Abstract
To determine if alterations in arterial pressure influenced fetal heart rate variability (HRV), experiments were carried out in chronically catheterized fetal sheep aged 128–138 d. Arterial pressure was raised or lowered by intravenous infusion of phenylephrine or sodium nitroprusside, and the effects on heart rate (HR) and HRV were measured (HRV, as the coefficient of variation (CV) in mean pulse interval or by power spectral analysis). Experiments were carried out before and during β-adrenoceptor blockade with propranolol or before and during cardiac vagal blockade with atropine. There were positive relationships between mean arterial pressure and HRV (slope = 0.074 ± 0.001, r = 0.81 ± 0.06, p < 0.001, measured as the CV of pulse interval) and between mean arterial pressure and power spectral density (slope = 4 ± 0.5, r = 0.89 ± 0.02, p < 0.001) in the frequency range 0.04–0.08 Hz. β-adrenoceptor blockade had no effect on these relationships, but they were abolished by cardiac vagal blockade. The sigmoid relationship between fetal HR and mean arterial pressure, i.e. the cardiac baroreflex, was affected, however, by blockade of cardiac sympathetics and abolished by blockade of cardiac vagal activity. Thus, fetal HRV was affected by alterations in arterial pressure, and these effects depended on the integrity of the cardiac vagus, not on alterations in cardiac sympathetic activity. Therefore, although baroreflex control of fetal HR depends on the integrity of both sympathetic and parasympathetic efferent pathways, baroreceptor-induced changes in HRV depend only on the cardiac vagus.
Similar content being viewed by others
Main
Variability in fetal HR is widely used to monitor fetal well-being; low levels of variability or loss of accelerations in either fetal or newborn HR are of clinical concern (1).
The major physiologic determinants of fetal HRV are fetal movements and breathing (2). Chemoreflexes also modulate fetal HRV. Itskovitz et al. (3) showed that chemodenervated fetal sheep had more HRV than normal animals. By contrast, we (4) and others (2) showed that acute hypoxia was associated with an increase in fetal HRV. Because this increase in fetal HRV during hypoxia was not affected by β-adrenoceptor blockade with propranolol but was abolished by treatment with the muscarinic antagonist atropine, Yu et al. (4) concluded that the increase in HRV associated with acute hypoxia depended on the integrity of efferent cardiac vagal pathways.
As far as we know, the degree to which the arterial baroreflex affects fetal HRV has not been quantified; nor is it known whether any possible effects are mediated via the cardiac sympathetics, the vagus, or both.
Recently, we have shown that in adult sheep there is a V-shaped relationship between HRV [measured either as the coefficient of variation (CV) in mean PI or by power spectral analysis] and MAP (5). The negative or downward slope of this relationship was not present in animals treated with propranolol, and the positive or upward slope was abolished when the animals were treated with atropine. Thus, arterial pressure affected HRV in the adult sheep, and both the cardiac sympathetic nerves and the vagus were necessary efferent pathways for these effects of arterial pressure on HRV. The two slopes of the limbs of the V provided a measure of the degree to which each of these two efferent pathways of the baroreflex mediated HRV (5).
To see if fetal HRV was also influenced by the arterial baroreflex and to determine the efferent pathways via which any such effects might be mediated, we carried out experiments in chronically catheterized fetal sheep in which arterial pressure was raised and lowered using phenylephrine and sodium nitroprusside, respectively. These drugs have been widely used for many years to study the cardiac baroreflex in both fetal (6, 7) and adult animals (6, 8) and human beings (9). Any effect of arterial pressure on fetal HRV was compared with its effects on mean fetal HR.
To determine the roles of the cardiac vagus and sympathetic nerves in mediating reflex changes in fetal HR and HRV, we studied animals before and after treatment with either atropine or propranolol.
