Abstract
We hypothesized that the inter-breath variability of the breathing pattern in newborn rats varied with temperature and oxygenation. Breathing pattern was recorded in 4-day-old rats by airflow plethysmography, during normoxia in warm (control) and cold conditions, or during hypoxia (inspired O2 = 10%) in warm or cold conditions, each lasting 15 min. The warm phase (36°C) either preceded or followed the cold (24°C). Time-domain analysis was applied to 500 continuous breaths recorded toward the end of each phase. All parameters describing the breathing pattern (instantaneous ventilation, tidal volume, and inspiratory and expiratory time) had lower variability when the condition differed from control i.e. in cold or hypoxia, with no correlation with the absolute level of ventilation. The difference in variability between warm-normoxia and the other conditions was reduced when cold preceded the warm phase. Gaseous metabolism was increased in cold because of thermogenesis. When the cold preceded the warm phase the increased thermogenesis partly persisted into the warm phase, raising the metabolic level. We conclude that the variability of the breathing pattern in newborn rats 1) does not depend on the absolute level of ventilation, and 2) is reduced by the increased chemical stimuli occurring during cold-hypermetabolism or hypoxia. In normoxia in warm condition metabolic and chemical stimuli are low, and the variability is the highest. The results are in agreement with the clinical observations of a higher incidence of apneic episodes in infants during warm conditions.
Similar content being viewed by others
Main
The breathing pattern during the first postnatal hours is very variable in both frequency and tidal volume, with frequent short apneas, bursts of rapid and shallow respiration alternating with slower and deeper periods, and interruptions of expiration at various lung volumes. These irregularities are well described for the human infant and various analytical methods have been adopted in an attempt to quantify their developmental changes (e.g.,1–4). Irregularities in the breathing pattern have been observed also in newborns of many other mammalian species (5). In newborn rats, breaths with one or more interruptions of expiratory flow due to closure of the glottis are approximately 50% at 10 min after birth, and decrease to ∼4% by the second postnatal day (6). Many parameters contribute to the irregularities of breathing in the neonatal period; among the most important ones are probably the rapidly occurring changes in respiratory mechanics and pulmonary fluid, in blood gases and in chemosensitivity, and the inputs from airway receptors. Changes in oxygenation and temperature, and the associated changes in metabolic level (7), are likely to be an additional source of variability, but their influence has been considered only marginally. Yet, it seems important to assess the role of temperature and oxygenation on breathing irregularities in view of the reports that hypoxia and hyperthermia can be associated with the sudden infant death syndrome (8–10).
In this study we have analyzed the breathing pattern of newborn rats in conditions of normoxia and hypoxia, in combination with cold or warm stimuli. Time-domain analysis has been adopted for quantification of breath-by-breath variability, following criteria similar to those adopted for the analysis of heart rate variability (11, 12). The results have been interpreted taking into account the metabolic changes determined by the variations in temperature and oxygenation.
METHODS
Experiments were performed on newborn Sprague-Dawley rats from nine litters, all at 4 days of age (day 0 = day of birth), either in the morning or afternoon. Experiments were approved by the Animal Ethics Committee of McGill University. The pregnant dams had free access to food and water, and were maintained in individual cages at ambient temperatures between 20 and 25°C, 50–53% relative humidity, 12:12-h dark-light cycle.
The main group of rats (n = 28) was used for measurements of the breathing pattern in normoxia or hypoxia. A separate group of rats (n = 40, from seven litters, studied in sets of four) was used for measurements of gaseous metabolism. Further details on the numbers of animals, or sets of animals in the case of metabolic measurements, used for each experiment are given in the pertinent sections (see “Results”) and in figure legends.
Within each group, rat pups were separated into two main sets, one for measurements in normoxia and the other one in hypoxia. In either case, ambient temperature (Ta) was first set at 32°C, which is slightly below thermo-neutrality for rats of this age (13), and maintained for 15 min. This was followed for half the rat by additional 15 min at 36°C (warm) and 15 min at 24°C (cold), whereas for the remaining half, cold preceded warm. The first phase, at Ta = 32°C, was to provide all the pups with the same “thermal history”; the next two phases, cold and warm in either order, represented the experimental phases.
Breathing pattern.
