Abstract
Patent ductus arteriosus (PDA) complicates the hospital course of premature infants. Impaired oxygen (O2)-induced vasoconstriction in preterm ductus arteriosus (DA) contributes to PDA and results, in part, from decreased function/expression of O2-sensitive, voltage-gated potassium channels (Kv) in DA smooth muscle cells (DASMCs). This paradigm suggests that activation of the voltage-sensitive L-type calcium channels (CaL), which increases cytosolic calcium ([Ca2+]i), is a passive consequence of membrane depolarization. However, effective Kv gene transfer only partially matures O2 responsiveness in preterm DA. Thus, we hypothesized that CaL are directly O2 sensitive and that immaturity of CaL function in preterm DA contributes to impaired O2 constriction. We show that preterm rabbit DA rings have reduced O2- and 4-aminopyridine (Kv blocker)–induced constriction. Preterm rabbit DASMCs have reduced O2-induced whole-cell calcium current (ICa) and [Ca2+]i. BAY K8644, a CaL activator, increased O2 constriction, ICa, and [Ca2+]i in preterm DASMCs to levels seen at term but had no effect on human and rabbit term DA. Preterm rabbit DAs have decreased γ and increased α subunit protein expression. We conclude that the CaL in term rabbit and human DASMCs is directly O2 sensitive. Functional immaturity of CaL O2 sensitivity contributes to impaired O2 constriction in premature DA and can be reversed by BAY K8644.
Similar content being viewed by others
Main
In the hypoxic environment in utero, the ductus arteriosus (DA), a vital fetal artery that connects the pulmonary artery to the aorta, is widely patent and shunts more than half of the right heart's cardiac output away from the nonventilated lung into the umbilicoplacental circulation, where gas exchange takes place (1). Within minutes of birth, the increased Po2 constricts the DA (2) and simultaneously dilates the pulmonary circulation (3). The response of the term DA to oxygen (O2) rarely fails; however, in humans, approximately 50% of preterm DAs do not close, despite adequate oxygenation (4). Failure of DA closure after birth complicates the hospital course of preterm infants. PDA is associated with an increased incidence of chronic lung disease, intraventricular hemorrhage, and necrotizing enterocolitis (4). Both medical and surgical interventions to close the DA, although usually effective, are associated with additional morbidity (5).
The crucial role of endothelium-derived relaxing and constricting factors in regulating DA tone is well established (6). However, O2 constricts the DA in the absence of endothelium (7), suggesting that the core of the O2-sensing mechanism is intrinsic to the DA smooth muscle cell (DASMC). Potassium (K+) channels in the vascular smooth muscle cells (SMCs) regulate vascular tone through modulation of the membrane potential (EM) (8). Closure of K+ channels leads to vasoconstriction by depolarizing EM. Depolarization opens voltage-gated L-type calcium (Ca2+) channels (CaL), thereby increasing influx of extracellular Ca2+. In term rabbit (9) and human (10) DAs, O2-induced constriction is initiated by the inhibition of O2 and 4-aminopyridine (4-AP)–sensitive voltage-gated, K+ channels (Kv), including Kv1.5 and Kv2.1. Preterm rabbit DAs have reduced O2 constriction due, in part, to decreased function and expression of O2-sensitive Kv (11). Kv1.5 or Kv2.1 gene transfer partially (50%) “rescues” the developmental deficiency, conferring O2 responsiveness to preterm rabbit DAs and human DAs (11). However, O2 responsiveness is not completely restored, suggesting additional mechanisms contribute to O2-induced constriction in the DASMCs. In resistance pulmonary artery SMC, another cell from the specialized O2-sensing system (12), the CaL have intrinsic O2 sensitivity in addition to their response to Kv inhibition–induced depolarization of EM (13). We suggest that DASMC CaL are more active participants in DA constriction to O2 than was previously recognized, responding not just to membrane depolarization but directly to increased Po2. We tested the hypothesis that the CaL are intrinsically O2 sensitive in rabbit and human DASMCs. We also tested the hypothesis that reduced expression and/or function of these channels contributes to impaired O2 constriction in preterm rabbit DA.
METHODS
All procedures were approved by the Animal Welfare and the Human studies committees of the University of Alberta. All investigators had access to the data and take responsibility for its integrity.
Rabbit DAs.
New Zealand White rabbits (n = 50) were delivered by cesarean section at gestational d 26 (preterm) or 30 (term), as previously described (11,14). The endothelium-intact DA was used within 5 min of harvest and was maintained hypoxic (pH = 7.40 ± 0.08, Po2 = 31 ± 1 mm Hg) until Po2 was intentionally increased.