METHODS
Experiments were approved by the Animal Care and Ethics Committee, University of New South Wales. Fourteen chronically catheterized fetuses were studied. Surgery was carried out between 120–125 d; fetuses were 128–138 d old (term = 150 d) when experiments were begun.
Surgical preparation.
Surgery was performed after the ewes had fasted for 16 h. Ewes were anesthetized with sodium thiopentone 1.5 g i.v. (Pentothal; Abbott, Kurnell, NSW, Australia) and maintained with 2–3% halothane (Fluothane; ICI, Macclesfield, Cheshire, UK) in oxygen. Under aseptic conditions, polyvinyl catheters (inner diameter, 1.0 mm; outer diameter, 1.5 mm; length, 100 cm) filled with heparinized saline (100 U/mL; Baxter Health Care Pty. Ltd., NSW, Australia) were inserted into a fetal femoral artery and both tarsal veins. Another catheter was placed in the amniotic cavity to measure intraamniotic pressure, and 600 mg of procaine penicillin and 750 mg of dihydrostreptomycin sulfate (Hydropen, Bomac Laboratories, Asquith, NSW, Australia) were injected into the amniotic cavity. Polyvinyl catheters (inner diameter, 1.5 mm; outer diameter, 2.7 mm) were inserted into a maternal femoral artery and vein (10). At the end of surgery, 600 mg of procaine penicillin and 750 mg of dihydrostreptomycin sulfate were given intramuscularly to the ewe. For the next 2 d after surgery, these antibiotics were given via the amniotic catheter. All arterial and venous catheters were flushed with heparinized saline (100 U/mL) daily. Ewes were housed in metabolic cages, and the ambient temperature was 18–23°C. They were given free access to water, lucerne chaff, and oats. Daily fluid and food intake and urine output were measured. No experiments were performed until at least 7 d after surgery.
Experimental protocol.
Maternal and fetal arterial pressures and intraamniotic pressure were recorded using Utah Medical disposable transducers connected to Neomedix preamplifiers (Neomedix Systems, Sydney, NSW, Australia) and a Yokogama ORP 1200 eight-channel recorder (Tech-Fast, Sydney, NSW, Australia). At appropriate times, 100-s records were logged using an IBM-compatible PC (486) and a Metrabyte DAS16 card (Keithley, MA). The sampling rate was 400 Hz.
After a 30-min control period, arterial pressure was raised or lowered by stepwise intravenous infusions of phenylephrine (Neosynephrine, Winthrop) at rates of 0.04–0.1 mg/min or by intravenous infusions of sodium nitroprusside (Mulgrave, Victoria, Australia) at rates of 16–46 μg/min. These drugs have been used in many studies in adult animals (6, 8) and in human beings (9) as well as in fetal sheep (6, 7) to characterize the cardiac baroreflex. In each fetus, seven to 10 100-s records of the different levels of arterial pressure were obtained. Arterial pressure was maintained for 3–5 min at each level, and records were taken during the last 100 s when arterial pressure was steady. Fetal arterial blood samples (3 mL) were collected before and 10 min after arterial pressure was raised to its highest level and 10 min after it was reduced to its lowest level. To assure that each 100-s sample was not contaminated by resetting, we waited 2–3 min after the arterial pressure had stabilized before collecting it. Although this may mean there was some resetting of the baroreceptors (11), it prevented any problems caused by rapid resetting occurring during collection of data. Arterial blood gases and pH were measured at 37°C and corrected to 39.5°C by using a CIBA-Corning blood gas system (model 288; Medfield, MA).