The animal was placed in the back chamber of a double-chamber airflow plethysmograph, identical to that previously adopted (14, 15). The animal head was emerging into the front-chamber by passing through multiple layers of paraffin sealing film (Parafilm®, Greenwich, CT, U.S.A.) that provided complete separation between the back and front chambers. The back chamber (∼30 mL) was for measuring the airflow (˚V) via a small pneumotachograph (16) connected to a differential pressure transducer (Validyne, Northridge, CA, U.S.A.). Tidal volume (VT) was obtained by electronic integration of the ˚V signal. A steady flow of 80 mL/min, controlled by a flowmeter, was continuously delivered through the anterior chamber, to avoid any accumulation of expired air. This flow consisted of either air, for the normoxic runs (n = 14, body weight 10.1 ± 0.3 g), or hypoxia (n = 14, 10.4 ± 0.2 g), obtained by connecting the anterior chamber to an anesthesia bag filled with a calibrated 10% O2 gas mixture. The two signals (˚V, VT) were recorded on paper (Gould pen recorder) at a speed of 25 mm/s. Ambient temperature was measured in both the front and back chambers by small tungsten-constantan thermocouples (DP30, Omega, Stamford, CT, U.S.A.) and recorded every 2 min.
The pup was placed in the setup with the chambers preset at 32°C by means of a large-size heating lamp. After 15 min, Ta was changed to either 36°C (warm) or 24°C (cold) in alternate order among the pups, respectively by adjusting the distance of the heating source or cooling the animal chamber with ice-wet pads. In either case, Ta reached the desired new value within 5–10 min. The total experimental time was therefore 45 min. Recordings were obtained during the last 5 min of each session (Fig. 1, top panel). At the end, colonic temperature was measured with a very fine thermocouple inserted about 15 mm in the rectum, and its value was taken as representative of body temperature (Tb). The pup was then returned to the dam.
Ambient temperature (Ta) during the experiments for the measurements of breathing pattern (top) or oxygen consumption (bottom). For either measurement, after 15 min at Ta = 32°C, in half of the cases (triangles), Ta was increased to 36°C (warm), and after additional 15 min, it was decreased to 24°C (cold). In the remaining half (circles), the protocol was reversed, with cold preceding warm. The same routine was performed in normoxia (open symbols) and hypoxia (filled symbols). Recordings were obtained during the last 5 min of warm or cold phases (clear boxes). Symbols represent average values of all the experiments, bars indicate 1 SEM.
Gaseous metabolism.
Oxygen consumption (˚VO2) and carbon dioxide production (˚VCO2) were measured with an open flow system, with a set up and a methodology similar to what previously adopted (13, 17). Rat pups were studied in sets of four animals with separators to impede huddling, which influences metabolic rate and is affected by hypoxia (15, 18). The metabolic chamber was preset at Ta = 32°C. After 15 min Ta was changed to warm for 15 min, followed by additional 15 min in cold, for half of the pups, or cold first followed by warm for the remaining half. The same protocols were repeated in normoxia (n = 20, in five sets, individual body weight 9.5 ± 0.1 g) and hypoxia (10% O2) (n = 20, in five sets, 10.1 ± 0.4 g). Gases were passed through a drying column, sampled by appropriate gas analyzers for measuring the O2 and CO2 concentrations, and the values continuously displayed on a computer monitor. ˚VO2 and ˚VCO2 were computed over the last minutes of each phase (Fig. 1, bottom panel), as the product between the inflow-outflow gas concentration difference and the steady gas flow (235 mL/min) delivered through the chamber. Metabolic data are presented normalized by the weight in kilograms, at standard temperature, pressure and dry (STPD) conditions. At the end of the experiment Tb was measured and the pup returned to the dam.
Analysis.
In each pup for each of the two experimental conditions (warm and cold) at least 500 consecutive breaths were analyzed with the help of a graphics tablet connected to a minicomputer. For each breath, tidal volume (VT, mL) and the inspiratory (TI, sec) and expiratory time (TE, sec) were measured. From these parameters instantaneous breathing frequency (f, breaths/min) was computed as [1/(TI+TE)] · 60, and instantaneous ventilation (˚VE, mL/min) as VT·f.