Rabbit DASMCs.
DASMCs were obtained by enzymatic digestion as described (11,14).
Human DASMCs.
Human DAs were obtained from hypoplastic left heart term infants during the Norwood procedure, and the SMCs were isolated by enzymatic digestion, as described (11,14).
Tension measurements in isolated preterm and term rabbit DA rings.
Isolated rabbit DAs were placed in an organ bath and equilibrated in hypoxic Krebs solution (Po2 = 31 ± 1 mm Hg to mimic in utero conditions), at the experimentally derived optimal resting tension values of 400 mg (preterm) and 800 mg (term), as previously described (11,14). To investigate the contribution of maturational differences in CaL function to diminished O2 constriction, the response of preterm and term DA rings to increased Po2 was compared in the presence and absence of the CaL opener BAY K8644 (10−6M) or the CaL inhibitor nifedipine (10−6M). The responsiveness to K+ channel inhibitors Kv inhibitor 4-AP and iberiotoxin (IBTX), a highly specific inhibitor of large conductance calcium-sensitive K+ channels (BKCa) was also compared.
Whole cell patch clamp.
The effect of Po2 on whole-cell Ca2+ current (ICa) and EM were measured in freshly dispersed preterm and term rabbit DASMCs and human DASMCs, using voltage and current clamp protocols, as previously described (11,15) and detailed in the online supplement. Ca2+ channel current recordings were obtained using the whole-cell configuration. Barium (20 mM) was used as a charge carrier because its favorable conduction by the CaL increases current amplitude.
The current-voltage relationship was obtained using a voltage-step protocol (from −60 to +50 mV, duration of 250 ms in 10-mV increments in hypoxic, Po2 = 40 mm Hg, perfusate). The effects of increasing O2 (Po2 = 165 mm Hg) and the CaL agonist BAY K8644 on ICa were studied.
Intracellular calcium [Ca2+]i measurements.
Ca2+ was measured using a spectrofluorometer (Photon Technology International, Birmingham, NJ). Cells were incubated with fura 2-AM (10−6 M) and pluronic (8 × 10−7 M) (Molecular Probes, Eugene, OR) for 20 min in 4% O2. The plates were then washed with hypoxic Hanks' balanced salt solution and incubated in a 4% O2 incubator for an additional 20 min, with or without BAY K8644 (1 μM) (Sigma Chemical Co.-Aldrich, St. Louis, MO). Plates were placed on the stage of an inverted microscope and perfused with a warmed normoxic Hanks' solution (32–33°C). Background fluorescence was recorded from each dish of cells and subtracted before calculation of the 340- to 380-nm ratio. Emission was measured at 510 nm. Duration of each measurement was 1200 s.
Immunoblotting.
DAs were flash frozen in liquid N2 and homogenized in buffer containing an antiprotease cocktail (Sigma Chemical Co.) and run on 7.5%–10% gels. Specific antibodies against CaL subunits α1c and γ2 were purchased from US Biologic (Cedarlane Laboratories Ltd., Hornby, Ontario) and Sigma Chemical Co.-Aldrich, respectively. Expression was quantified using densitometry and expressed as the percentage of the loaded protein density, measured using the Ponceau stain.
Statistics.
Values are expressed as means ± SEM. All sample sizes are listed in the figures. Intergroup comparisons were performed with a t test or factorial repeated-measures analysis of variance, as appropriate. Fisher's probable least significant differences test was used for post hoc comparisons. A p value <0.05 was considered statistically significant.
RESULTS
Decreased O2-induced constriction in preterm rabbit DA is restored by a CaL opener.
In both term and preterm DAs, O2-induced constriction increased in proportion to Po2 (Fig. 1A, B). O2-induced constriction was significantly weaker in preterm DAs (Fig. 1A, B). Pretreatment with the CaL opener BAY K8644 enhanced O2-induced constriction in preterm DAs to a magnitude similar to that achieved in term DAs (Fig. 1A, B). In contrast, BAY K8644 had no effect on O2-induced constriction in term DAs. BAY K8644 had no effect on phenylephrine-induced constriction in preterm and term DAs (data nor shown). The Ca2+ channel inhibitor nifedipine blunted O2 constriction in both preterm and term DAs (by 60% in 20% O2), suggesting a crucial role of extracellular calcium influx through the CaL in O2-induced constriction in this acute phase of O2-induced DA constriction (Fig. 1A, B).
