Abstract
Changes in body composition, in particular the onset of obesity, may result from reductions in total daily energy expenditure (TDEE) as a consequence of relative physical inactivity. Children previously treated for acute lymphoblastic leukemia (ALL) become obese, yet the mechanism remains undefined. TDEE and physical activity levels [PAL = TDEE/basal metabolic rate(BMR)] were measured in 34 long-term survivors of ALL and compared with results from 21 survivors of other malignancies and 32 healthy sibling control subjects using the flex-heart rate technique. Body composition was measured by dual energy x-ray absorptiometry. The median TDEE was reduced in the ALL group(150 kJ·kg d-1) compared with other malignancies and controls(207 and 185 kJ·kg d-1, respectively, p < 0.01). This reduction was accounted for mainly by a relative decrease in the PAL of the ALL group (1.24) compared with both other malignancies and controls (1.58 and 1.47, respectively, p < 0.01). TDEE and PAL were correlated with percentage body fat (r = -0.39, p < 0.001 and r = -0.24, p < 0.05, respectively). Obesity in survivors of ALL may, in part, be explained by a reduction in TDEE as a consequence of reduced PAL. The cause of such reduction is uncertain.
Similar content being viewed by others
Main
Improved survival after treatment for malignancy in childhood has led to increasing emphasis being placed on long-term quality of life(1). Obesity has been recognized as a late effect after therapy for ALL in childhood(2–5), but the mechanisms involved are unknown. Physical activity has not only an important role in the regulation of body mass and composition(6), but also has an influence on psychologic health and well being in children(7). Abnormalities of energy expenditure, possibly as a result of physical inactivity, may predispose to obesity. The aim of this study was to measure the free living TDEE and patterns of physical activity in a group of survivors of childhood malignancy and compare it with a group of healthy control subjects. Relationships of these variables with alterations in body composition were also evaluated. Previous research has suggested that the onset of obesity may result from previous cranial irradiation(2), hence the division of the survivors into two groups,1) children treated for ALL who had received cranial irradiation and chemotherapy and 2) children treated for other malignancies who had received chemotherapy alone.
METHODS
Subjects. Measurements were performed on a total of 88 children of whom 56 were long-term survivors of childhood malignancy with a median(range) age of 10.4 (7.2, 18.4) y, at least 1.5 y from cessation of therapy, and were in continuous first remission. Thirty-five of these children (14 boys) had received treatment for ALL including chemotherapy and prophylactic cranial irradiation (≤18 Gy, n = 30, and 24 Gy, n = 5), and 21 children (11 boys) were a heterogeneous group who had received chemotherapy for a variety of tumors but had not received cranial or any other radiotherapy. Children with ALL had been treated according to the Medical Research Council, United Kingdom ALL (UKALL) protocols VI (n = 2), VIII (n = 8)(8), or X (n = 24)(9). One child in the ALL group had received treatment for NHL but was included in this group because he had received cranial irradiation(17.2 Gy). Each treatment regimen consisted of a period of induction to induce remission followed by cranial irradiation and maintenance chemotherapy for 2 or 3 y. The later protocols included further blocks of more intensive chemotherapy. Children treated for ALL received variable doses of anthracycline therapy (UKALL X, 90-270 mg/m2; UKALL VIII, 0-90 mg/m2; UKALL VI, no anthracycline; and NHL, 330 mg/m2).
The 21 children who comprised the group treated for other malignancies had been treated for acute myeloid leukemia (n = 7), NHL (n = 2), Wilms' tumor (n = 6), neuroblastoma (n = 2), yolk sac tumor (n = 2), rhabdomyosarcoma (n = 1), and Hodgkin's lymphoma (n = 1). Children treated for either acute myeloid leukemia or NHL had received anthracycline therapy at a dosage of 270-450 mg/m2.
The major differences in therapy between the two groups were cranial irradiation and the more prolonged and continuous nature of chemotherapy in children treated for ALL and also the use of oral corticosteroids. The remaining 32 (18 boys) children were siblings of the survivors invited to participate as healthy control subjects. Where there was a choice of more than one sibling within the appropriate age range, the one closest in age to the index case was chosen. The study was approved by the ethics committee for South Glamorgan, and written parental consent was obtained for each child.
