Abstract
Although numerous reports have appeared showing high levels of galactitol in the urine of patients with galactose-1-phosphate uridylyltransferase deficiency, little attention has been paid to measurement of urinary galactonate. Herein we explored the use of 1H and 13C nuclear magnetic resonance, which required only the concentration of urine without derivatization, to detect and quantitate urinary galactonate. We report that transferase deficient infants, as well as adults on galactose restricted diets excrete significant amounts of galactonate, whereas none is detected in the urine of normal subjects. Galactose-toxic infants were found to excrete large amounts of galactonate, which decreased when the lactose-free diet was instituted. We also found that normal individuals subjected to an oral galactose load also excrete high levels of galactonate for at least 4 h after galactose ingestion. Our data provide evidence that the first reaction in the oxidative pathway of galactose metabolism described in rat liver in 1966 is activated in patients with a variety of galactose-1-phosphate uridylyltransferase gene mutations even while on a lactose-restricted diet. In both patients and normal individuals, flux through the alternate galactonate pathway appears to be related to the body galactose burden.
Similar content being viewed by others
Main
In the metabolic pathway described by Cuatrecasas and Segal(1) whereby galactose is converted to d-xylulose by rat liver, the first step involved the oxidation of galactose to galactonate. The existence of this mode of galactose metabolism was substantiated by the observation that rats fed a high galactose diet not only excrete galactonate in the urine but accumulate the compound in several tissues, including liver, intestine, heart, and kidney(2). Guinea pigs on a similar diet also accumulate galactonolactone, the cyclized form of galactonate, in lens and other tissues(3). Galactonate also accumulates in suckling rat liver perfused with high concentrations of galactose(4).
Segal and Cuatrecasas(5) postulated that this direct oxidative pathway might play a role in human galactose disposition when the normal Leloir pathway for galactose metabolism is blocked in galactosemia as a result of defective GALT. This stemmed from their observation(5) that the rate of radioactive CO2 formation from [1-14C]galactose was much greater than that from[2-14C]galactose by transferase-deficient patients, whereas normal individuals showed no difference in the 14CO2 yield from these specifically labeled galactoses(6). In the pathway described by Cuatrecasas and Segal the galactonate formed is subsequently decarboxylated with preferential liberation of the C-1 as CO2, whereas the C-2 of galactose is retained as the first carbon of xylulose. Supporting evidence for the oxidation of galactose to galactonate in man came from two sources. Bergen et al.(7) reported the urinary excretion of large amounts of galactonate when both a normal subject and three galactosemic patients were loaded with galactose and Rancour et al.(2) detected galactonate in liver tissue from a transferase-deficient galactosemic patient. The data thus indicate that the oxidation of galactose to galactonate functions as an alternate metabolic pathway(1) as does the reduction of galactose to galactitol(8).
Although numerous reports have appeared showing abnormally high levels of galactitol in the urine of transferasedeficient galactosemic subjects(9–11), little attention has been paid to measurement of urinary galactonate. There have been only a few instances where the quantitation of urinary galactonate or galactonolactone was attempted in patients with defined mutations in GALT on a lactose-restricted diet. No galactonate was found by gas chromatography before administration of a galactose load to an affected adult(7) or galactonolactone by reverse phase liquid chromatography of urine of a 12-d-old galactosemic infant(12). Because there was ample evidence for the existence of galactonate formation as an alternate route of galactose metabolism, we explored the use of 1H and 13C NMR, which required only a concentration of urine without derivatization, to detect and quantitate urinary galactonate. Herein we report that both infants and adults with GALT deficiency caused by several different mutations on lactose-restricted diets excrete significant amounts of galactonate, whereas none is detected in the urine of normal subjects. Galactose-toxic newborn infants were found to excrete large amounts of galactonate, which decreased when a lactose-free diet was instituted. We also found(7) that normal individuals subjected to an oral galactose load excrete high levels of galactonate for at least 4 h after galactose ingestion.
METHODS
Subjects. Urine samples were collected from 25 Caucasian and 3 African American patients with galactosemia, ages 13 d to 33 y. All had absent red blood cell GALT, undectable enzyme red blood cell GALT banding pattern on isoelectric focusing, and elevated red cell galactose 1-phosphate levels. Young infants had been placed on lactose-free diets as soon as the diagnosis was made. All of the older patients were on lactose-restricted diets.