Variability was quantified by use of the analytical approach adopted for time-domain analysis of cardiac inter-beat intervals (11, 12). The simplest quantification of the variability of each of the main parameters describing the breathing pattern (VT, TI, TE, ˚VE) was the calculation of the standard deviation (SD), i.e. the square root of the variance, and the coefficient of variation (CV = SD/mean) of the sequential 500 breaths. The distribution around the mean was quantified with a geometric method based on the construction of a histogram with bins of 1 mL/kg (for VT), 10 ms (TI), 20 ms (TE), and 200 mL·kg−1· min−1 (˚VE); the triangular index (TrIn) corresponds to the total number (500) divided by the number of occurrence at the peak of the histogram. Hence, the larger the TrIn, the flatter the histogram distribution. A further quantification of the degree of dispersion was obtained by measuring the percent of breaths differing from the mean value by more than 30% (DIFF>30%).
We then computed the differences between two adjacent breaths (B-B). This was done by counting the percent of breaths differing from the one immediately preceding by more than a predetermined absolute amount (B-B absolute) or by more than 30% of the overall mean (B-B %mean). These parameters are equivalent to the pSD (percentage of inter-beat interval) and the pNN50 (percentage of adjacent beats differing more than 50 ms) of the classic time domain analysis of heart rate variability. In conclusion, to quantify the inter-breath variability of VT, TI, TE, ˚VE five parameters were used: CV, TrIn, DIFF>30%, B-B absolute, B-B %mean. For any of these parameters, the higher the value, the greater the variability.
Finally, all the five parameters of variability for each rat in each condition were expressed in percent of the mean value in normoxic-warm condition; hence, after this transformation it was possible to average them into a single “variability index.”
Statistical analysis.
Data are presented as group means ± 1 SEM. Statistical analysis was performed by two-way ANOVA to assess the intergroup interactions, one grouping factor being the ambient temperature (warm-cold) and the other the level of oxygenation (normoxia-hypoxia). For the four comparisons of interest (cold-versus-warm in normoxia or hypoxia, normoxia-versus-hypoxia in warm or cold) posthoc analysis was performed with Bonferroni limitations. A significant difference was considered at p < 0.05.
RESULTS
Gaseous metabolism
During normoxia, in the cold ˚VO2 increased by 65%. On the other hand, in hypoxia, as expected (13), the thermogenic effort was absent (Fig. 2).
Oxygen consumption during the warm (36°C) and cold (24°C) conditions in normoxia (n = 14, open symbols) and hypoxia (n = 14, filled symbols). The heavy lines join the average values of all rats, irrespective of the order of warm and cold. The thin lines join the values of the rats, which had either warm first (squares) or cold first (inverted triangles). During normoxia in warm, metabolic rate was higher when it followed the cold phase. Bars indicate 1 SEM.
In hypoxia at 36 or 24°C and in normoxia in the cold ˚VO2 values were very similar whether the cold exposure preceded or followed the warm phase. Differently, in normoxia-warm ˚VO2 varied according to the thermal history. In fact, ˚VO2 was ∼33% higher when the warm phase was preceded by the cold phase (p < 0.005), indicating that the thermogenic effort during cold was not completely abolished by the 15 min in the warm condition.
Body temperature
In normoxia, at the end of the measurements, Tb averaged 36.1 ± 0.2°C and 31.3 ± 0.4°C in the warm and the cold conditions, respectively. Similar values were measured at the end of the hypoxic runs, 35.7 ± 0.2°C (warm) and 31.1 ± 0.2°C (cold).
Breathing Pattern
Average values.
In normoxia during cold ˚VE had only a modest and insignificant change from the warm values; neither VT nor f changed significantly. In hypoxia-warm the pattern was rapid and shallow, and ˚VE averaged ∼20% more than in normoxia. During hypoxia in the cold ˚VE, VT, and f were similar to the normoxic values (Table 1).
Variability.
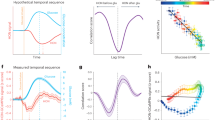
In normoxia the variability index, which is the average of the five parameters used to assess variability, was lower in the cold than in the control (warm) condition. Also in hypoxia-warm the variability index was low compared with control, and not significantly different from hypoxia-cold. These results, which uniformly applied to VT, TI, TE, and ˚VE (Fig. 3), were similarly expressed by all of the five parameters used to quantify variability, individually considered.