After a 2-h recovery period, the experiment was repeated either during cardiac vagal blockade or during β-adrenoceptor blockade. These treatments were randomized and were not carried out on the same day. Cardiac vagal blockade was achieved by giving atropine sulfate (Astra Pharmaceuticals, Sydney, NSW, Australia). Fourteen fetuses were given an intravenous injection of 2.4 mg atropine sulfate 10 min before an experiment, followed by continuous infusion of atropine sulfate at 4.8 mg/h and an injection of 1.2 mg of atropine sulfate before each record. Propranolol (Inderal, ICI, Australia Operations Pty Ltd.) was used to induce β-adrenoceptor blockade. Seven fetuses were given an intravenous injection of 2 mg of propranolol 10 min before an experiment, followed by an infusion of 4 mg/h. These doses of atropine and propranolol have been shown to block cardiac vagal and cardiac sympathetic activity, respectively, in fetal and adult sheep (6) and have been used in a number of studies of the cardiac baroreflex of adult animals (8), human beings (12), and fetal sheep (13) to characterize the cardiac baroreflex. Parasympathetic and sympathetic blockade was performed on different days, allowing 24 h between each experiment.
At the end of an experiment, ewes were killed by intravenous injection of 20 mL of pentobarbital sodium (325 mg/mL; Lethabarb, Virbac, Australia).
Analysis of data.
PI was calculated from the time between each maximum of the arterial pressure wave. A peak picking method was used to derive PI from the arterial pressure record. From each 100-s record, the mean PI and its SD were calculated. Because the SD is dependent on the magnitude of the mean (14), the CV (%) of mean PI was calculated and used as an index of the HRV that occurred over the 100-s period. Fetal HR was determined from the mean PI.
The relationship between MAP and HR was analyzed by a logistic sigmoid function (GraphPad Inplot, GraphPad Software, San Diego, CA) using the following equation (15):MATH where A(1) is the range of HR [beats per minute (bpm)], A(2) is the slope or sensitivity of the relationship (1/mm Hg), A(3) is the midpoint in mm Hg (i.e. the point from which equal pressor and depressor responses can occur), and A(4) is the minimal HR. Derivations of this equation (11) use MAP rather than systolic pressure to determine the relationship between arterial pressure and HR.

The gain of the baroreflex was calculated from the first derivative of the equation (15); the threshold pressure (the lowest pressure that produces a significant decline in HR) and the saturation pressure (the pressure necessary to achieve maximal inhibition of HR) were calculated from the solution of the third derivative of the equation (15).
Each 100-s record of beat-to-beat intervals was interpolated into an 8192-point wave suitable for fast Fourier transform and determination of HRV in the frequency domain. In a previous study, we have shown that the same spectra are obtained in adult and fetal sheep when beat-to-beat intervals are used as when R-R intervals (from the ECG) are used (4). A rectangular window was used for calculating the power spectrum. Results were exported to an Excel spreadsheet for further analysis. PSD was expressed in arbitrary units.
To relate our data to data obtained in fetal sheep (13) and human infants (16), each spectrum was divided into the following six frequency ranges; LLF (0.04–0.08 Hz), LF (0.08–0.15 Hz), HF1 (0.16–0.45 Hz), HF2 (0.46–0.6 Hz), HF3 (0.61–0.9 Hz), and HF (0.91–1.3 Hz). In adult sheep, we describe only three ranges; two are the same as LLF and LF in fetal sheep, and the third corresponds to respiratory frequency, which is not consistently available in fetuses (5).
In each frequency range (in each experiment), there were a similar number of points in the power spectrum, i.e. the following number of samples was collected: in LLF 4 ± 1, in LF 7 ± 1, in HF1 26 ± 2, in HF2 13 ± 1, in HF3 26 ± 2, and in HF 35 ± 2. The power in each range was the sum of these samples. Total power was the sum of the power in all ranges.
Statistical analysis.
Paired t test was used to compare differences before and after vagal blockade or differences before and after sympathetic blockade. The relationships between HRV and MAP and between PSD and MAP were determined by linear regression analysis (14) using the SPSS statistical package (SPSS/PC; SPSS, Inc.; Chicago, IL). Slopes of the relationships between MAP and PSD (in the frequency ranges LLF, LF, HF1, and HF2) were compared using ANOVA. If a difference was found (p < 0.05), the Newman-Keuls test was used to determine which means were different. Values are expressed as mean ± SEM.