Normal urine specimens were obtained from 90 subjects ranging in age from newborns to 55 y. The samples were obtained from infants and children in the general pediatric clinics and normal adult laboratory personnel.
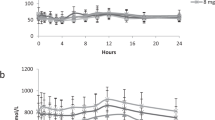
Galactose loading studies were performed in three normal adults. one woman and two men, ages 28-45 y(13). All studies were performed after a minimum of an 8-h overnight fast. Urine was collected before and 2 and 4 h after oral ingestion of 50 g of galactose (Pfanstiehl Laboratories, Inc., Waukegan, IL). These studies were approved by the Children's Hospital of Philadelphia and the Emory University Committees for the Protection of Human subjects.
Molecular analyses. The Q188R and S135L mutations were identified using PCR and restriction enzymes by previously described techniques(13, 14). Molecular genotypes of all other mutations were accomplished by screening single-stranded conformational polymorphisms and direct sequencing of PCR-amplified DNA on an ABI Prism 310 genetic analyzer using previously reported methods(2).
1H NMR spectroscopy of urine. Proton NMR spectroscopy was performed at 400 MHz on a Bruker AM 400 wide-bore spectrometer. For intact urine analysis, 0.5 mL of untreated urine was introduced in a 5-mm NMR tube. whereas concentrated urine samples were obtained by lyophilizing 5 mL of urine to dryness and dissolving the residue in 0.5 mL of D2O. In both cases, an external standard made of a sealed capillary containing a solution of TSP in D2O was introduced in the NMR tube. The TSP resonance served as chemical shift reference and allowed for quantitation of the metabolites. The capillary had been previously calibrated against solutions of known concentration. Standard quantitative acquisition conditions were as follows: 45° pulse. 8-s repetition time, and water saturation during the relaxation delay (4.75 s), 0.305 Hz/Pt digital resolution [spectral width 5000 Hz, 32K data points (data size)], 32-128 scans, i.e. 4-17 min of data collection. The power used for water saturation was 30 mW in the intact urine (H2O) and less than 10 mW in concentrated urine (D2O). Care was taken to use the minimum power to minimize the saturation of the resonances close to the water peak such as galactonate H2.
13C NMR spectroscopy. Proton-decoupled carbon spectra of the concentrated urine samples were obtained at 100.62 MHz in a 5-mm dual probe. Acquisition conditions were as follows: 20° pulse flip angle, 1.3-s repetition time, a value equal to 2T1 of CH2s, spectral width 25 kHz, data size 64K, 40,000 scans. The free induction decays were zero filled to 128K and a Lorentzian to Gaussian transformation (line broadening = -1.2 Hz, Gaussian factor = 0.1) was applied before Fourier transformation. Relaxation times of the methylene carbons of galactitol, galactonate, citrate, and hippurate were measured in a concentrated urine sample by inversion/recovery and were found to be of the order of 0.6 ± 0.1 s. Because the methylene carbon resonances are fully relaxed under the chosen acquisition conditions and the nuclear Overhauser effect factors can be assumed equal, quantitation of galactitol, and galactonate was achieved by comparing the intensity of their C6 methylene with the intensity of the methylene of citrate and/or hippurate, the concentration of which is measured in the intact urine. Quantitation of galactonate was routinely obtained from both proton and 13C spectra of 10-fold concentrated urine because NMR spectra of some of the more dilute urine specimens gave insufficient signal to noise ratio to detect and quantitate galactonate.
Level of detection and variability. By diluting one of the adult most concentrated urine we were able to determine that the level of detection for galactonate is approximately a 50 μM concentration in urine. Likewise, by adding galactonate to a normal urine so as to make the concentration 50 μM we could observe the galactonate H2 signal with a signal-to-noise ratio of 5/1, a value we consider the minimum necessary for quantitation. Expressed in millimoles per mol of creatinine, the minimum level of detection is a function of the creatinine concentration: in the 10-fold concentrated urine used, the minimum level of detection for galactonate ranged between 2 and 5 mmol/mol of creatinine. We repeated the quantitation of galactonate twice in five samples at several hours to a few days interval and found a variability of 10%.