Total daily energy expenditure. The estimation of daily energy expenditure was made by making measurements of BMR (kJ/min) and RMR (kJ/min). BMR is the minimum rate of energy expenditure in an awake, relaxed person lying supine in a thermoneutral environment and in the fasted state(10). It comprises the sleeping metabolic rate and the energy cost of arousal. RMR includes BMR and the energy costs attributed to the thermic effect of food and the state of unrelaxed rest. Energy expended during physical activity was measured from minute by minute daytime ambulatory HR recording after individual calibration of HR with energy expenditure under exercise conditions (see below).
BMR. BMR was measured by indirect calorimetry using ventilated hood calorimetry (Deltatrac II metabolic monitor, Datex Instrumentation Corporation, Helsinki, Finland). The RQ and flow settings were calibrated by reference to alcohol burning every 6 mo and the gas sensors calibrated before each subject measurement using standard gases (CO2 5% and O2 95% by volume, Datex). Measurements of oxygen consumption (˙VO2) and carbon dioxide production (˙VCO2) were performed under standardized conditions, and the equation of Weir(11) was used to calculate energy expenditure. Each child lay supine, having fasted from the previous evening, and rested for 10 min on the couch before commencement of measurements, which were made at 1-min intervals for 20-35 min, depending on the state of restlessness of the child. The first 5 min of each recording were discarded to ensure that steady state conditions were achieved.
RMR. RMR was calculated as the mean energy expenditure for resting activities. These were defined as lying, sitting, and standing quietly, measurements being performed in the afternoon at least 60 min after lunch. Expired gases were collected through a two-way nonrebreathing valve(Salford) and monitored continuously using an on-line breath-by-breath analysis system (Medgraphics, Salford) for a period of 6 min in each posture consecutively. The last 4 min were used to calculate the energy expenditure(11) in each position. HR was recorded during the resting activities by telemetry using the Polar Sport Tester PE4000 (Polar Electo Oy, Finland) recording at 15-s intervals.
Energy expended during physical activity. Energy expended during exercise and physical activity was determined by individual calibration of HR with energy expenditure and measurement of minute by minute ambulatory HR. The former was assessed by simultaneously measuring ˙VO2, VCO2, and HR directly after the resting activities at steadily increasing levels of activity(12). This was achieved by exercising on a motorized treadmill (P. K. Morgan) using an incremental discontinuous protocol. Belt speed commenced at 2 km/h and was raised by 1 km/h until a HR approaching 190 beats/min was reached. Each 3-min exercise period was separated by a rest period of 1 min. For analysis, only the last minute of each 3-min exercise period was used so as to allow for steady state conditions to be achieved. Children walked at speeds of 2 and 3 km/h and were encouraged to jog and run from speeds of 4 km/h and upward. A warm-up period was allowed between the walking and running period to accustom the children to running on the treadmill.
Ambulatory minute by minute HR was monitored under free living conditions(Polar Sport Tester PE4000; Polar Electo Oy, Finland) for the 4 d after HR energy expenditure calibration. This included two week days and two weekend days. Children and their parents were instructed in the use of the apparatus, which included a transmitter secured to the chest by an elasticized belt and a receiver watch worn on the wrist. Recording commenced from the time the subject woke in the morning and was discontinued when retiring to bed in the evening, the times for which were also recorded manually to allow cross-reference with the recording time on the Sports Tester. Information was retrieved by means of an interface unit and micro-computer for calculation of TDEE.
Calculation of TDEE from HR recording. The flex-HR (the HR which defines the difference between rest and exercise) was calculated for each individual as the midpoint between the mean HR for the resting activities and the lowest HR of the exercise activities (walking at 2 km/h). TDEE was then calculated for each individual with reference to their daytime HR recording. For each minute of the day where the HR fell below the flex-HR, energy expenditure was assumed to be equivalent to RMR. For each minute of the day when the HR was greater than or equal to the flex-HR, energy expenditure was calculated by reference to the individual HR energy expenditure regression line. Energy expenditure during sleep was assumed to be equal to BMR. Twenty-four-hour energy expenditure was then computed by summing the estimated energy expenditure from HR monitoring and energy expenditure at night.