Variability index for the four experimental conditions. Data are expressed as percent of the mean value in normoxia-warm. n = 14 rats in normoxia and n = 14 rats in hypoxia. VT = tidal volume. TI = inspiratory time. TE = expiratory time. ˚VE = ventilation. Bars are SEM. *, significant difference from cold. ‡, significant difference from the corresponding condition in hypoxia.
Because of the previously mentioned differences in ˚VO2 during normoxia-warm depending upon the thermal history, the analysis of variability was also performed after separating the animals into the two groups according to their thermal history (Fig. 4). When normoxia-warm followed the cold phase the variability index was less, and not statistically different from that of the cold phase. This result applied to all aspects of the breathing pattern (VT, TI, TE, and ˚VE), and was apparent for each of the five parameters used to express variability.
Variability index for the four experimental conditions, separately considering the results of Fig. 3 according to the sequence of exposures. The bars on each pair of columns indicate that measurements were taken either in cold or warm conditions. The solid bar in the cold studies indicate that a warm phase preceded the cold study, whereas the hatched bar represents a study in the cold with no preceding warm phase. In the warm studies, the hatched bar represents studies in which cold preceded the warm, and the solid bar is a study under warm conditions with no preceding cold phase. Data are expressed as percent of the overall mean value in normoxia-warm, as in Fig. 3. Bars are SEM. *, significant difference from cold. ‡, significant difference from the corresponding condition in hypoxia.
DISCUSSION
The primary finding of this study in newborn rats was that the variability of the breathing pattern was lower in the presence of hypoxia and cold, singly or combined, in comparison to the control (normoxia-warm) condition. Important for the interpretation of the results is that the variability in normoxia-warm condition was reduced when metabolic rate was still high because of the immediately preceding cold exposure.
Methodological Considerations
Protocol.
In the early hours after birth the breathing pattern varies rapidly, both in human infants and animal neonates (2, 19, 20). We have therefore opted to study the animals at day 4, at a time when most of the rapidly changing processes accompanying the adaptation to air breathing have subsided (6). Because in newborn rats maternal behavior is largely responsible for the newborn Tb, the cold or warm experimental phases were in all cases preceded by 15 min at Ta = 32°C, in an attempt to standardize the thermal, and therefore also the metabolic, history of the pups. The duration of the whole experiment was constrained to ∼45 min in order to limit the time that the pup was deprived of maternal care. This implied that the metabolic effect of one phase could still be present throughout the next phase. Indeed to some extent this was the case during warm in normoxia after the cold-induced thermogenesis (Fig. 2). This carry-over effect did not alter the mean results, because the warm-cold sequence alternated among pups; yet, it was useful to appreciate the role of metabolic rate in determining breathing variability, an aspect that will be discussed below.
Assessment of variability.
For the quantification of breathing variability, we opted for the standard time-domain analysis, following criteria, and maintaining the terminology, commonly adopted for the analysis of heart rate variability. On a few occasions frequency-analysis techniques have been applied to the analysis of infant breathing (21, 22); however, unlike the case of heart rate variability (12, 23), for breathing no relationship has been established between spectral frequency ranges and mechanisms of autonomic control. Long-term recordings (i.e. several hours) are not practical in newborns that require frequent maternal care and feeding. In the case of heart rate, long-term recordings in newborns have been found to be less useful than in adults, because the conditions are unstable or “non-stationary”; in these cases, the averaging of long recordings can obscure aspects of autonomic regulation, and therefore have limited physiologic value.
The parameters chosen to quantify the breath-by-breath variability are complementary to each other. Their averaging into one number (“variability index”) much simplifies comparisons and statistical analysis. It should be emphasized that this is not an index of breathing periodicity. In fact, the present analysis applied to patterns characterized by regular waxing and waning of VT or f, as in Cheyne-Stokes respiration, or by periodic clusters, as in Biot respiration (24), would produce high CV and TrIn, and low B-B absolute and B-B %mean, and a rather low variability index.
Average Responses to Hypoxia and Cold
The average metabolic and ventilatory responses to cold and hypoxia were similar to those previously observed in newborn rats (7, 13). Briefly, during cold the increase in ˚VO2 due to nonshivering thermogenesis was not sufficient to maintain Tb, which in newborn rats depends almost exclusively on Ta (13). The increase in ˚VE did not match that of ˚VO2, because during cold the decrease in Tb has an inhibitory effect on ˚VE (25). In hypoxia, cold-induced thermogenesis is depressed; therefore, the ˚VO2 level in cold-hypoxia was determined by the Q10 effect, as it is the case for many other newborn species (7).
