Abstract
Leptin is a 16-kD protein encoded by the ob/ob (obesity) gene. In rodents it plays a role in obesity, diabetes, fertility, and neuroendocrine function. In humans serum concentrations of leptin correlate with total body fat in both adults and children. We measured cord blood leptin in 186 neonates that included 82 appropriate for gestational age (AGA), 47 large for gestational age (LGA), 20 infants of diabetic mothers, 52 preterm infants, and 15 intrauterine growth-retarded (IUGR) infants. There were 16 pairs of twins. The mothers of 17 preterm infants were treated with steroids before delivery. Leptin (mean ± SD) concentration in term, AGA infants (39.4 ± 1.1 wk) with birth weight (BW) of 3.2 ± 0.3 kg, body mass index (BMI) of 12.6 ± 1.1 was 4.01 ± 3.5 ng/mL. BW correlated with cord leptin (p = 0.002) in a multivariate analysis controlling for potential confounders. Both LGA infants and infants of diabetic mothers had higher cord leptin concentration 7.3 ± 3.8 and 6.1 ± 4.8 ng/mL, respectively, compared with AGA infants (p < 0.05). Preterm infants had a mean leptin level of 1.8 ± 0.97 ng/mL and a 3-fold elevation was seen if mothers received steroids antenatally (p = 0.006). IUGR infants had increased leptin (6.5 ± 3.9 ng/mL, p= 0.03). Concerning the twin pairs, the smaller had a higher leptin level compared with larger twin (4.1 ± 9.51 versus 2.8 ± 5.14, p = NS). Neonatal cord leptin concentrations correlate well with BW and BMI. No gender differences were found in cord blood leptin. Maternal obesity had no effect on cord leptin, whereas exogenous maternal steroids increased neonatal leptin concentrations.
Similar content being viewed by others
Main
Obesity has long been considered to have genetic underpinnings, but it was not until 1994 that the obesity gene (ob/ob) was positionally cloned(1). The ob/ob gene product, designated leptin, is a 16-kD adipocyte-derived protein that reflects body fat content(2). Leptin is thought to act as an afferent satiety signal from body fat to the hypothalamus, which causes a reduction in appetite and augments basal metabolic rate when fat stores are replete(3, 4). The obese (ob/ob) mouse, which is markedly hyperphagic and obese, is leptin-deficient due to a mutation in the ob gene. When given leptin, its food intake is reduced and the mice lose weight(1). Although leptin deficiency may play a role in some forms of rodent and human obesity, CNS resistance to leptin may be the more likely explanation(5–7). Leptin is now known to act through high affinity transmembrane receptors(8). High affinity binding sites for leptin have been localized in hypothalamic tissue (arcuate nucleus)(9), leptomeninges, and choroid plexus(10). Point mutations of these receptors have been associated with obesity and diabetes in select animal models(11, 12).
Both serum leptin concentrations and ob gene mRNA are elevated in adipocytes from obese humans. Moreover, there is a consistent correlation between the serum leptin concentration and the percentage of body fat, the BMI, and basal serum insulin concentrations(2, 13). Human adipocytes produce more leptin when the adipose mass increases(14). Obese patients show decreased sensitivity to the action of leptin(13, 14).
Beyond its relation with body-fat mass, little is known about the regulation or secretion of leptin. Caloric restriction reduces serum leptin concentrations and the ob mRNA level in adipose tissue, whereas refeeding increases these levels. Enhanced leptin production has been mimicked by norepinephrine, insulin, and glucocortocoids in cell culture experiments(15–17). Induction of leptin mRNA has been shown to occur in infections using the endotoxin lipopolysaccharide model in hamsters(18). Whether this is the cause for the loss of weight seen in some inflammatory processes remains to be seen. Leptin has also been shown to play a major role in fertility and the induction of puberty(19).
The role of leptin in diabetes (insulin dependent or noninsulin dependent) is not entirely clear(20). Animal experiments have shown that insulin administration can up-regulate leptin mRNA expression. Conversely, administration of recombinant leptin to normal rats significantly reduces appetite, weight, and serum glucose levels(1, 21). In humans, however, neither euglycemic hyperinsulinemia nor hyperinsulinemic hypoglycemia acutely stimulate leptin production for up to 5 h, but chronic effects of insulin have not been examined(22, 23). In patients with non-insulin-dependent diabetes, leptin concentrations differ significantly by diabetic status and are higher in female compared with male subjects(23).