Anthropometry and body composition. Height and weight to the nearest 0.1 cm and 0.1 kg, respectively, were measured by a single trained observer using a wall-mounted Harpenden stadiometer (Holtain Ltd., Crymych, Dyfed, UK) and Avery beam balance (Avery Ltd., Birmingham, UK). BMI was calculated from the formula weight (kg)/height2 (m). SDS for the anthropometric data were calculated using the 1990 British reference data(13, 14). Body composition was measured by DEXA scanning (Hologic QDR 1000/W; Hologic, Inc., Waltham, MA). This allowed estimation of FFM and percentage body fat (percent fat)
Statistical Analysis. Medians and ranges are quoted except where otherwise stated. Group medians were compared using the Kruska-Wallis one-way ANOVA test. Paired t tests were used to compare RMR and HR at different postures. The HR and energy expenditure relationship during exercise was established by regression analysis. Associations between variables was tested for by Pearson correlation and partial correlation. Statistical analyses were performed on the Statistical Package for Social Sciences (SPSS) version 6.0 and Minitab version 8.0 for windows.
RESULTS
Because of malfunction of the HR recorders due to detachment of the transmitting belt and/or fiddling with the receiver by the subjects, a number of recordings were lost or were too short to estimate TDEE. Fifty-six children achieved 4-d recording, 22 3-d recording, 8 2-d, and 1 child had only a 1-d recording. One child from the ALL group did not obtain any HR recording and was excluded from the analysis. Table 1 shows the subject details for the remaining 87 children. There was no difference in the length of time since cessation of therapy for the ALL group [5.7 (2.6, 12.8) years] and the other malignancies [5.5 (1.5, 11.8) y]. There were no significant differences in age, height SDS, or weight SDS between groups. Children treated for ALL had a significantly higher BMI SDS and were significantly fatter as estimated by percent fat measurements from DEXA (Table 1).
For all children combined there were significant increases in HR between lying and sitting and sitting and standing (mean difference 6 (95% CI 5-8) beats/min, p < 0.0001 and 16 (95% CI 15-18) beats/min,p < 0.0001, respectively), with no significant difference in the increments between groups. Children treated for ALL had a significantly higher HR during lying and sitting compared with control subjects, yet there was no significant difference in the overall mean resting HR between groups(Table 2). The HR at minimal exercise intensity (2 km/h) was significantly higher in the ALL group compared with controls leading to a significantly higher flex-HR (Table 2). The HR elevation(the percentage increase in HR between rest and flex-HR) was significantly greater in the ALL group compared with control subjects(Table 2). There were no significant differences in the mean daytime HR between groups.
For all groups combined there were significant increments in minute energy expenditure with change of posture from lying to sitting [4.01 (1.54, 8.05) kJ/min to 4.39 (1.85, 9.22) kJ/min, p < 0.0001] and sitting to standing [4.39 (1.85, 9.22) kJ/min to 4.63 (2.16, 9.06) kJ/min, p< 0.0001], with no differences in the change between groups. The mean increment in energy expenditure between BMR and RMR for all groups combined was 1.12 (95% CI 0.74-1.49) MJ/d, p < 0.0001, with no significant differences in the increment between groups.
Group data for TDEE and the components used in its calculation (BMR and RMR) and the daily energy costs of activity above BMR (TDEE-BMR) are shown in Table 3. TDEE and TDEE-BMR were significantly reduced in the ALL group. BMR and TDEE were correlated with body weight (r = 0.83, p < 0.001 and r = 0.41, p < 0.001, respectively), FFM (r = 0.90, p < 0.001 and r= 0.52, p < 0.001, respectively) and age (r = 0.68,p < 0.001 and r = 0.40, p < 0.001, respectively). After controlling for body weight, the correlation between BMR and TDEE with age was no longer significant (partial r = 0.13,p = 0.22 and partial r = 0.15, p = 0.17, respectively). Therefore, to allow comparison of energy expended between individuals of differing body composition and age, BMR and TDEE were corrected for body weight or FFM either by a simple ratio method, or adjusted for body weight or FFM using regression analysis(15), the results of which are shown in Table 4. BMR, after adjustment for body weight, was significantly reduced in the survivors of ALL. TDEE, either expressed as a ratio or adjusted for body weight or FFM, was significantly reduced in children treated for ALL compared with both other malignancies and control subject values (Table 4).