RESULTS
Neither changes in arterial pressure nor treatment with atropine or propranolol affected blood gases or pH (Table 1). To prevent any confounding effects of residual actions of pharmacologic blockade on mean HR and HRV, no experiments using pharmacologic blockade were carried out within a 24-h period of each other.
The relationship between mean fetal HR and MAP.
Figure 1A shows the sigmoid relationship between MAP and mean fetal HR (averaged over 100 s) by use of data obtained from 14 fetal sheep. The gain was −3.1 ± 0.5 bpm/mm Hg. The maximal HR of 197 ± 6 bpm was obtained when MAP was 46 ± 1 mm Hg (threshold pressure), and the minimal HR of 121 ± 3 bpm was obtained when MAP was 72 ± 1 mm Hg (saturation pressure). Thus, the operating range was 25 ± 1 mm Hg. The midpoint pressure was 59 ± 1 mm Hg.
In seven fetal sheep, the effects of β-adrenoceptor blockade were studied. The gain of the baroreflex was slightly increased. The mean was −3.0 ± 0.4 bpm/mm Hg before and −3.5 ± 0.5 bpm/mm Hg during β-adrenoceptor blockade (p < 0.05, Fig. 1B). The maximal HR was reduced from 196 ± 9 to 131 ± 6 bpm (p < 0.01), and the minimal HR was lowered from 118 ± 2 to 96 ± 7 bpm (p < 0.05). Threshold pressure increased from 47 ± 2 to 57 ± 1 mm Hg (p < 0.01), and midpoint pressure increased from 60 ± 2 to 66 ± 2 mm Hg (p < 0.01). Saturation pressure did not change. Thus, the operating range decreased from 25 ± 1 to 14 ± 2 mm Hg (p < 0.01). In all 14 fetal sheep, the relationship between MAP and HR was abolished by atropine (Fig. 1C).
The relationship between HRV and MAP.
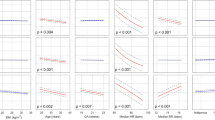
Linear regression analysis was used to determine the relationship between HRV (measured as the CV of mean PI) and MAP (Fig. 2). In all 14 fetuses, there was a positive relationship between HRV and MAP (slope = 0.074 ± 0.001, r = 0.81 ± 0.06, p < 0.001, n = 14, Fig. 2A).
The mean slopes of the relationships between MAP (mm Hg) and HRV (measured as the CV in PI, %) (A) before (n = 14, slope = 0.074 ± 0.001, r = 0.81 ± 0.06, p < 0.001) and (B) during β-adrenoceptor blockade (n = 7, slope = 0.073 ± 0.002, r = 0.91 ± 0.07, p < 0.001) and (C) during cardiac vagal blockade (n = 14). Values are mean ± SEM. SI unit conversion, 1 mm Hg = 0.1333 kPa.
In seven fetal sheep, β-adrenoceptor blockade had no effect on the relationship between HRV (measured as CV of mean PI) and MAP (Table 2 and Fig. 2B). In all 14 fetal sheep, the relationship between HRV and MAP was abolished during treatment with atropine (Fig. 2C).
The relationship between PSD and MAP.
Figure 3 shows PSD (expressed in arbitrary units) in one fetus measured at different arterial pressures. The higher the level of arterial pressure the greater the power in all ranges studied (Fig. 3 and Table 3). However, the increase in power was most evident in the lower ranges, being more than 7-fold in LLF (Table 3). Therefore, the relationship between power in LLF and MAP is described and is shown in Figure 4. In LLF, there was a positive relationship between MAP and PSD (slope = 4.0 ± 0.5, r = 0.89 ± 0.02, p < 0.001, n = 14;Fig. 4A and Table 4). Similar but weaker relationships between power in LF, HF1, HF2, and MAP were also found (Table 4), and the effects of pharmacologic blockade on these relationships were the same as those that are described below for the relationship between LLF and MAP.