Reduced O2-induced constriction in preterm DA rings is overcome by CaL activation. Representative tracings (A) and mean data (B) showing decreased O2-induced constriction in preterm vs term DA. In preterm DAs, pretreatment with the CaL opener BAY K8644 significantly increases O2-induced constriction to a magnitude similar to that of term DA (n = 10–15; *p < 0.05). BAY K8644 does not increase O2-induced constriction in term DA (n = 10–15, *p < 0.05 vs term vehicle; †p < 0.05 vs preterm vehicle. Preterm vehicle (white columns), term vehicle (black columns), preterm BAY K8644 (light gray columns), term BAY K8644 (dark gray columns). The CaL inhibitor nifedipine reduces O2-induced constriction in preterm and term DA by 60% (preterm nifedipine (light gray columns), term nifedipine (dark gray columns).
Opening CaL does not affect Kv inhibition–induced constriction in rabbit DA.
In both term and preterm DAs, the Kv blocker 4-AP (1, 5, and 10 mM) caused a dose-dependent constriction (Fig. 2A). Kv inhibition was weaker in preterm than in term DAs. Pretreatment with BAY K8644 had no effect on 4-AP–induced constriction in preterm or term DA (Fig. 2A). Conversely, pretreatment of preterm and term DA with BAY K8644 significantly enhanced BKCa-induced constriction, although this constriction was very small compared with that induced by either increased Po2 or 4-AP (Fig. 2B).
Effect of CaL activation on K+ channel blockade in preterm and term DASMCs. (A) In both term and preterm DAs, 4-AP causes a dose-dependent constriction. Kv inhibition is weaker in preterm than in term DAs, consistent with Kv immaturity. Pretreatment with BAY K8644 has no effect on 4-AP–induced constriction in either preterm or term DA (n = 10–15, *p < 0.05, preterm vehicle (white columns), preterm BAY K8644 (light gray columns), term vehicle (black columns), term BAY K8644 (dark gray columns).(B) Pretreatment of preterm and term DA with BAY K8644 significantly enhances BKCa inhibition–induced constriction with IBTX (n = 10–15; *p < 0.05; vehicle (white columns), BAY K8644 (black columns).
EM is unchanged by the CaL opener BAY K8644.
In hypoxia (Po2 = 40 mm Hg), preterm rabbit DASMCs are more depolarized than term DASMCs (Fig. 3A). As expected, BAY K8644 had no effect on EM in either term or preterm DA.
ICa is reduced in preterm DASMCs but can be increased by BAY K8644. (A) In hypoxia (Po2 = 40 mm Hg), preterm rabbit DASMCs are more depolarized than term DASMCs (n = 7, **p < 0.01). BAY K8644 has no effect on EM in either term or preterm DA (vehicle, white columns; BAY K8644, black columns). (B) Compared with term DASMCs (n = 16, solid triangle), preterm DASMCs (n = 19, solid circle) have decreased ICa. BAY K8644 significantly increases ICa in preterm DASMCs (open circles) to term (open triangles) values. BAY K8644 also increases ICa in term DASMCs (*p < 0.05, **p < 0.01). (C) Time to maximal increase in ICa caused by BAY K8644 is the same in term (ET50 2.89 min, solid squares) and preterm DASMCs (open squares, ET50 3.19 min, *p < 0.05, n = 10). However, the percentage of increase in ICa is significantly greater in preterm DASMCs.
Compared with hypoxic term DASMCs, hypoxic preterm DASMCs have decreased ICa (Fig. 3B). BAY K8644 increases ICa in hypoxic term and preterm rabbit DASMCs. In hypoxic preterm DASMCs, BAY K8644 enhances ICa to levels similar to those in term DASMCs. BAY K8644 also increased ICa in term DASMCs (Fig. 3B). Although the time to maximal increase in ICa caused by BAY K8644 was the same in term and preterm DASMCs, the percentage of increase in ICa was significantly greater in preterm DASMCs (Fig. 3C).
DASMC CaL are O2 sensitive and this sensitivity is absent in preterm rabbit DASMCs.
In term rabbit DAs, O2 significantly increased ICa (Fig. 4A). This effect is evident beginning at EM −25 mV (Fig. 4A). In contrast, O2 did not alter ICa in preterm rabbit DASMCs (Fig. 4B). BAY K8644 increased ICa in preterm rabbit DASMCs. The increase in ICa caused by BAY K8644 was the same whether it was given in normoxia or hypoxia (Fig. 4B). In term human DASMCs, O2 significantly increased ICa (Fig. 4C). This increase was largely eliminated by the CaL blocker nicardipine (Fig. 4C).