Thus, the exact role of leptin in human glucose and fat metabolism is still unfolding. Little is known regarding the level of this hormone in neonates(24, 25). Pregnancy, a clinically diabetogenic process, causes a large change in body weight and fat content. Infants born to gestational or insulin-dependent diabetic mothers as well as infants who are growth-retarded in utero have metabolic changes that may impact body size, glucose, and intermediary metabolism(26).
The purpose of this study was to: 1) establish normal values for serum concentrations of leptin in neonates by gestational age, BW, and maternal diabetic status; 2) correlate various anthropometric variables of the mother and infant with cord serum leptin concentration; and 3) examine the effect of maternal antenatal steroid treatment on neonatal leptin levels.
METHODS
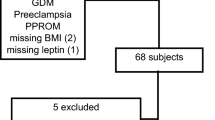
Cord blood samples were collected from live born infants over a 2-mo period at three major maternity hospitals in Milwaukee, WI. Blood was collected in a plain tube for serum leptin measurement and in a EDTA tube for GHB estimation. Serum was separated after the blood was clotted, and both tubes were stored at 4 °C till the time of analysis. BW; length; gestational age (early ultrasound, menstrual history or neonatal examination); maternal diabetes status; and antenatal steroid exposure were recorded. Standard growth curves(27, 28) were used to categorize infants as appropriate, large, or small for gestational age. Diagnosis of IUGR was based on accepted clinical criteria(26). BMI was calculated as BW (kg)/square of length (m)(29). Documentation was made concerning use of antenatal corticosteroids. Maternal antenatal steroid treatment was defined by exposure to at least one dose (12 mg) of betamethasone before delivery. Maternal obesity was defined by a maternal weight >90th percentile for height and a pregravid BMI >29(30). Data sheets were completed by the laboratory personnel or a research nurse at the respective hospitals. Blood samples were analyzed for leptin and GHB in a blinded fashion.
Leptin was measured by an 125I-labeled leptin RIA (Linco Research, St. Louis, MO)(31). The coefficient of variation of this method is 3.5% (intraassay) and 2.4% (interassay). GHB was measured using affinity chromatography (Isolab, Inc., Akron, OH)(32). The GHB assay measures all glycohemoglobins; importantly, fetal Hb does not interfere with this method(33). The study was approved by the respective Internal Review Boards of the three hospitals.
Statistical methods. Data were analyzed using SAS(6, 12) for the PC. Means were compared using the t test(34). Adjustments for multiple comparisons were made using Fisher's least significant difference method. Adjusted means were obtained using analysis of covariance, and differencts were compared using Fisher's least significant difference t test(35). Statistical significance was set at <0.05 when the overall experiment error rate was <0.05.
The relationship between BW, BMI, and leptin concentration was determined using univariate and multivariate regression analysis techniques. Data were assessed using a quadratic term in the regression model(Yij = β0 +β1Xi +β2Xi2 +εij), where Yij is the leptin level, β0 is the intercept, and β1 and β2 are the parameter estimates for the linear and quadratic components, andεij is the error term for the model used. Model assumptions were checked graphically using residual plots. If nonhomogeneous error variances were encountered, then weighted least squares regression analysis was used. The weights used in the regression model were inverse of the square of the dependent variable. Model assumptions were again checked for the weighted regression model. Both linear and quadratic effects were tested in the models. A nonsignificant value of β2 indicated that a quadratic term did not improve the fit of the data.
Multivariate analysis was done using a weighted multiple regression model to determine variables associated with leptin levels. Linear and quadratic components were considered for BW, BMI, and GHB. Forward stepwise regression was used to find the “best” model to predict leptin concentrations(35, 36).
RESULTS
Leptin was detected in the cord blood of preterm infants as small as 24 wk of gestation. Cord leptin concentration increased with increasing BW, BMI, and gestational age (Figs. 1 and 2,Table 1). The relationship between cord blood leptin and BW was quadratic (Fig. 1) but linear for BMI (Fig. 2). There were significant differences in cord serum leptin concentration between infants with different characteristics (Table 1). Analysis of AGA infants (after excluding infants whose mothers received antenatal steroids, infants of diabetic mothers and adjusting for BWs) did not find any gender differences. These leptin levels were (mean ± SD) 3.23 ± 2.76 ng/mL in female infants and 2.98 ± 2.96 ng/mL in male infants(p = 0.15). Intrauterine growth retardation was associated with a significantly higher cord serum leptin concentration compared with BW matched AGA infants (p = 0.03). Maternal obesity had no effect on fetal leptin levels (Table 3). Antenatal steroid exposure was associated with higher cord serum leptin concentration (1.9 ± 5.34versus 6.4 ± 10.01) (p = 0.006)(Fig. 3). The smaller twin had an insignificantly greater leptin level compared with the larger twin (Table 2).
