneration and functional recovery. Proc Natl Acad Sci USA 101: 8786–8790
Pearse DD, Pereira FC, Marcillo AE, Bates ML, Berrocal YA, Filbin MT, Bunge MB 2004 cAMP and Schwann cells promote axonal growth and functional recovery after spinal cord injury. Nat Med 10: 610–616
Follett PL, Rosenberg PA, Volpe JJ, Jensen FE 2000 NBQX attenuates excitotoxic injury in developing white matter. J Neurosci 20: 9235–9241
Sizonenko SV, Sirimanne E, Mayall Y, Gluckman PD, Inder T, Williams C 2003 Selective cortical alteration after hypoxic-ischemic injury in the very immature rat brain. Pediatr Res 54: 263–269
Lonze BE, Ginty DD 2002 Function and regulation of CREB family transcription factors in the nervous system. Neuron 35: 605–623
Carbonell WS, Mandell JW 2003 Transient neuronal but persistent astroglial activation of ERK/MAP kinase after focal brain injury in mice. J Neurotrauma 20: 327–336
Lee B, Dziema H, Lee KH, Choi YS, Obrietan K 2007 CRE-mediated transcription and COX-2 expression in the pilocarpine model of status epilepticus. Neurobiol Dis 25: 80–91
Chang YC, Huang CC 2006 Perinatal brain injury and regulation of transcription. Curr Opin Neurol 19: 141–147
Bos JL 2003 Epac: a new cAMP target and new avenues in cAMP research. Nat Rev Mol Cell Biol 4: 733–738
MacKenzie SJ, Houslay MD 2000 Action of rolipram on specific PDE4 cAMP phosphodiesterase isoforms and on the phosphorylation of cAMP-response-element-binding protein (CREB) and p38 mitogen-activated protein (MAP) kinase in U937 monocytic cells. Biochem J 347: 571–578
Mansuy I 2004 A constraint on cAMP signaling. Neuron 41: 4–6
Baumann N, Pham-Dinh D 2001 Biology of oligodendrocyte and myelin in the mammalian central nervous system. Physiol Rev 81: 871–927
Raible DW, McMorris FA 1993 Oligodendrocyte differentiation and progenitor cell proliferation are independently regulated by cyclic AMP. J Neurosci Res 34: 287–294
Garcia C, Paez P, Davio C, Soto EF, Pasquini JM 2004 Apotransferrin induces cAMP/CREB pathway and cell cycle exit in immature oligodendroglial cells. J Neurosci Res 78: 338–346
Back SA, Rivkees SA 2004 Emerging concepts in periventricular white matter injury. Semin Perinatol 28: 405–414
Lehnardt S, Lachnance C, Patrizi S, Lefebvre S, Follett PL, Jensen FE, Rosenberg PA, Volpe JJ, Vartanian T 2002 The toll-like receptor TLR4 is necessary for lipopolysaccharide-induced oligodencrocyte injury in the CNS. J Neurosci 22: 2478–2486
Baud O, Foix-L'Helias L, Kaminski M, Audibert F, Jarreau PH, Papiernik E, Huon C, Lepercq J, Dehan M, Lacaze-Masmonteil T 1999 Antenatal glucocorticoid treatment and cystic periventricular leukomalacia in very premature infants. N Engl J Med 341: 1190–1196
Sizonenko SV, Kiss JZ, Inder T, Gluckman PD, Williams CE 2005 Distinctive neuropathologic alterations in the deep layers of the parietal cortex after moderate ischemic-hypoxic injury in the P3 immature rat brain. Pediatr Res 57: 865–872
Back SA, Craig A, Luo NL, Ren J, Akundi RS, Ribeiro I, Rivkees SA 2006 Protective effects of caffeine on chronic hypoxia-induced perinatal white matter injury. Ann Neurol 60: 696–705
Acknowledgements
We thank Chien-Jung Ho and Yu-Chen Lin, for their skillful technical assistance in the laboratory and with animal preparations.
Author information
Authors and Affiliations
Additional information
Supported by grants from the Taiwan National Science Counsel (NSC: 94-2314-B-182A-089, 95-2314-B-182A-014), and Chang Gung Memorial Hospital Research Program (CGMHG-850381).
Rights and permissions
About this article
Cite this article
Chang, YC., Huang, CC., Hung, PL. et al. Rolipram, a Phosphodiesterase Type IV Inhibitor, Exacerbates Periventricular White Matter Lesions in Rat Pups. Pediatr Res 64, 234–239 (2008). https://doi.org/10.1203/PDR.0b013e31817cfc87
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31817cfc87