DASMC CaL are O2 sensitive, and this sensitivity is absent in preterm DASMCs. (A) O2 increases ICa in term (open triangles), but not preterm DASMCs (open circles). Solid circles and solid triangles represent term and preterm DASMCs in hypoxia, respectively. The bar graph highlights the effects at physiologic membrane potentials (n = 6–7 per group, *p < 0.05, **p < 0.01). Open columns, preterm hypoxia; solid columns, preterm normoxia; hatched columns, term hypoxia; cross-hatched columns, term normoxia. (B) BAY K8644 significantly increases ICa in hypoxic term and preterm DASMCs but does not increase ICa during normoxia in term DASMCs (n = 7–12, *p < 0.05). Solid circles, hypoxia; open circles, normoxia; solid triangles, hypoxia + BAY K8644; open triangles, normoxia + BAY K8644. (C) CaL in human term DASMCs also display O2 sensitivity. The O2-induced increase in ICa is abolished by the CaL blocker nicardipine (n = 6, **p < 0.01). Solid circles, normoxia; open circles, hypoxia; open triangles, normoxia + nicardipine.
Oxygen elicits less increase in [Ca2+]i in preterm versus term DASMCs.
[Ca2+]i increased less in preterm versus term DASMCs upon 20 min of exposure to increased Po2 (Fig. 5). BAY K8644 significantly enhanced [Ca2+]i after O2 exposure in preterm DASMCs, bringing it to levels similar to those achieved without BAY K8644 in term DA. BAY K8644 had no additional effect on [Ca2+]i in term DA beyond that achieved by increased Po2.
Decreased [Ca2+]i in preterm DASMCs can be enhanced by BAY K8644. O2 causes a smaller increase in [Ca2+]i in preterm DASMCs as compared with term DASMCs. BAY K8644 significantly enhances the Po2- induced increases in [Ca2+]i in preterm, but not in term DASMCs (*p < 0.05 vs hypoxia (H), **p < 0.01 vs hypoxia, †p < 0.05 vs normoxia (N), n = 5 per group).
Expression of CaL α subunit is increased but γ subunit is decreased in preterm DA.
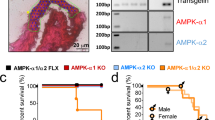
Immunoblotting showed increased α1c subunit expression in preterm DAs in pooled specimens derived from four term and four preterm DAs (Fig. 6). In contrast, expression of the CaL's γ2 subunit was significantly decreased in preterm compared with term DAs.
Preterm DAs have conserved expression of the pore-forming α subunit of CaL but express less of the CaL γ2 subunit. (A) Immunoblot showing increased protein expression of the putative O2-sensing α1c subunit in preterm compared with term rabbit DAs. (B). The γ2 subunit in preterm rabbit DAs is decreased compared with term DAs (n = 4 per group, *p < 0.05).
DISCUSSION
Vasoconstriction of the DA in response to increased Po2 is a robust response that is a major determinant of functional closure of the DA, a crucial step in the transition of the fetal circulation at birth. It is not surprising that a response so essential to the neonate's postnatal adaptation is mediated by multiple, complementary mechanisms. The preterm rabbit DAs (at 26 d of gestation) offers an ideal model in which to explore the mechanisms that must mature to permit DA constriction and closure at term (11). Patency is favored in preterm DA by several mechanisms, including (relative to term DA) increased production of vasodilator prostanoids (6), reduced production of endothelin (6), decreased expression and function of O2-sensitive Kv (6,11) and more recently decreased rho-kinase activity (16,17). The current investigation identifies a new, developmentally regulated mechanism of O2 sensitivity that is absent in preterm DA and that contributes to O2-induced constriction in term DAs. We demonstrate for the first time that the CaL in term rabbit and human DASMCs are intrinsically O2 sensitive and that impaired O2 constriction in preterm DAs results, in part, from decreased CaL activation by increases in Po2 that mimic birth (40 to 100 mm Hg) (Fig. 7). The immaturity of the CaL is evident both physiologically and electrophysiologically. In DA rings from premature rabbits, O2 constriction is reduced but can be restored to term levels by administration of BAY K8644, which increases the opening of CaL (Fig. 1).
Proposed mechanism for impaired CaL-mediated O2 constriction. (Left) Previous work showed that term DAs respond with constriction to O2, in part due to intact function/expression of the O2-sensitive Kv, which results in depolarization and CaL activation. (Right) In addition to a reduced Kv-EM mechanism in preterm DAs, new data show that O2 directly activates CaL in term DAs (arrow) and that this mechanism is lacking in preterm DAs, but can be restored by BAY K8644. This explains why a CaL opener (BAY K8644) increases O2 constriction in preterm DAs to a magnitude similar to that in term DAs.