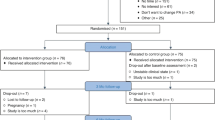
Children treated for ALL spent a significantly lower percentage of the waking hours at a HR greater than or equal to flex-HR [27.3 (1.5, 91.7)%] compared with both other malignancies and control values [46.0 (8.8, 71.2)% and 38.7 (5.8, 91.4)%, respectively, p < 0.05]. The PAL(TDEE/BMR) was also significantly reduced in ALL survivors [1.24 (0.88, 3.12) compared with both other malignancies and control values (1.58 (1.02, 3.03) and 1.47 (0.96, 3.12) respectively, p < 0.01](Fig. 1). The percent time spent with a HR greater than flex-HR and the PAL were correlated (r = 0.76, p < 0.001).
Mean (±SE) PAL (TDEE/BMR) by group. ANOVA*p < 0.01. Dotted lines indicate the range of estimates for the PAL based on normal girls and boys aged 10.5-17.5 y(35).
For all children combined, TDEE was correlated with percent fat after adjusting for body weight (r = -0.39, p < 0.001) or FFM(r = -0.29, p < 0.01) (Fig. 2). Similarly, the percent time spent with a HR greater than flex-HR and PAL were both correlated with percent fat (r = -0.23, p < 0.05 and r = -0.24, p < 0.05, respectively).
DISCUSSION
The relationship between body composition and energy expenditure in children is poorly understood. Theoretically, abnormalities in the energy balance equation, which states that energy intake equals energy expenditure and energy stored, may result in, or be caused by, alterations in body composition. It is recognized that children previously treated for ALL become obese(2, 4, 5, 16, 17), but the etiology is undefined. In the same cohort of children we have previously shown that energy expended during submaximal exercise and at maximal exercise capacity is reduced in children treated for ALL, and negative correlations exist between these variables and body fat(12). The current study demonstrates both reductions in TDEE and patterns of physical activity in children who have previously undergone therapy for ALL, compared with both children treated for a variety of other malignancies and with healthy sibling controls.
Healthy siblings were chosen as controls in this study because this has the advantage of controlling for familial factors that may influence PAL and body composition. As described below, the measurements recorded from the control group are very similar to previously published data on both TDEE and PAL in healthy children. The choice of a heterogeneous group of other malignancies was made to control for the effects of cranial irradiation, which has previously been implicated as a possible cause for the onset of obesity(2), because this group had received neither cranial nor any other radiotherapy. It is accepted that these children were treated for a variety of different tumors and received differing chemotherapy protocols, yet the group as a whole demonstrated very similar results to those of the healthy siblings, and significantly different to those treated for ALL. Insufficient numbers prohibited the breakdown of this group into smaller subgroups to allow examination of the effects that individual chemotherapeutic agents may have on TDEE or PAL. This requires further research.
The assessment of TDEE and patterns of physical activity using HR monitoring is relatively inexpensive and noninvasive and provides information collected under free living conditions. The technique has previously been applied to adults(18–21) and more recently adapted for use in children(22–25). The methodology requires establishment of the relationship between energy expenditure and HR during exercise(26) and the definition of a HR, specific to each individual which discriminates between resting and exercise or activity, known as the flex-HR(22, 23). In the current study the flex-HR was calculated as the midpoint between the mean HR of three resting activities (lying, sitting, and standing) and the lowest HR from exercising on a treadmill. This has been adapted from the method originally used in adults (mean of the highest HR during rest and the lowest during exercise)(21) due to the very high HR of children observed during standing, often higher than that achieved during low intensity exercise (Table 2). The high HR during standing has been attributed to a combination of the physiologic response to stroke volume and a psychologically driven tachycardia in response to excitement and anxiety that the children experience before running on the treadmill(22).
At rest, cardiac output and stroke volume are higher in the lying than in the standing position. A change in posture from lying to standing leads to a decrease in venous return, left ventricular end diastolic volume and pressure, and hence a reduction in stroke volume. In response cardiac output is maintained by a compensatory increase in HR(27). In the early phase of exercise the cardiac output is increased by an augmentation in stroke volume, mediated through the use of the Frank-Starling mechanism, and HR(28). Theoretically, therefore, in the current study the significantly raised HR observed in the survivors of ALL during lying, sitting, and walking at 2 km/h (Table 2) may be explained by an inadequate augmentation in stroke volume, possibly as a result of chemotherapy-induced cardiotoxicity, because previous research has shown that in children who have received anthracycline therapy the shortening fraction is reduced on resting echocardiography(29, 30), and there is an inappropriate increase in shortening fraction in response to stress(31) and exercise(32). This hypothesis is further supported by the significantly higher HR elevation in the ALL group, but this requires further research.