The mean slopes of the relationships between PSD (expressed in arbitrary units) measured over the frequency range 0.04–0.08 Hz and MAP (mm Hg) (A) before (n = 14, slope = 4.0 ± 0.5, r = 0.89 ± 0.02, p < 0.001) and (B) during β-adrenoceptor blockade (n = 7, slope = 2.8 ± 0.8, r = 0.93 ± 0.06, p < 0.001) and (C) during cardiac vagal blockade (n = 14). Values are mean ± SEM. SI unit conversion, 1 mm Hg = 0.1333 kPa.
During β-adrenoceptor blockade, the positive relationship between HRV and PSD was still present (slope = 2.8 ± 0.8, r = 0.93 ± 0.06, p < 0.001, n = 7;Table 4 and Fig. 4B), but it was absent during vagal blockade (Fig. 4C).
DISCUSSION
In the present study in fetal sheep and in our previous study in adult nonpregnant and pregnant ewes (5, 6), we used phenylephrine to raise arterial pressure and sodium nitroprusside to lower it. Both drugs have been used for many years to study baroreflex-mediated changes in HR in human beings (9) and in animals (8). We and others (7) have also used phenylephrine and sodium nitroprusside to study the cardiac baroreflex in chronically catheterized fetal sheep, and both drugs have been used to study the baroreceptor-mediated changes in HR and RSNA (17, 18). Although pharmacologic studies have suggested that both phenylephrine and sodium nitroprusside can affect the activity of intrinsic cardiac neurons, studies in denervated animals show that these effects, if they occur in vivo, are so slight that their administration after baroreceptor denervation has no significant effect on HR (19).
In studying the effect of arterial pressure on mean HR, we chose to examine the HR-MAP relationship rather than the relationship between MAP and PI. This was because the MAP-PI relationship overemphasizes changes occurring at the bradycardic end of the curve where the cardiac vagus is dominant and underemphasizes changes at the tachycardic end where the cardiac sympathetics are dominant (11). MAP-HR curves measure each end of the curve equally. This is an advantage when partitioning responses between vagal and sympathetic components (11). Using this method, we could show that β-adrenoceptor blockade reduced the maximal achievable HR and the operating range but had no effect on the gain. This could be because the effects of the cardiac sympathetics on HR are attenuated when vagal tone is high (20). There is no doubt that the level of efferent vagal tone was different at different levels of arterial pressure because treatment with atropine abolished the sigmoid relationship between HR and MAP (Fig. 1C).
We chose to measure the effects of arterial pressure on HR and HRV by collecting 100-s records of arterial pressure 2–3 min after arterial pressure had stabilized at a given level. This may have meant that some resetting of the arterial baroreceptors occurred. Korner (11) concluded that resetting or adaptation began within 30 s of a change in pressure. We needed to collect 100-s records when arterial pressure was stable, and we wanted to be sure that any responses mediated by changes in efferent sympathetic tone had affected HR. Therefore, we deliberately chose to take our measurements at a later time. Because all our measurements were made at the same time, we feel that we can confidently describe effects of the arterial baroreceptors on fetal HRV and the autonomic pathways mediating these actions.
The major finding in the present study is that there was a positive relationship between fetal HRV and MAP. To our knowledge, this observation has not been made previously. We showed that the relationship between HRV and MAP was present when HRV was determined in both time and frequency domains (Figs. 2 and 4). The effects on HRV (measured using power spectral analysis) were most marked in the LLF range (0.04–0.08 Hz). We have previously shown that this frequency range is influenced by both vagal and sympathetic tone (5).