The observation that pharmacological activation of CaL with BAY K8644 rapidly restores O2-induced constriction in preterm DA to the same magnitude as that observed in term DA and likewise increases ICa and [Ca2+]i suggests that CaL are present in preterm DA, but somehow are not activated in response to O2 alone. Moreover, this response to BAY K8644 seems relatively specific for the effects of increased O2. BAY K8644 does not enhance the constrictor response to 4-AP (Fig. 2) or phenylephrine (data not shown). The fact that BAY K8644 does not enhance constriction or increase ICa in term DA may reflect the relative hyperpolarization of term DASMCs (Fig. 3A). BAY K8644 has little effect on vascular tone unless there is depolarization and our findings in hypoxic term DAs are consistent with BAY K8644's lack of effect on the normoxic pulmonary vascular resistance in normal lungs (18). Moreover, BAY K8644 had no effect on tension or calcium influx in rabbit aorta when they were maximally activated by high K+ depolarization, whereas it enhanced norepinephrine constriction and calcium influx (19). Likewise, BAY K8644 had no effect on 4-AP constriction in DA. This suggests that in oxygenated term DA, maximal depolarization has occurred, reducing the possibility of an additive effect on CaL opening. BAY K8644 exerts its effects (enhancing cardiac contractility and increasing vascular tone) by increasing the open probability of the calcium channels evoking a shift of the open-probability curve to more negative EM (20). In term DASMCs, adequate O2-sensitive Kv ensure that increased Po2 achieves maximal depolarization and CaL activation via a voltage-dependent mechanism. Perhaps BAY K8644 selectively enhances O2 constriction in preterm DAs because they have an immature O2-sensitive Kv channel mechanism. We now show that oxygen's ability to activate the CaL and increase calcium influx relies in part on the intrinsic O2-sensitivity of the CaL. This mechanism of CaL activation is dificient in preterm DASMC and this deficiency can be overcome by administration of the CaL opener BAY K8644. In preterm DASMC BAY K8644 enhances CaL opening and shifts the activation threshold, allowing it to occur at relatively more physiological (negative) membrane potentials (Fig 4A).
On an electrophysiological level, the use of the patch-clamp technique allowed us to examine the effects of Po2 on ICa, independent on changes in EM caused by Kv inhibition. These studies show that the premature DASMC has reduced ICa, but that this is restored to term levels with the addition of BAY K8644 (Fig. 4B). Even more importantly, whereas an increase in Po2 increases ICa in term DASMCs, there is no effect on preterm ICa (Fig. 4B). Thus, much like Kv, the function of which is reduced in preterm DAs (11), the CaL's function is also reduced. However, unlike the Kv channel, whose expression is decreased (11), expression of the α1c subunit, the putative O2-sensing subunit of CaL, is paradoxically increased in premature DASMC in the face of reduced Ca2 function (Fig. 6).
More recently, we identified a unique O2 sensor in the DA comprised of a sensor, the proximal electron transport chain of the mitochondria, that produces a diffusible mediator (H2O2) that inhibits redox-sensitive Kv promoting constriction (7,9,10,15,21) (Fig. 7). Reduced expression and function of putative O2-sensing Kv1.5 and Kv2.1 in preterm DAs appear to contribute to DA patency in preterm newborn rabbits. Kv1.5 or Kv2.1 overexpression in preterm rabbit DAs does not restore O2 response to term DA levels (rather it reaches 50% of term constriction) (11). Kv gene therapy confers 300–400 mg of constriction to the ductus exposed to oxygen versus 800 mg in the normal term ductus without gene therapy. In contrast, BAY K8644 fully restores O2 sensitivity in preterm DAs (Fig. 1B). With BAY K8644 pretreatment, there was no difference between O2-induced constriction in preterm DAs (light gray columns) versus untreated term DAs (black columns). This suggests that CaL are present but functionally immature in preterm DAs.