The observed flex-HR for control children in the current study(Table 2) is comparable to that observed in healthy children elsewhere. In an anthropologic study comparing Nepali boys from villages, schools, and the homeless, the mean (SD) flex-HR was 91(7), 100(9), and 103(12) beats/min, respectively(23). There is considerable variability in the flex-HR between subjects, which demonstrates the need for individual determination of the value for each child rather than the use of group means which would lead to large errors in the calculation of TDEE(33). The reliability for this measure has previously been reported as showing a mean difference in flex-HR of only 3 beats/min between an initial and repeat measurement, taken 3 mo apart, which was not significant, although individual differences varied from-15 to +24 beats/min(23). This would suggest flex-HR to be reliable measure for the estimation of TDEE when evaluating groups of children but less reliable on an intraindividual basis. This suggestion is confirmed in the validation of the flex-HR technique against doubly labeled water for the estimation of TDEE. Livingstone et al.(22) measured TDEE in 36 children aged 7.1-15.9 y using both techniques, and although individual discrepancies ranged from -16.9% to+18.8%, as a group the 95% confidence limits for the bias between the two techniques was only -0.56 to +0.01 MJ/d, with the flex-HR slightly underestimating TDEE compared with the doubly labeled water technique(22).
Comparison of BMR and TDEE between individuals of differing age and body composition requires some form of adjustment, because these variables are correlated. After controlling for body size, however, the correlation between BMR and TDEE with age was no longer significant. The most appropriate method for scaling physiologic measurements for individuals of differing body size remains open to debate(15, 34). In the current study the ratio technique, expressing BMR and TDEE either per kg of body weight or FFM, and a mathematical modeling technique have been used(15). TDEE, however expressed, was significantly reduced in the ALL survivors compared with control subjects (Table 4). The median TDEE for the control group (9.23 MJ/d,Table 3) observed in the current study where the ages ranged from 7.6 to 17.3 y compared favorably with that described elsewhere using the same flex-HR technique for children aged from 7.1 to 15.9 y [mean(SD) 8.86 (2.02) MJ/d](22). Recommendations for TDEE in children aged 10.5-17.5 y ranges from 164.7 to 278.0 kJ·kg of body weight d-1(35), which also compares favorably with the current control group with a median TDEE of 185 kJ·kg of body weight d-1 (Table 4).
The reduction in TDEE in survivors of ALL is explained mainly by reduced patterns of physical activity. The daily energy expended above BMR (TDEE-BMR) was significantly reduced (Table 3), as was the PAL and the percentage of the day with a HR greater than flex-HR, in children treated for ALL compared with both those treated for other malignancies and healthy control subjects. In the study of Livingstone et al.(22) a mean (SD) of 41.3% (13.1%) of the day was spent with a HR greater than flex-HR, which compares similarly to the median of that observed for control subjects (38.7%) and other malignancies (46.0%) in the current study.
The significantly raised flex-HR and reduced PAL in children treated for ALL may be as a consequence of reduced levels of physical fitness. Peak oxygen consumption (the oxygen consumption in response to maximal exercise and a component of physical fitness) has been previously shown to be reduced in survivors of ALL(12, 36). Peak oxygen consumption[data previously published(12)] was inversely correlated with flex-HR, r = -0.48 (p < 0.001), and positively correlated with the PAL, r = 0.49 (p < 0.001). Training in obese boys over a 4-wk period has previously been shown to result in significant increases in TDEE and PAL with no significant increase in peak oxygen consumption(37). Further research is required to investigate whether improving physical fitness would result in improved TDEE and PAL in children treated for ALL. The significant association between TDEE, percentage time spent with a HR greater than flex-HR and the PAL with percent fat is difficult to interpret. The reduction in TDEE, percentage time spent with a HR greater than flex-HR, and PAL seen in survivors of ALL may be a result of their obesity rather than a contributory cause. However, previous research has shown that the TDEE tends to be either greater or no different in obese than in nonobese children(38–40). Furthermore, no differences in the PAL between obese and nonobese adolescents have been reported (1.68 versus 1.79 for obese and nonobese boys and 1.74 versus 1.69 for obese and nonobese girls, respectively)(38). This would tend to suggest that children treated for ALL have some intrinsic difference in their PAL due to a mechanism as yet undefined, but has a consequence on their TDEE, which may lead to obesity. This is further supported by the fact that the ALL group had significantly different TDEE and PAL compared with both a group of healthy sibling control subjects and a group of children treated for other malignancies. High dose corticosteroids, as used in the treatment of ALL, are recognized to have adverse effects on body composition leading to an increase in body fat during administration. However, in the current study the children treated for ALL had all finished treatment some time previously, and it was therefore felt that steroids would no longer exert an influence on their body composition. Further metabolic studies are required to resolve these issues.