During hypoxia, since thermogenesis is depressed, in warm conditions the metabolic level was essentially the same whether or not it was immediately preceded by the cold phase; in fact, eventually, it tended to be slightly lower when preceded by cold (Fig. 2), because of the low Tb. On the contrary, in normoxia-warm ˚VO2 was 33% higher when preceded by cold. This carry-over of the preceding thermogenic effort into the warm phase permitted to separate the rats into two groups according to their thermal history. This separation revealed an association between the level of ˚VO2 in normoxia-warm and the magnitude of breathing pattern variability (Fig. 4).
Breathing Pattern Variability
Numerous studies have quantified the variability of breathing pattern in infants, utilizing from simple statistical approaches to complex analytical techniques (e.g. 1–4, 21, 22). This is the first report aiming to compare inter-breath variability during changes in oxygenation and temperature. The results are unequivocal in indicating that the breathing pattern became more regular during hypoxia and cold-induced thermogenesis, whether singly or in combination.
It was previously reported that in preterm infants during a given sleep state, REM or non-REM sleep, the pattern was more regular when alveolar CO2 increased either spontaneously or because of a small (0.3–1.2%) increase in inspired CO2 (1). In either case ˚VE was higher during the more regular phases, raising the possibility that the lower variability was associated with the hyperpnea. In this study the variability in hypoxia, warm or cold, averaged between ∼40 to ∼70% of normoxia-warm (Fig. 3), with similar mean values of ˚VE, VT, and f. Hence, the ventilatory index did not bear any relationship with the level of ˚VE, nor with any of the other parameters of the breathing pattern.
In warm conditions Ta and Tb were similar between normoxia and hypoxia, whereas the variability index differed greatly; also, during hypoxia, the variability index was similar between the warm and cold phases whereas Ta and Tb differed. Hence, neither Ta nor Tb per se correlated with the magnitude of breathing variability; rather, the effects of temperature on variability depended upon the corresponding changes in metabolic rate. In normoxic lambs breathing irregularities were more frequent when ˚VO2 was lowered by an increase in Ta (26). If not only hypoxia but also hypercapnia reduced breathing variability, as suggested by some results in infants or animal models (1, 27), then the generalization could be made that an increase in chemical drive, including that determined by an increase in metabolism, has the effect of increasing the regularity of the neonatal breathing pattern. The mechanisms potentially involved in lowering the breathing variability with increased chemical drive are speculative. In the case of small amplitude periodic oscillations, it is thought that the gains of the various facilitatory and inhibitory feed-back loops controlling ˚VE are of major importance in determining the extent of the variability (24). An increase in the gain of the chemosensory loops, which in adults is related to ventilatory instability (28), can occur with changes in the state of arousal; however, newborn rats spend most of their sleep time in the REM phase (29). In infants both regular and irregular breathing were occurring within the same sleep state (1), although an increase in Ta and Tb favored the occurrence of apneas mostly during REM sleep (30). At lower temperatures the gain of the ˚VE responses to hypoxia and hypercapnia decreases (7), a phenomenon that probably applies also to newborn rats (15, 17). In addition, in newborn rats the vagal inhibition of pulmonary origin decreases with a decrease in Ta or Tb (17, 31). Hence, based on what is presently known, the combination of two sets of factors, the greater chemical stimuli and the lower gain of the feed-back control loops, seems a likely mechanism for the lower breathing variability in the cold and in hypoxia.
If indeed the level of chemical drive was an important factor in determining the magnitude of breathing variability, it should follow that breathing irregularities would be most apparent when metabolism and chemoreceptor activity are low. In newborns, this combination is a rare eventuality, a part from special cases of hypometabolism during anesthesia or hypothermia. In fact, in newborns hypometabolism commonly occurs during hypoxia, which, however, at the same time activates the chemoreceptors. Conversely, hyperoxia, which silences the peripheral chemoreceptors, in newborns raises metabolic rate (7). On the other hand, in premature, which have low chemosensitivity, hypoxic hypometabolism could be a condition sufficient to enhance breathing variability (32). In healthy newborns an increase in temperature during normoxia could create the conditions for an increase in breathing variability, because in this case both the activity of the chemoreceptors and metabolic rate are low, and the gain of chemosensitivity is high. In such a situation, the passage from wakefulness to sleep could further enhance the variability because of the reduction in metabolism and the lowering in the set point of thermoregulation characteristic of sleep (33).