O2 sensitivity of K+ channels have been described in various specialized, O2-sensing tissues such as chemoreceptors in the carotid body, the pulmonary SMCs, neuroepithelial bodies, the placenta, and adrenal chromaffin cells (12). More recently, CaL in vascular SMCs (13,22,23) and carotid body chemoreceptor cells (24) have been shown to be O2 sensitive. Whereas hypoxia reversibly inhibits CaL in SMCs from systemic arteries and proximal pulmonary arteries [vessels where hypoxia causes vasodilatation (22)], hypoxia activates CaL in resistance pulmonary artery SMCs (25), suggesting that rather than solely responding to Kv-determined changes in EM, CaL actively contribute to hypoxic pulmonary vasoconstriction. Here we demonstrate a similar phenomenon: CaL in DASMCs are directly O2 sensitive in that increased Po2 rapidly and reversibly increases ICa in freshly isolated term rabbit DASMCs (Fig. 3). The activation of CaL increases [Ca2+]i, leading to DA constriction (Fig. 5). The fact that the O2 sensitivity of the channel is deficient in preterm DAs and can be restored by BAY K8644 (which also restores O2 constriction in premature DA rings) suggests that there are two nonadditive means of activating maximally the CaL: depolarization (which requires Kv inhibition) and activation of CaL by O2 (which is enhanced by BAY K8644).
In both term and preterm DAs approximately two thirds of O2 constriction depends on calcium influx via the CaL and thus is inhibited by a CaL blocker, consistent with previous reports (9,16,17). The remaining one third of constriction appears to reflect calcium sensitization (i.e. rho-kinase activation) and persists in the absence of extracellular calcium and inhibition of sarcoplasmic reticulum calcium release (17). The rho-kinase pathway also displays functional immaturity in preterm DAs (17).
CaL are composed of a central pore-forming, voltage-sensing α1 subunit and auxiliary subunits including various isoforms of β, δ, and γ (26–28). α1c is the putative O2-sensing subunit, and work by Fearon et al. (29,30) indicate that auxiliary subunits are not necessary for O2 sensing in the human cardiac CaL. Several splice variants of the α1 subunits exist. The rat DA predominantly expresses α1C and α1G subunits (31). The α1C subunit is highly expressed in the DA's neointimal cushion (31), where proliferating and migrating SMCs are abundant. This localization is consistent, with such channels contributing to both functional and anatomical closure of the DA, although mechanistic studies are lacking.
To our knowledge, the role of auxiliary CaL subunits in the vasculature is unknown. Term rabbit DAs strongly express the γ2 subunit, whereas preterm rabbit DA express very little of the γ2 subunit (Fig. 6). We speculate that the γ2 subunit is somehow important in conferring O2 sensitivity and/or BAY K8644 responsiveness to CaL in term DASMCs. Further studies will be required to evaluate the putative role of CaL subunits in the diminished O2 sensitivity of ICa in preterm DASMCs.
Maturational changes in DASMC electrophysiology are not the only factors favoring patency of the preterm DA; the endothelium has a major modulatory role. O2 responsiveness of the term DA is reinforced by reduced synthesis and reduced responsiveness to endothelium-derived vasodilating prostaglandins (32,33) and perhaps by increased endothelin-1 production (10,34–36).
In conclusion, we demonstrate that CaL in DASMCs are O2 sensitive and that impaired O2 constriction in preterm DA results in part from decreased O2 activation of CaL. Reduced O2 constriction in preterm rabbit DA can be overcome by enhancing/prolonging CaL activation with BAY K8644. O2-induced activation of CaL in the DASMCs is a novel additional mechanism contributing to DA closure (Fig. 7). With the growing interest in developing selective CaL blockers and activators for a variety of diseases associated with Ca2+ channelopathies (including fertility, neuronal growth, bone formation, and epilepsy) (28), modulation of DA patency can be added to this list of potential therapeutic targets.