Our second major finding was that the relationship between HRV and MAP depended on the integrity of the efferent cardiac vagus (Figs. 2 and 4). There was no effect of β-adrenoceptor blockade on this relationship (Table 2). It could be argued as above that the simultaneous changes in vagal activity masked the effects of alterations in cardiac sympathetic activity (20). This is unlikely because in adult sheep we were able to show that the arterial baroreceptors modified HRV through both vagal and sympathetic efferent pathways (5). The striking V-shaped relationship between HRV and MAP in chronically catheterized adult pregnant and nonpregnant ewes was not seen in the fetus. In the fetus, only a positive or upward slope was found. Because the negative or downward slope of the V-shaped relationship between HRV and MAP was abolished in adult sheep by β-adrenoceptor blockade, we concluded that it reflected the degree to which cardiac sympathetic activity modulated HRV in response to altered baroreceptor input. This means that in the fetus there is no evidence that HRV is modulated by baroreceptor-mediated changes in cardiac sympathetic tone.
The only recordings of efferent sympathetic nerve activity that have been made in fetal sheep have been recordings from RSNA (18). Although it may be dangerous to extrapolate from these data to fetal cardiac sympathetics, it is worth mentioning that resting renal sympathetic tone is low in fetal sheep. It is, however, modulated by the arterial baroreceptors in a pattern similar to their modulation of fetal HR (18). If, like the renal sympathetics, efferent cardiac sympathetic tone is also low, it is possible that any effects of altered sympathetic tone on fetal HRV could be masked by the more dominant changes in efferent cardiac vagal tone (20). It is also possible that cardiac sympathetic nerve activity increases with birth, as does RSNA (21). If this were the case, then, within hours of delivery, the single direct relationship that exists between HRV and MAP in fetal life might be replaced by the V-shaped relationship seen in adult sheep.
In conclusion, it has been known for a long time that the major factors affecting fetal HRV are fetal movements and breathing. As well, it is influenced by chemoreflexes. Now we have shown that it is also modulated by the arterial baroreflex, the effects of which depend on the integrity of the fetal cardiac vagus. The degree to which baroreceptor-mediated changes in efferent cardiac vagal activity affect HRV can be measured as the slope of the relationship between fetal MAP and HRV.
Abbreviations
- HR:
-
heart rate
- MAP:
-
mean arterial pressure
- HRV:
-
heart rate variability
- PI:
-
pulse interval
- PSD:
-
power spectral density
- RSNA:
-
renal sympathetic nerve activity
- LLF:
-
low low frequency (0.04–0.08 Hz)
- LF:
-
low frequency (0.08–0.15 Hz)
- HF1:
-
high frequency 1 (0.16–0.45 Hz)
- HF2:
-
high frequency 2 (0.46–0.6 Hz)
- HF3:
-
high frequency 3 (0.61–0.9 Hz)
- HF:
-
high frequency (0.91–1.3 Hz)
References
Hanson MA, Spencer JAD, Rodeck CH 1993 Fetus and Neonate Physiology and Clinical Applications. Vol I. The Circulation. Cambridge University Press, Cambridge
Dalton KJ, Dawes GS, Patrick JE 1977 Diurnal, respiratory, and other rhythms of fetal heart rate in lambs. Am J Obstet Gynecol 127: 414–424
Itskovitz J, LaGamma EF, Rudolph AM 1983 Baroreflex control of the circulation in chronically instrumented fetal lambs. Circ Res 52: 589–596
Yu ZY, Lumbers ER, Gibson KJ, Stevens AD 1998 Effects of hypoxaemia on fetal heart rate, variability, and cardiac rhythm. Clin Exp Pharmacol Physiol 25: 577–584