CONCLUSIONS
The analysis, despite its primarily descriptive nature, has indicated that in the newborn rat inter-breath variability is decreased by hypoxia and cold, singly or in combination. Variability did not correlate with the absolute level of ˚VE. Presumably what is important in determining the degree of breathing variability is the magnitude of the chemical stimuli, including those of metabolic origin. When these were reduced in normoxia-warm conditions, the variability was the greatest. High body or ambient temperature have been observed in some victims of sudden infant death (8, 9), and inhibitory inputs on breathing can become more effective during warm conditions (17, 31). Hence, the notion that breathing variability is enhanced during warm exposure could also be important within the clinical context of the neonatal disturbances in regulation of breathing and apneas.
Abbreviations
- B-B absolute:
-
inter-breath difference >± an absolute amount
- B-B %mean:
-
inter-breath difference >±30% of the overall mean
- CV:
-
coefficient of variation
- DIFF>30%:
-
percent of breaths differing from the mean value >30%
- f:
-
breathing frequency
- REM:
-
rapid eye movement
- Ta:
-
ambient temperature
- Tb:
-
body temperature
- TE:
-
expiratory time
- TI:
-
inspiratory time
- TrIn:
-
triangular index
- ˚V:
-
airflow
- ˚VE:
-
minute ventilation
- VT:
-
tidal volume
- ˚VCO2:
-
gaseous carbon dioxide production
- ˚VO2:
-
gaseous oxygen consumption
References
Rigatto H, Kalapesi Z, Leaky FN, Durand M, Maccallum M, Cates D 1980 Chemical control of respiratory frequency and tidal volume during sleep in preterm infants. Respir Physiol 41: 117–125
Fisher JT, Mortola JP, Smith JB, Fox GS, Weeks S 1982 Respiration in newborns. Am Rev Respir Dis 125: 650–657
Frey U, Silverman M, Barabási AL, Suki B 1998 Irregularities and power law distributions in the breathing pattern in preterm and term infants. J Appl Physiol 85: 789–797
Hodgman JE, Gonzales F, Hoppenbroeuers T, Cabal LA 1990 Apnea, transient episodes of bradycardia, and periodic breathing in preterm infants. Am J Dis Child 144: 54–57
Mortola JP 1984 Breathing pattern in newborns. J Appl Physiol 56: 1533–1540
Mortola JP 1987 Dynamics of breathing in newborn mammals. Physiol Rev 67: 187–243
Mortola JP, Gautier H 1995 Interaction between metabolism and ventilation: effects of respiratory gases and temperature. In: Dempsey JA, Pack AI (eds) Regulation of Breathing. Marcel Dekker, New York, pp 1011–1064
Stanton AN 1984 Overheating and cot death. Lancet 2: 1199–1201
Sawczenko A, Fleming PJ 1996 Thermal stress, sleeping position, and the sudden infant death syndrome. Sleep 19: S267–S270
Poets CF, Meny RG, Chobanian MR, Bonofiglo RE 1999 Gasping and other cardiorespiratory patterns during sudden infant deaths. Pediatr Res 45: 350–354
Kleiger RE, PK Stein, Bosner MS, Rottman JN 1992 Time domain measurements of heart rate variability. Amb Electrocard 10: 487–498
Mortola JP, León-Velarde F, Aguero L, Frappell PB 1999 Heart rate variability in 1-day-old infants born at 4300 m altitude. Cli Sci 96: 147–153
Mortola JP, Dotta A 1992 Effects of hypoxia and ambient temperature on gaseous metabolism of newborn rats. Am J Physiol 263: R267–R272
Saetta M, Mortola JP 1985 Breathing pattern and CO2 response in newborn rats before and during anesthesia. J Appl Physiol 58: 1988–1996
Saiki C, Mortola JP 1996 Effect of CO2 on the metabolic and ventilatory responses to ambient temperature in conscious adult and newborn rats. J Physiol Lond 491: 261–269
Mortola JP, Noworaj A 1983 Two-sidearm tracheal cannula for respiratory airflow measurements in small animals. J Appl Physiol 55: 250–253