Abbreviations
- 4-AP:
-
4-aminopyridine
- [Ca2+]i:
-
cytosolic calcium
- CaL:
-
L-type Ca2+ channels
- DA:
-
ductus arteriosus
- EM:
-
membrane potential
- ICa:
-
whole-cell calcium current
- Kv:
-
voltage-gated K+ channels
- SMC:
-
smooth muscle cell
References
Heymann MA, Rudolph AM 1975 Control of the ductus arteriosus. Physiol Rev 55: 62–78
Kennedy JA, Clark SL 1942 Observations on the physiological reactions of the ductus arteriosus. Am J Physiol 136: 140–147
Abman S, Kinsella J, Mercier J 1999 Nitric oxide and endothelin in the developing pulmonary circulation: physiologic and clinical implications. In: Gaultier CBJ, Post M (eds) Lung Development. Oxford University Press, New York, pp 196–102
Clyman RI 2000 Ibuprofen and patent ductus arteriosus. N Engl J Med 343: 728–730
Koehne PS, Bein G, Alexi-Meskhishvili V, Weng Y, Buhrer C, Obladen M 2001 Patent ductus arteriosus in very low birthweight infants: complications of pharmacological and surgical treatment. J Perinat Med 29: 327–334
Smith GC 1998 The pharmacology of the ductus arteriosus. Pharmacol Rev 50: 35–58
Fay FS 1971 Guinea pig ductus arteriosus. I. Cellular and metabolic basis for oxygen sensitivity. Am J Physiol 221: 470–479
Weir EK, Archer SL 1995 The mechanism of acute hypoxic pulmonary vasoconstriction: the tale of two channels. FASEB J 9: 183–189
Tristani-Firouzi M, Reeve HL, Tolarova S, Weir EK, Archer SL 1996 Oxygen-induced constriction of rabbit ductus arteriosus occurs via inhibition of a 4-aminopyridine-, voltage-sensitive potassium channel. J Clin Invest 98: 1959–1965
Michelakis E, Rebeyka I, Bateson J, Olley P, Puttagunta L, Archer S 2000 Voltage-gated potassium channels in human ductus arteriosus. Lancet 356: 134–137
Thebaud B, Michelakis ED, Wu XC, Moudgil R, Kuzyk M, Dyck JR, Harry G, Hashimoto K, Haromy A, Rebeyka I, Archer SL 2004 Oxygen-sensitive Kv channel gene transfer confers oxygen responsiveness to preterm rabbit and remodeled human ductus arteriosus: implications for infants with patent ductus arteriosus. Circulation 110: 1372–1379
Weir EK, Lopez-Barneo J, Buckler KJ, Archer SL 2005 Acute oxygen-sensing mechanisms. N Engl J Med 353: 2042–2055
Franco-Obregon A, Urena J, Lopez-Barneo J 1995 Oxygen-sensitive calcium channels in vascular smooth muscle and their possible role in hypoxic arterial relaxation. Proc Natl Acad Sci USA 92: 4715–4719
Thebaud B, Michelakis E, Wu XC, Harry G, Hashimoto K, Archer SL 2002 Sildenafil reverses O2 constriction of the rabbit ductus arteriosus by inhibiting type 5 phosphodiesterase and activating BK(Ca) channels. Pediatr Res 52: 19–24
Michelakis ED, Rebeyka I, Wu X, Nsair A, Thebaud B, Hashimoto K, Dyck JR, Haromy A, Harry G, Barr A, Archer SL 2002 O2 sensing in the human ductus arteriosus: regulation of voltage-gated K+ channels in smooth muscle cells by a mitochondrial redox sensor. Circ Res 91: 478–486
Hong Z, Hong F, Olschewski A, Cabrera JA, Varghese A, Nelson DP, Weir EK 2006 Role of store-operated calcium channels and calcium sensitization in normoxic contraction of the ductus arteriosus. Circulation 114: 1372–1379
Kajimoto H, Hashimoto K, Bonnet SN, Haromy A, Harry G, Moudgil R, Nakanishi T, Rebeyka I, Thebaud B, Michelakis ED, Archer SL 2007 Oxygen activates the Rho/Rho-kinase pathway and induces RhoB and ROCK-1 expression in human and rabbit ductus arteriosus by increasing mitochondria-derived reactive oxygen species: a newly recognized mechanism for sustaining ductal constriction. Circulation 115: 1777–1788
Tolins M, Weir EK, Chesler E, Nelson DP, From AH 1986 Pulmonary vascular tone is increased by a voltage-dependent calcium channel potentiator. J Appl Physiol 60: 942–948
Yamamoto H, Hwang O, Van Breemen C 1984 Bay K8644 differentiates between potential and receptor operated Ca2+ channels. Eur J Pharmacol 102: 555–557
Bechem M, Gross R, Hebisch S, Schramm M 1989 Ca-agonists: a new class of inotropic drugs. Basic Res Cardiol 84: 105–116
Roulet MJ, Coburn RF 1981 Oxygen-induced contraction in the guinea pig neonatal ductus arteriosus. Circ Res 49: 997–1002
Franco-Obregon A, Lopez-Barneo J 1996 Low PO2 inhibits calcium channel activity in arterial smooth muscle cells. Am J Physiol 271: H2290–H2299