The mechanism underlying patterns of reduced activity in children treated for ALL remains unknown. Concern has been previously raised about relatively low levels of habitual physical activity in normal children(41). For children treated for malignancy one might speculate that therapy-induced impairment of lung function together with a reduction in exercise capacity may underly the mechanism(12, 36). Jenney et al.(36) found that 42% of children previously treated for ALL reported some degree of exercise intolerance. In this study it was postulated that these children may be overprotected, have lower self-esteem, or simply participate in less activity than their peers. The latter hypothesis is supported by the results of the current study. No difference was found in TDEE, the time spent in activity or the PAL for children treated for malignancies other than ALL, and the control group in the current study. This implies that the mechanism underlying the reduction in such variables may be unique to children treated for ALL. Before the introduction of protocol UKALL XI in the UK, all children treated for ALL received low dose cranial irradiation, which although not often associated with frank GH deficiency, may lead to abnormalities in GH pulsatility(42). It may be postulated that such subtle deficiencies may lead to alterations in body composition, which in turn may have an influence on exercise capacity and PAL. Alternatively, asymptomatic anthracycline-induced cardiomyopathy may lead to a limited exercise capacity and PAL due to an impaired ability to increase stroke volume in response to exercise, which has indirect consequences on body composition(12). This area requires further research.
In conclusion, this study demonstrates that reduced TDEE in long-term survivors of ALL as a consequence of reduced patterns of habitual physical activity are associated with obesity. The mechanism underlying such changes is unknown and requires further research.
Abbreviations
- ALL:
-
acute lymphoblastic leukemia
- BMI:
-
body mass index
- BMR:
-
basal metabolic rate
- CI:
-
confidence interval
- DEXA:
-
dual energy x-ray absorptiometry
- FFM:
-
fat free mass
- HR:
-
heart rate
- PAL:
-
physical activity level
- RMR:
-
resting metabolic rate
- TDEE:
-
total daily energy expenditure
- NHL:
-
non-Hodgkin's lymphoma
- SDS:
-
SD score
References
Jenney ME, Kane RL, Lurie N 1995 Developing a measure of health outcomes in survivors of childhood cancer: a review of the issues. Med Pediatr Oncol 24: 145–153.
Odame I, Reilly JJ, Gibson BES, Donaldson MDC 1994 Patterns of obesity in boys and girls after treatment for acute lymphoblastic leukaemia. Arch Dis Child 71: 147–149.
Van Dongen-Melman JEWM, Hokken-Koelega ACS, Hählen K, De Groot A, Tromp CG, Egeler RM 1995 Obesity after successful treatment of acute lymphoblastic leukemia in childhood. Pediatr Res 38: 86–90.
Didi M, Didcock E, Davies HA, Ogilvy-Stuart AL, Wales JKH, Shalet SM 1995 High incidence of obesity in young adults after treatment of acute lymphoblastic leukemia in childhood. J Pediatr 127: 63–67.
Zee P, Chen CH 1986 Prevalence of obesity in children after therapy for lymphoblastic leukemia. Am J Pediatr Hematol Oncol 8: 294–299.
Wilmore JH 1996 Increasing physical activity: alterations in body mass and composition. Am J Clin Nutr 63 ( suppl): 456S–460S.
Steptoe A, Butler N 1996 Sports participation and emotional well being in adolescents. Lancet 347: 1789–1792.
Eden OB, Lilleyman JS, Richards S, Shaw MP, Peto J 1991 Results of Medical Research Council Leukaemia Trial UKALL VIII (report to the Medical Research Council on behalf of the working party on leukaemia in childhood). Br J Haematol 78: 187–196.
Chessells JM, Bailey CC, Richards S 1992 MRC UKALL X. The UK protocol for childhood ALL: 1985-1990. The Medical Research Council working party on childhood leukaemia. Leukaemia 6 ( suppl 2): 157–161.