RESULTS
1H and 13C spectra of galactonate and pH variation of the resonances. Proton and carbon resonance assignments for known galactonate and for comparison galactitol in solution in D2O were done according to published values(16) and updated by us using two-dimensional techniques, i.e. COSY(17) and heteronuclear multiple quantum correlation(18) experiments. (1H and 13C chemical shifts of galactitol and galactonate in D2O (reference TSP for1 H and dioxane for 13C) are as follows. Galactitol:δCH2-1 = 3.7 ppm; δH2 = 3.98 ppm; δH3 = 3.7 ppm;δC1 = 63.33 ppm; δC2 = 70.23 ppm; δC3 = 69.40 ppm. Galactonate: δH2 = 4.27 ppm; δH3 = 3.99 ppm; δH4 = 3.65 ppm;δH5 = 3.98 ppm; δCH2-6 = 3.7 ppm; δC1 = 179.6 ppm;δC2 = 71.72 ppm; δC3 = 71.5 ppm; δC4 = 69.95 ppm; δC5= 70.28 ppm,; δC6 = 63.51 ppm.) Figure 1 shows the one-dimensional 1H and 13C spectra of each metabolite and the13 C spectrum of a mixture. Although all the proton resonances of galactitol are concentrated in the region between 3.9 and 3.5 ppm, the H2 signal of galactonate is shifted down field by the effect of the carboxyl group and appears at 4.28 ppm as a small doublet with a coupling constant JH2-H3 of 1.5 Hz.
All carbon resonances for both compounds are distinct and have been unambiguously assigned. Their terminal CH2s have different chemical shifts and appear in the same order through the range of pH 5 to 8. Chemical shifts of galactonate protons and carbons particularly H2 and C2 are slightly pH dependent in the range of pH 5 to 8, whereas, those of galactitol are not.
Proton and carbon spectra of concentrated urine. In the proton spectrum of urine, galactonate is identifiable by the resonance of the H2 proton, which appears in a relatively empty region close to 4.30 ppm. Figure 2 shows the 4.3-4.55 ppm region of a urine sample of an adult on a normal diet (A), urine of the same adult 2 h after ingestion of a 50-g galactose load (B), and urine of a classic galactosemic patient aged 30 y on an excellent galactose-restricted diet(C). In the 13C spectrum, the terminal CH2 carbon of galactonate and galactitol resonate at 63.68 and 63.6 ppm, respectively.Figure 3 shows the 63-64 ppm region in the carbon spectrum of the urine samples of Figure 2.
Galactonate and galactitol CH2-6 resonances(region 63-64 ppm) in the carbon spectrum of the urine samples ofFigure 2.
Urinary galactonate excretion by normal subjects. Galactonate was not detectable by 1H NMR in urine from 90 normal subjects ranging in age from the newborn period to adulthood. High levels of it, however, were found in urine 2 h after oral administration of 50 g of galactose to three adult normal volunteers. Table 1 gives the individual values expressed in millimoles per mol of creatinine. The galactonate increased from being undetectable to an average of 126 mmol/mol of creatinine at 2 h. The level continued to increase to an average of 206 mmol/mol of creatinine at 4 h. The measurement of galactonate and galactitol was also performed with 13C NMR and their ratio calculated. Galactonate excretion was larger than galactitol with the ratio of galactitol to galactonate averaging 0.66 at 2 h. The ratio decreased by 50% at 4 h due to the increase in galactonate, whereas galactitol excretion tended to level off.
Urinary galactonate excretion by patient with galactosemia.Table 2 shows the urinary galactonate excretion according to age of 23 classic Caucasian galactosemic patients and of 3 African American variants with different GALT mutations and considerable ability to metabolize galactose(19). The analysis was performed by both1 H and 13C NMR. All of the galactosemic subjects excreted excessive amounts of galactonate. There was some variability between the values determined by proton and carbon NMR. This variation depended on the difference in signal-to-noise ratio between the two methods. The correlation coefficient (r2) of the values for the two methods for all the data in Tables 1, 2,and 3 was 0.99.