Franco-Obregon A, Montoro R, Urena J, Lopez-Barneo J 1996 Modulation of voltage-gated Ca2+ channels by O2 tension. Significance for arterial oxygen chemoreception. Adv Exp Med Biol 410: 97–103
Montoro RJ, Urena J, Fernandez-Chacon R, Alvarez de Toledo G, Lopez-Barneo J 1996 Oxygen sensing by ion channels and chemotransduction in single glomus cells. J Gen Physiol 107: 133–143
Franco-Obregon A, Lopez-Barneo J 1996 Differential oxygen sensitivity of calcium channels in rabbit smooth muscle cells of conduit and resistance pulmonary arteries. J Physiol 491: 511–518
Rousset M, Cens T, Restituito S, Barrere C, Black JL 3rd, McEnery MW, Charnet P 2001 Functional roles of gamma2, gamma3 and gamma4, three new Ca2+ channel subunits, in P/Q-type Ca2+ channel expressed in Xenopus oocytes. J Physiol 532: 583–593
Striessnig J, Hoda JC, Koschak A, Zaghetto F, Mullner C, Sinnegger-Brauns MJ, Wild C, Watschinger K, Trockenbacher A, Pelster G 2004 L-type Ca2+ channels in Ca2+ channelopathies. Biochem Biophys Res Commun 322: 1341–1346
Triggle DJ 2006 L-type calcium channels. Curr Pharm Des 12: 443–457
Fearon IM, Palmer AC, Balmforth AJ, Ball SG, Mikala G, Schwartz A, Peers C 1997 Hypoxia inhibits the recombinant alpha 1C subunit of the human cardiac L-type Ca2+ channel. J Physiol 500: 551–556
Fearon IM, Varadi G, Koch S, Isaacsohn I, Ball SG, Peers C 2000 Splice variants reveal the region involved in oxygen sensing by recombinant human L-type Ca(2+) channels. Circ Res 87: 537–539
Yokoyama U, Minamisawa S, Adachi-Akahane S, Akaike T, Naguro I, Funakoshi K, Iwamoto M, Nakagome M, Uemura N, Hori H, Yokota S, Ishikawa Y 2006 Multiple transcripts of Ca2+ channel alpha1-subunits and a novel spliced variant of the alpha1C-subunit in rat ductus arteriosus. Am J Physiol Heart Circ Physiol 290: H1660–H1670
Bhattacharya M, Asselin P, Hardy P, Guerguerian AM, Shichi H, Hou X, Varma DR, Bouayad A, Fouron JC, Clyman RI, Chemtob S 1999 Developmental changes in prostaglandin E(2) receptor subtypes in porcine ductus arteriosus. Possible contribution in altered responsiveness to prostaglandin E(2). Circulation 100: 1751–1756
Clyman RI, Mauray F, Koerper MA, Wiemer F, Heymann MA, Rudolph AM 1978 Formation of prostacyclin (PGI2) by the ductus arteriosus of fetal lambs at different stages of gestation. Prostaglandins 16: 633–642
Coceani F, Kelsey L 1991 Endothelin-1 release from lamb ductus arteriosus: relevance to postnatal closure of the vessel. Can J Physiol Pharmacol 69: 218–221
Coceani F, Liu YA, Seidlitz E, Kelsey L, Kuwaki T, Ackerley C, Yanagisawa M 2000 Deletion of the endothelin-A-receptor suppresses oxygen-induced constriction but not postnatal closure of the ductus arteriosus. J Cardiovasc Pharmacol 36: S75–S77
Fineman JR, Takahashi Y, Roman C, Clyman RI 1998 Endothelin-receptor blockade does not alter closure of the ductus arteriosus. Am J Physiol 275: H1620–H1626
Author information
Authors and Affiliations
Corresponding author
Additional information
ArticlePlus
Click on the links below to access all the ArticlePlus for this article.
Please note that ArticlePlus files may launch a viewer application outside of your web browser.
Rights and permissions
About this article
Cite this article
Thébaud, B., Wu, XC., Kajimoto, H. et al. Developmental Absence of the O2 Sensitivity of L-Type Calcium Channels in Preterm Ductus Arteriosus Smooth Muscle Cells Impairs O2 Constriction Contributing to Patent Ductus Arteriosus. Pediatr Res 63, 176–181 (2008). https://doi.org/10.1203/PDR.0b013e31815ed059
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31815ed059
This article is cited by
-
Understanding the pathobiology in patent ductus arteriosus in prematurity—beyond prostaglandins and oxygen
Pediatric Research (2019)
-
Pharmacological Closure of Patent Ductus Arteriosus: Selecting the Agent and Route of Administration
Pediatric Drugs (2016)
-
Predictors of successful closure of patent ductus arteriosus with indomethacin
Journal of Perinatology (2015)
-
Activation of the EGFR/p38/JNK pathway by mitochondrial-derived hydrogen peroxide contributes to oxygen-induced contraction of ductus arteriosus
Journal of Molecular Medicine (2014)
-
Low-dose thromboxane A2 receptor stimulation promotes closure of the rat ductus arteriosus with minimal adverse effects
Pediatric Research (2012)