Effect of antenatal steroids on cord serum leptin concentration. Preterm infants (n = 47) whose mothers did not receive antenatal steroids (·) had a mean cord serum leptin of 1.9 ± 0.79 (SEM) compared 6.4 ± 2.42 (SEM) for infants (n = 17) exposed to steroids (▪) antenatally (p = 0.006) (BW-adjusted data).
GHB (%) analysis was performed in the first 97 infants enrolled in the study. Term AGA infants born to nondiabetic mothers had lower GHB levels, 3.01± 0.28%, compared with infants born to diabetic mothers, 3.49 ± 0.6% (p = 0.01). GHB was linearly related to leptin concentration(p = 0.03) (Table 4). There was no statistically significant effect of gestational age, BW, BMI, maternal obesity, or steroid treatment on GHB in all other groups of infants.
In the univariate regression model, BW was a better predictor of leptin concentration than was BMI (Table 4). Multiple weighted regression analysis (excluding infants exposed to antenatal steroids) examined relationships between infant type (AGA, LGA, and IUGR), maternal obesity, diabetes status, BW, BMI, and leptin concentration. Only BW (p = 0.002) showed a significant relationship with leptin concentration(R2 = 0.41).
DISCUSSION
In adults, children, and all normal animals studied to date, serum leptin concentrations correlate with adiposity. This report examines whether a similar relationship is apparent at birth and moreover whether maternal obesity, diabetes, or antenatal steroid treatment is related to neonatal cord leptin concentrations. Our study has shown a direct quadratic relation of serum leptin to BW, and it is linear for BMI. The latter linear relationship may be explained by the fact that in the growth-retarded human fetus there could be sparing of head and length growth (asymmetric IUGR) that leads to a disproportionate change in BMI in relation to BW(37). Analysis of cord blood leptin in 16 pairs of twins revealed no significant differences in BW, BMI, and leptin concentration (Table 2). This could be due to asymmetric growth retardation in the smaller twin due to intrauterine stress and not due to genetic factors as shown in adults(38).
Neonates with IUGR had elevated cord leptin (Table 1 and 3). The etiology of intrauterine growth retardation is multifactorial and includes both maternal and fetal factors. Major causes of IUGR include pregnancy-induced hypertension, intrauterine infections, placental dysfunction, drugs, and genetic factors. Pregnancy-induced hypertension, the commonest cause of IUGR, is associated with increased maternal inflammatory mediators such as tumor necrosis factor-α and IL-12(39, 40). Because inflammation increases leptin expression in cell culture experiments(18) and leptin receptors are closely linked to IL-6 receptors(41, 42), these factors might enhance leptin production. It is possible that insulin resistance and hyperinsulinemia in infants with IUGR is responsible for the elevated cord leptin concentration. Insulin resistance and hyperinsulinemia correlate with leptin concentrations in normal and diabetic adults(43, 44). Moreover, studies in cell cultures suggest that insulin promotes adipocyte leptin production. Because IUGR infants have a smaller, dysfunctional placenta, leptin levels may be inversely correlated with placental weight(24). Finally, elevated concentrations of endogenous corticosteroid hormones, present in some infants with IUGR(45, 46), may contribute to the elevated leptin concentrations. Thus the intrauterine growth-retarded fetus is known to be under a state of stress with high endogenous corticosteroid production, which may augment leptin synthesis(47–50). Intrauterine infections such as syphilis have also been shown to be associated with elevated serum cortisol(47).
Neonatal cord serum leptin levels were elevated in infants whose mothers received antenatal steroids (Fig. 3). The wide variation of leptin concentrations in control and treated infants can be explained by the diverse range of gestational age, BWs, and dosage of steroid used, along with the time lag (12 h to 2 wk) between administration and delivery of the infant. The ability of steroids to increase leptin has been demonstrated in cell culture experiments(48), animal experiments(18), and in adult healthy women(49). That antenatal steroid treatment is associated with increased neonatal leptin suggests that a similar cellular response mechanism may exist in both the fetus and adult. Whether this elevated leptin is persistent or involved in the increased adiposity or catabolism associated with prenatal steroids remains to be determined. There is a possibility that leptin may be secreted periodically during fetal development, and our one measurement at birth may not reflect cumulative secretion of this protein. However, leptin levels in an individual are somewhat stable over a 24-h period, except for a slight circadian rhythm of small amplitude(50).