Ravussin E, Bogardus C 1989 Relationship of genetics, age, and physical fitness to daily energy expenditure and fuel utilization. Am J Clin Nutr 49: 968–975.
Weir JB deV 1949 New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 109: 1–9.
Warner JT, Bell W, Webb DKH, Gregory JW 1997 Relationship between cardiopulmonary response to exercise and adiposity in survivors of malignancy. Arch Dis Child 76: 298–303.
Freeman JV, Cole TJ, Chinn S, Jones PRM, White EM, Preece MA 1995 Cross sectional stature and weight reference curves for the UK, 1990. Arch Dis Child 73: 17–24.
Cole TJ, Freeman JV, Preece MA 1995 Body mass index reference curves for the UK. 1990. Arch Dis Child 73: 25–29.
Poehlman ET, Toth MJ 1995 Mathematical ratios lead to spurious conclusions regarding age- and sex-related differences in resting metabolic rate. Am J Clin Nutr 61: 482–485.
Schell MJ, Ochs JJ, Schriock EA, Carter M 1992 A method of predicting adult height and obesity in the long-term survivors of childhood acute lymphoblastic leukemia. J Clin Oncol 10: 128–133.
Warner JT, Gregory JW, Webb DKH 1995 Patterns of obesity in boys and girls after treatment for acute lymphoblastic leukaemia. Arch Dis Child 72: 97
Ceesay SM, Prentice AM, Day KC, Murgatroyd PR, Goldberg GR, Scott W, Spurr GB 1989 The use of heart rate monitoring in the estimation of energy expenditure: a validation study using indirect whole-body calorimetry. Br J Nutr 61: 175–186.
Schulz S, Westerterp KR, Brück K 1989 Comparison of energy expenditure by the doubly labeled water technique with energy intake, heart rate, and activity recording in man. Am J Clin Nutr 49: 1146–1154.
Spurr GB, Prentice AM, Murgatroyd PR, Goldberg GR, Reina JC, Christman NT 1988 Energy expenditure from minute-by-minute heart-rate recording: comparison with indirect calorimetry. Am J Clin Nutr 48: 552–559.
Livingstone MBE, Prentice AM, Coward WA, Ceesay SM, Strain JJ, McKenna PG, Nevin GB, Barker ME, Hickey RJ 1990 Simultaneous measurement of free-living energy expenditure by the doubly labelled water method and heart-rate monitoring. Am J Clin Nutr 52: 59–65.
Livingstone MBE, Coward WA, Prentice AM, Davies PSW, Strain JJ, McKenna PG, Mahoney CA, White JA, Stewart CM, Kerr M-JJ 1992 Daily energy expenditure in free-living children: comparison of heart-rate monitoring with doubly labeled water (2H218O) method. Am J Clin Nutr 56: 343–352.
Panter-Brick C, Todd A, Baker R, Worthman C 1996 Comparative study of flex heart rate in three samples of Nepali boys. Am J Hum Biol 8: 653–660.
Panter-Brick C, Todd A, Baker R, Worthman C 1996 Heart rate monitoring of physical activity among village, school, and homeless Nepali boys. Am J Hum Biol 8: 661–672.
Emons HJG, Groenenboom DC, Westerterp KR, Saris WHM 1992 Comparison of heart rate monitoring with indirect calorimetry and the doubly labelled water (2H218O) method for the measurement of energy expenditure in children. Eur J Appl Physiol 65: 99–103.
Bradfield RB 1971 A technique for determination of usual daily energy expenditure in the field. Am J Clin Nutr 24: 1148–1154.
Chaitman B 1992 Exercise stress testing. In: Braunwald E(eds) A Textbook of Cardiovascular Medicine, 4th Ed. WB Saunders, Philadelphia, pp 161–179.
Flamm SD, Taki J, Moore R, Lewis SF, Keech F, Maltais F, Ahmed M, Callahan R, Dragotakes S, Alpert N 1990 Redistribution of regional and organ blood volume and effect on cardiac function in relation to upright exercise intensity in healthy human subjects. Circulation 81: 1550–1559.
Bu'Lock FA, Mott MG, Oakhill A, Martin RP 1995 Left ventricular diastolic function after anthracycline chemotherapy in childhood: relation with systolic function, symptoms, and pathophysiology. Br Heart J 73: 340–350.