Lumbers ER, Yu ZY 1999 A method for determining baroreflex-mediated sympathetic and parasympathetic control of the heart in pregnant and non-pregnant sheep. J Physiol 512: 555–566
Ismay MJ, Lumbers ER, Stevens AD 1979 The action of angiotensin II on the baroreflex response of the conscious ewe and the conscious foetus. J Physiol 288: 467–479
Nuyt AM, Segar JL, Holley AT, O'Mara MS, Chapleau MW, Robillard JE 1996 Arginine vasopressin modulation of arterial baroreflex responses in fetal and newborn sheep. Am J Physiol 271: R1643–R1653
Schuessler RB, Canavan TE, Boineau JP, Cox JL 1988 Baroreflex modulation of heart rate and initiation of arterial activation in dogs. Am J Physiol 255: H503–H513
Fritsch JM, Rea RF, Eckberg DL 1989 Carotid baroreflex resetting during drug-induced arterial pressure changes in humans. Am J Physiol 256: R549–R553
Lumbers ER, Stevens AD 1983 Changes in fetal renal function in response to infusions of a hyperosmotic solution of mannitol to the ewe. J Physiol 343: 439–446
Korner PI 1989 Baroreceptor resetting and other determinants of baroreflex properties in hypertension. Clin Exp Pharmacol Physiol 15: 45–64
Fagius J, Sundlof G, Wallin BG 1987 Variation of sympathetic reflex latency in man. J Auton Nerv Syst 21: 157–165
Metsälä T, Siimes A, Välimäki I 1995 The effect of change in sympatho-vagal balance on heart rate and blood pressure variability in the foetal lamb. Acta Physiol Scand 154: 85–92
Zar JH 1984 Biostatistical Analysis, 2nd Ed. Prentice-Hall, Englewood Cliffs, NJ, pp 162–205
Kent BB, Drane JW, Blumenstein B, Manning JW 1972 A mathematical model to assess changes in the baroreceptor reflex. Cardiology 57: 295–310
Chatow U, Davidson S, Reichman BL, Akselrod S 1995 Development and maturation of the autonomic nervous system in premature and full-term infants using spectral analysis of heart rate fluctuations. Pediatr Res 37: 294–302
Robillard JE, Nakamura KT, Wilkin MK, McWeeny OJ, Dibona GF 1987 Ontogeny of the renal hemodynamic response to renal nerve stimulation in sheep. Am J Physiol 252: F605–F612
Segar JL, Hajduczok G, Smith BA, Merrill DC, Robillard JE 1992 Ontogeny of baroreflex control of renal sympathetic nerve activity and heart rate. Am J Physiol 263: H1819–H1826
Yardley RW, Bowes G, Wilkinson M, Cannata JP, Maloney JE, Ritchie BC, Walker AM 1983 Increased arterial pressure variability after arterial baroreceptor denervation in fetal lambs. Circ Res 52: 580–588
Levy MN, Zieske H 1969 Autonomic control of cardiac pacemaker activity and atrioventricular transmission. J Appl Physiol 27: 465–470
Segar JL, Mazursky JE, Robillard JE 1994 Changes in ovine renal sympathetic nerve activity and baroreflex function at birth. Am J Physiol 267: H1824–H1832
Acknowledgements
The authors thank Dr. K.J. Gibson, Dr. A.D. Stevens, and P. Bode for their assistance and E. Crawford for his development of computer software.
Author information
Authors and Affiliations
Additional information
Supported by the NHMRC (Australia). Z.Y.Y. was supported by a CRC for Biopharmaceutical Research Pty. Ltd. Postgraduate Scholarship.
Rights and permissions
About this article
Cite this article
Yu, ZY., Lumbers, E. Measurement of Baroreceptor-Mediated Effects on Heart Rate Variability in Fetal Sheep. Pediatr Res 47, 233 (2000). https://doi.org/10.1203/00006450-200002000-00014
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200002000-00014
This article is cited by
-
Continuous measurement of cardiac output with the electrical velocimetry method in patients under spinal anesthesia for cesarean delivery
Journal of Clinical Monitoring and Computing (2015)
-
Development of baroreflex and endocrine responses to hypotensive stress in newborn foals and lambs
Pflügers Archiv - European Journal of Physiology (2005)