In summary, neonatal cord serum concentrations of leptin correlate with BW and BMI. IUGR infants and infants whose mothers received antenatal steroids had an increased cord leptin concentration. Leptin, which alters pituitary function and affects numerous extraneuronal tissues, may be responsible for the regulation of body mass of the human fetus and neonate.
Abbreviations
- GHB:
-
glycosylated Hb
- AGA:
-
appropriate for gestational age
- LGA:
-
large for gestational age
- IUGR:
-
intrauterine growth retardation
- BW:
-
birth weight
- BMI:
-
body mass index
References
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM 1994 Positional cloning of the mouse obese gene and its human homologue. Nature 372: 425–432
Considine RV, Sinha M, Heiman ML, Kriauciunas A, Stephens TW, Nyce MR, Ohannesian JP, Marco CC, McKee LJ, Bauer TL, Caro JF 1996 Serum immunoreactive-leptin concentration in normal-weight and obese humans. N Engl J Med 334: 292–295
Yu WH, Kimura M, Walczewska A, Karnath S, McCann SM 1997 Role of leptin in hypothalamic-pituitary function. Proc Natl Acad Sci USA 94: 1023–1028
Stephens TW, Basinski M, Bristow PK, Bue-Valleskey JM, Burgett SG, Craft L, Hale J, Hoffman J, Hsiung HM, Kriauciunas A, MacKellar W, Rosteck PR Jr, Schoner B, Smith D, Tinsley FC, Zhang XY, Heiman M 1995 The role of neuropeptide Y in the antiobesity action of the obese gene product. Nature 377: 530–532
Maffei M, Stoffel M, Barone M, Moon B, Dammerman M, Ravussin E, Bogardus C, Ludwig DS, Flier JS, Tally M, Auerbach S, Friedman JM 1996 Absence of mutation in the human OB gene in obese/diabetic subjects. Diabetes 45: 679–682
Frederich RC, Hamann A, Anderson S, Lollmann B, Lowell BB, Flier JS 1995 Leptin levels reflect body lipid content in mice: evidence for diet-induced resistance to leptin action. Nat Med 1: 1311–1314
Heek MV, Compton DS, France CF, Tedesco RP, Fawzi AB, Graziano MP, Sybertz EJ, Strader CD, Davis HR Jr 1997 Diet-induced obese mice develop peripheral, but not central, resistance to leptin. J Clin Invest 99: 385–390
Tartaglia LA, Dembski M, Weng X, Deng N, Culpepper J, Devos R, Richards GJ, Campfield LA, Clark FT, Deeds J, Muir C, Sanker S, Moriarty A, Moore KJ, Smutko JS, Mays GG, Woolf EA, Monroe CA, Tepper RI 1995 Identification and expression cloning of a leptin receptor, OB-R. Cell 83: 1263–1271
Malik KF, Young WS 1996 Localization of binding sites in the central nervous system for leptin in normal, obese and diabetic mice. Endocrinology 137: 1497–1500
Lynn RB, Cao GY, Considine RV, Hyde TM, Caro JF 1996 Autoradiographic localization of leptin binding in the choroid plexus ofob/ob and db/db mice. Biochem Biophy Res Commun 219: 884–889
Chen H, Charlet O, Tartaglia LA, Woolf EA, Weng X, Ellis SJ, Lakey ND, Culpepper J, Moore KJ, Breitbart RE, Duyk GM, Tepper RI, Morgenstern JP 1996 Evidence that the diabetes gene encodes the leptin receptor: identification of a mutation in the leptin receptor gene in db/db mice. Cell 84: 491–495
Lee GH, Proenca R, Montez JM, Darvishzadeh JG, Lee JI, Friedman JM 1996 Abnormal splicing of the leptin receptor in diabetic mice. Nature 379: 632–635
Dagogo-Jack S, Fanelli C, Paramore D, Brothers J, Landt M 1996 Plasma leptin and insulin relationship in obese and nonobese humans. Diabetes 45: 695–698
Cusin I, Sainsbury A, Doyle P, Rohner-Jeanrenaud F, Jeanrenaud B 1995 The ob gene and insulin: a relationship leading to clues to the understanding of obesity. Diabetes 44: 1467–14670
Campfield LA, Smith FJ, Guisez Y, Devos R, Burn P 1995 Recombinant mouse OB protein: evidence for a peripheral signal linking adiposity and central neural network. Science 269: 546–549