Lipshultz SE, Colan SD, Gelber RD, Perez-Atayde AR, Sallan SE, Sanders SP 1991 Late cardiac effects of doxorubicin therapy for acute lymphoblastic leukemia in childhood. N Engl J Med 324: 808–815.
Klewer SE, Goldberg SJ, Donnerstein RL, Berg RA, Hutter JJ 1992 Dobutamine stress echocardiography: a sensitive indicator of diminished myocardial function in asymptomatic doxorubicin-treated long-term survivors of childhood cancer. J Am Coll Cardiol 19: 394–401.
Weesner KM, Bledsoe M, Chauvenet A, Wofford M 1991 Exercise echocardiography in the detection of anthracycline cardiotoxicity. Cancer 68: 435–438.
Li R, Deurenberg P, Hautvast JGAJ 1993 A critical evaluation of heart rate monitoring to assess energy expenditure in individuals. Am J Clin Nutr 58: 602–607.
Nevill AM, Ramsbottom R, Williams C 1992 Scaling physiological measurements for individuals of different body size. Eur J Appl Physiol 65: 110–117.
Food and Agricultural Organisation World Health Organisation United Nations University 1985 Report of a joint expert consultation. Energy and protein requirements. WHO Tech Rep Ser 724: 194–195.
Jenney MEM, Faragher EB, Morris-Jones PH, Woodcock A 1995 Lung function and exercise capacity in survivors of childhood leukaemia. Med Pediatr Oncol 24: 222–230.
Blaak EE, Westerterp KR, Bar-Or O, Wouters LJM, Saris WHM 1992 Total energy expenditure and spontaneous activity in relation to training in obese boys. Am J Clin Nutr 55: 777–782.
Bandini LG, Schoeller DA, Dietz WH 1990 Energy expenditure in obese and nonobese adolescents. Pediatr Res 27: 198–203.
Maffeis C, Schutz Y, Zaffanello M, Piccoli R, Pinelli L 1994 Elevated energy expenditure and reduced energy intake in obese prepubertal children: paradox of poor dietary reliability in obesity?. J Pediatr 124: 348–354.
Bradfield RB, Paulos J, Grossman L 1971 Energy expenditure and heart rate of obese high school girls. Am J Clin Nutr 24: 1482–1488.
Armstrong N, Balding J, Gentle P, Kirby B 1990 Patterns of physical activity among 11 to 16 year British children. BMJ 301: 203–205.
Crowne EC, Moore C, Wallace WHB, Ogilvy-Stuart AL, Addison GM, Morris-Jones PH, Shalet SM 1992 A novel variant of growth hormone(GH) insufficiency following low dose cranial irradiation. Clin Endocrinol 36: 59–68.
Acknowledgements
The authors thank R. Tong (Section of Exercise Physiology, University of Wales Institute, Cardiff) for assistance in collection of the exercise data, J. H. Pearse (Department Medical Physics, University Hospital of Wales, Cardiff) for performing the DEXA scans, and Dr. F. D. J. Dunstan (Department of Medical Statistics, University of Wales College of Medicine, Cardiff) for statistical advice. Finally we thank the children and their parents for participating and making the study possible.
Author information
Authors and Affiliations
Additional information
Supported by a grant from the local childhood oncology charity, Llandough Aims to Treat Children with Cancer and Leukaemia with Hope (LATCH) (to J.T.W.). Support was also provided by Pharmacia and Upjohn.
Rights and permissions
About this article
Cite this article
Warner, J., Bell, W., Webb, D. et al. Daily Energy Expenditure and Physical Activity in Survivors of Childhood Malignancy. Pediatr Res 43, 607–613 (1998). https://doi.org/10.1203/00006450-199805000-00008
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199805000-00008
This article is cited by
-
Self-reported physical activity behaviors of childhood cancer survivors: comparison to a general adolescent population in Korea
Supportive Care in Cancer (2023)
-
Physical activity and fitness among pediatric cancer survivors: a meta-analysis of observational studies
Supportive Care in Cancer (2019)
-
The effect of autonomic nervous system dysfunction on oxygen consumption during daily living activities in patients with spinal cord injury
Spinal Cord (2017)
-
EXERCISE in pediatric autologous stem cell transplant patients: a randomized controlled trial protocol
BMC Cancer (2012)
-
High incidence of fatty liver and insulin resistance in long-term adult survivors of childhood SCT
Bone Marrow Transplantation (2011)