Merazzi D, Mortola JP 1999 Effects of changes in ambient temperature on the Hering-Breuer reflex of the conscious newborn rat. Pediatr Res 45: 370–376
Mortola JP, Feher C 1998 Hypoxia inhibits cold-induced huddling in rat pups. Respir Physiol 113: 213–222
Davey MG, Johns DP, Harding R 1998 Postnatal development of respiratory function in lambs studied serially between birth and 8 wk. Respir Physiol 113: 83–93
Mortola JP, Fisher JT, Smith JB, Fox GS, Weeks S, Willis D 1982 Onset of respiration in infants delivered by cesarean section. J Appl Physiol 52: 716–724
Hathorn MKS 1974 The rate and depth of breathing in new-born infants in different sleep states. J Physiol London 243: 101–113
Waggener TB, Frantz ID III, Stark AR, Kronauer RE 1982 Oscillatory breathing patterns leading to apneic spells in infants. J Appl Physiol 52: 1288–1295
Öri Z, Monir G, Weiss J, Sayhouni X, Singer DH 1992 Heart rate variability. Amb Electrocard 10: 499–537
Khoo MCK 1997 Periodic breathing. In Crystal RG, West JB, Barnes PJ, Weibel ER (eds) The Lung: Scientific Foundations. Lippincott-Raven Publishers, Philadelphia, pp 1851–1863
Gautier H 1996 Interactions among metabolic rate, hypoxia, and control of breathing. J Appl Physiol 81: 521–527
Andrews DC, Symonds ME, Johnson P 1991 The interaction of the upper airway and thermometabolism on respiratory rhythm during non-REM sleep in the developing lamb. J Dev Physiol 16: 37–43
Canet E, Praud J-P, Bureau MA 1997 Periodic breathing induced on demand in awake newborn lamb. J Appl Physiol 82: 607–612
Dunai J, Kleiman J, Trinder J 1999 Ventilatory instability during sleep onset in individuals with high peripheral chemosensitivity. J Appl Physiol 87: 661–672
Jouvet-Mounier D, Astic L, Lacote D 1970 Ontogenesis of the states of sleep in rat, cat and guinea pig during the first postnatal month. Dev Psychobiol 2: 216–239
Berterottière D, D'Allest AM, Dehan M, Gaultier C 1990 Effects of increase in body temperature on the breathing pattern in premature infants. J Dev Physiol 13: 303–308
Merazzi D, Mortola JP 1999 Hering-Breuer reflex in conscious newborn rats: effects of changes in ambient temperature during hypoxia. J Appl Physiol 87: 1656–1661
Rigatto H, Brady JP 1972 Periodic breathing and apnea in preterm infants. Pediatrics 50: 219–228
Parmeggiani PL 1990 Thermoregulation during sleep in mammals. News Physiol Sci 5: 208–212
Author information
Authors and Affiliations
Additional information
The study was supported by funds from the Medical Research Council of Canada. D.M. stage at McGill University was financially supported by a bursary in Neonatology from the Fondo J. Migliorina, Varese, Italy.
Rights and permissions
About this article
Cite this article
Cameron, Y., Merazzi, D. & Mortola, J. Variability of the Breathing Pattern in Newborn Rats: Effects of Ambient Temperature in Normoxia or Hypoxia. Pediatr Res 47, 813–818 (2000). https://doi.org/10.1203/00006450-200006000-00022
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200006000-00022
This article is cited by
-
Diaphragmatic activity and neural breathing variability during a 5-min endotracheal continuous positive airway pressure trial in extremely preterm infants
Pediatric Research (2021)
-
Disharmony between wake- and respiration-promoting activities: effects of modafinil on ventilatory control in rodents
Respiratory Research (2016)
-
Thermogenesis, vocalization, and temperature preference of 1-day-old chicken hatchlings after cold-exposure in late embryogenesis
Journal of Comparative Physiology B (2014)
-
Experimental febrile seizures are precipitated by a hyperthermia-induced respiratory alkalosis
Nature Medicine (2006)