Trayhurn P, Duncan JS, Rayner DV 1995 Acute cold-induced suppression of ob gene expression in white adipose tissue of mice: mediation by the sympathetic system. Biochem J 311: 729–733
De Vos P, Saladin R, Auwerx J, Staels B 1995 Induction of ob gene expression by corticosteroids is accompanied by body weight loss and reduced food intake. J Biol Chem 270: 15958–15961
Grunfeld C, Zhao C, Fuller J, Pollock A, Moser A, Friedman J, Feingold KR 1996 Endotoxin and cytokines induce expression of leptin, the ob gene product, in hamsters. J Clin Invest 97: 2152–2157
Ahima RS, Dushay J, Flier SN, Prabakaran D, Flier JS 1997 Leptin accelerates the onset of puberty in normal mice. J Clin Invest 99: 391–395
Kolaczynski JW, Nyce MR, Considine RV, Boden G, Nolan JJ, Henry R, Mudalier SR, Olefsky J, Caro JF 1996 Acute and chronic effects of insulin on leptin production in humans. Diabetes 45: 699–701
Pelleymounter MA, Cullen MJ, Baker MB, Hecht R, Winters D, Boone T, Collins F 1995 Effects of obese gene product on body weight regulation in ob/ob mice. Science 269: 540–546
Cusin I, Sainsbury A, Doyle P, Rohner-Jeanrenaud F, Jeanrenaud B 1995 The ob gene and insulin. Diabetes 44: 1460–1470
Haffner SM, Stern MP, Miettinen H, Wei M, Gingerich RL 1996 Leptin concentrations in diabetic and nondiabetic Mexican-Americans. Diabetes 45: 822–824
Schubring C, Kiess W, Englaro P, Rascher W, Blum W 1996 Leptin concentration in amniotic fluid, venous and arterial cord blood and maternal serum: high leptin synthesis in the fetus and inverse correlation with placental weight [Letter]. Eur J Pediatr 155: 830
Gross G, Solenberger T, Landt M, Philpott T, Holcomb WL Jr 1997 Leptin levels in newborns of diabetic and non-diabetic mothers. Am J Obstet Gynecol 176 : S162( abstr 562)
Kliegman RM 1997 Intrauterine growth retardation. In: Fanaroff AA, Martin RJ (eds) Neonatal-Perinatal Medicine Diseases of the Fetus and Infant, 6th Ed. Mosby, St. Louis, pp 203–240
Lubchenco LO, Hansman C, Boyd E 1966 Intrauterine growth in length and head circumference as estimated from live births at gestational ages from 26 to 42 wk. Pediatrics 37: 403–408
Battaglia FC, Lubchenco LO 1967 A practical classification of newborn infants by weight and gestational age. J Pediatr 71: 159–163
Cole TJ, Freeman JV, Preece MA 1995 Body mass index reference curves for the UK, 1990. Arch Dis Child 73: 25–29
Field NT, Piper JM, Langer O 1995 The effect of maternal obesity on the accuracy of fetal weight estimation. Obstet Gynecol 86: 102–107
Mai Z, Gingerich RL, Santiago JV, Klein S, Smith CH, Landt M 1996 Radioimmunoassay of leptin in human plasma. Clin Chem 42: 942–946
Abraham EC, Perry RE, Stallings M 1983 Application of affinity chromatography for separation of glycosylated hemoglobins. J Lab Clin Med 102: 187–197
Abraham EC, Stallings M, Abraham A, Elseweidy MM 1983 Affinity chromatography quantitation of glycosylated hemoglobin in newborn infants. Hemoglobin 7: 449–460
SAS/STAT® User's Guide, Version 6, Vol. 2 GLM-VARCOMP( 1990) SAS® Institute Inc., Cary, NC, pp 891–996
Milliken G, Johnson D 1992 Analysis of Messy Data. Vol 1. Designed Experiments. Chapman & Hall, New York, pp 32–37
Neter J, Wasserman W, Kutner MH 1989 Applied Linear Regression Models. Irwin, Boston, MA, pp 225–246
Kramer MS, McLean FH, Oliver M, Willis DM, Usher RH 1989 Body proportionality and head and length sparing in growth-retarded neonates: a critical reappraisal. Pediatrics 84: 717–723
Ronnemaa T, Karonen SL, Rissanen A, Koskenvuo M, Koivisto VA 1997 Relation between plasma leptin levels and measures of body fat in identical twins discordant for obesity. Ann Intern Med 126: 26–31
Kupferminc MJ, Peaceman AM, Wigton TR, Rehnberg KA, Socol ML 1994 Tumor necrosis factor-α is elevated in plasma and amniotic fluid of patients with severe preeclampsia. Am J Obstet Gynecol 170: 1752–1759
Schiff E, Friedman SA, Baumann P, Sibai BM, Romero R 1994 Tumor necrosis factor-α in pregnancies associated with preeclampsia or small-for-gestational-age newborns. Am J Obstet Gynecol 170: 1224–1229
Nakashima K, Narazaki M, Taga T 1997 Overlapping and distinct signals through leptin (OB-R) and a closely related cytokine signal transducer, gp130. FEBS Lett 401: 49–52
Baumann H, Morella KK, White DW, Dembski M, Bailon PS, Kim H, Lai CF, Tartaglia LA 1996 The full length leptin receptor has signaling capabilities of interleukin 6-type cytokine receptors. Proc Natl Acad Sci USA 93: 8374–8378
Barker DJP, Hales CN, Fall CHD, Osmond C, Phipps K, Clark PMS 1993 Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipedemia (syndrome X): relation to reduced fetal growth. Diabetologia 36: 62–67
Goldman SL, Hirata T 1980 Attenuated response to insulin in very low birthweight infants. Pediatr Res 14: 50–53
Parker CR Jr, Buchina ES, Barefoot TK 1994 Abnormal adrenal steroidogenesis in growth-retarded newborn infants. Pediatr Res 35: 633–636
Harlin CA, Tucker JM, Winkler CL, Henson B, Parker CR Jr 1993 Altered adrenal steroid production in term infants having respiratory acidosis. Acta Endocrinol 128: 136–139
Parker CR Jr, Wendel GD 1988 The effects of syphilis on endocrine function of the fetoplacental unit. Am J Obstet Gynecol 159: 1327–1331
Slieker LJ, Sloop KW, Surface PL, Kriauciunas A, LaQuier F, Manetta J, Valleskey JB, Stephens TW 1996 Regulation of expression of ob mRNA and protein by glucocorticoids and cAMP. J Biol Chem 271: 5301–5304
Larsson H, Ahren B 1996 Short term dexamethasone treatment increases plasma leptin independently of changes in insulin sensitivity in healthy women. J Clin Endocrinol Metab 81: 4428–4432
Sinha MK, Sturis J, Ohannesian J, Magosiu S, Stephens J, Heimen ML, Polonsky KS, Caro JP 1996 Ultradian oscillations of leptin in humans. Biochem Biphys Res Commun 228: 733–738
Acknowledgements
The authors thank Chang-Ling Fu, Collen Alex, RN, Gonul Kojasoy, and Tracy L. VanderBloomer for help in sample collection and conducting the RIAs and affinity chromatographic estimations.
Author information
Authors and Affiliations
Additional information
Supported in part by the Max McGee Diabetes Foundation.
Rights and permissions
About this article
Cite this article
Shekhawat, P., Garland, J., Shivpuri, C. et al. Neonatal Cord Blood Leptin: Its Relationship to Birth Weight, Body Mass Index, Maternal Diabetes, and Steroids. Pediatr Res 43, 338–343 (1998). https://doi.org/10.1203/00006450-199803000-00005
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199803000-00005
This article is cited by
-
Lipid profile after omega-3 supplementation in neonates with intrauterine growth retardation: a randomized controlled trial
Pediatric Research (2023)
-
Body adiposity and oral feeding outcomes in infants: a pilot study
Journal of Perinatology (2021)
-
Birth anthropometry and cord blood leptin in Korean appropriate-for-gestational-age infants born at ≥ 28 weeks’ gestation: a cross sectional study
International Journal of Pediatric Endocrinology (2020)
-
Maternal overweight is not an independent risk factor for increased birth weight, leptin and insulin in newborns of gestational diabetic women: observations from the prospective ‘EaCH’ cohort study
BMC Pregnancy and Childbirth (2018)
-
Estimation of umbilical cord blood leptin and insulin based on anthropometric data by means of artificial neural network approach: identifying key maternal and neonatal factors
BMC Pregnancy and Childbirth (2016)