The urine of the two youngest patients was obtained at the time of diagnosis, before diet therapy, and contained the highest amount of galactonate. Overall, the three youngest patients excreted the largest amounts and had mutant alleles known to ablate GALT activity. All of the Caucasian patients except for one excreted less than 100 mmol/mol of creatinine after the age of 2 y when quantitated by 1H NMR. There is some relationship to the GALT genotype. Two of the patients with the S135L mutation had lower galactonate excretion than those with ablative genotypes. In this category the homozygosity for Q188R was not important; the average excretion of proton NMR-determined galactonate by six Q188R homozygotes was 47.5 ± 16.4 mmol/mol of creatinine (mean ± SD), whereas that of the eight Q188R compound heterozygotes was 62.4 ± 10.1 (p < 0.6). Among these compound heterozygotes for the Q188R mutation several new G alleles were found which include: ΔT→C2359 which produces a stop codon in exon 11, K285N (frequent in Croatia, Bosnia, and Austria), Q334K, and R259W. The second allele in the S135L/other GALT genotype was a ΔT→C transition at bp 2749. This is a silent polymorphism at amino acid 315 (H315H) but produces a splice site in exon 10. Both G alleles are probably“leaky.” This may account for the fact that the lowest excretion of galactonate occurred in the two older patients with an S135L mutation, which is consistent with their ability to metabolize galactose(19, 20). The galactitol to galactonate ratio measured by 13C averaged 3.67 in one and 2.98 in the other, values not significantly different (p < 0.18). However, four of the six Q188R homozygote subjects had a galactitol to galactonate ratio greater than 3, whereas only two of the eight compound galactosemic subjects had a ratio greater than 3. In the subjects less than 1 mo of age, some in the“toxic state,” the ratio of galactitol to galactonate was greater than 10.
Table 3 shows the galactonate excretion of two patients homozygous for the Q188R mutation during the 1st y of life after instituting a lactose-restricted diet. The data appear to substantiate the impression from Table 2 that the highest excretion of galactonate is in the very young exposed to galactose and that with the dietary treatment the levels decrease but slowly. The data again reveal the very high ratio of galactitol to galactonate during the 1st y of therapy, consistent with the known very high galactitol excretion in the young newly diagnosed and treated infant(11).
DISCUSSION
1H and 13C NMR has been used to absolutely identify and quantitate the presence of elevated amounts of galactonate in the urine of patients with uridyltransferase-deficient galactosemia. With this technique no galactonate was detected in the urine of normal subjects except when they were given a large oral load of galactose. Galactonate was found in the urine of all the galactosemic subjects examined. The levels varied in the patients and were greatest in infants during the first few months of treatment with a lactose-free diet. Urinary galactonate measurement offers a new parameter in addition to red cell galactose 1-phosphate assay and urinary galactitol excretion to assess the metabolic status of galactosemic patients.
Our data provide evidence that the first reaction in the oxidative pathway of galactose metabolism described by Cuatrecasas and Segal(1) occurs as an alternate pathway when the normal metabolism of galactose is blocked. In this pathway shown inFigure 4, galactose is oxidized to galactonate in an NAD-dependent reaction followed by a subsequent formation of the 3-keto compound. The latter then undergoes decarboxylation, liberating carbon 1 to form xylulose. The preferential oxidation to CO2 of[1-14C]galactose compared with [2-14C]galactose by galactosemics led Segal and Cuatrecasas(5) to postulate that this pathway functioned as an important alternative pathway in afflicted subjects. Evidence for oxidation of galactose to galactonate is the finding of galactonate in the liver of a galactosemic patient(2).
Galactose conversion to d-xylulose: an alternate pathway of galactose metabolism involving oxidation to galactonate(1).
We have not observed other intermediates of the pathway in the urine NMR spectra. Because xylulose easily enters the hexose-monophosphate pathway of glucose metabolism, any formed intracellularly would be readily phosphorylated and metabolized. The fact that galactonate is found suggests that it accumulates in various tissues, and that a subsequent reaction in the pathway is a rate-limiting one. That galactonate accumulates in the liver of normal rats fed a high galactose diet(2) as well as mice with absent GALT (S. Segal, N. Leslie, P. MacNamara, S. Wehrli, R. Reynolds, and C. Yeager, unpublished results) supports this supposition. Perfusion of normal suckling rat liver with fluids with very high galactose concentrations does result in the presence of xylulose as well as galactonate in tissue extracts(4).
Although galactonate was not detected in the urine of normal individuals of any age, large amounts were found 2 and 4 h after oral ingestion of 50 g of galactose by normal adult subjects. These data provide evidence that the potential for galactose oxidation to galactonate exists in normal subjects when tissues are exposed to amounts of galactose that overwhelm the capacity of the Leloir pathway involving GALT, which is the prime route for the metabolic disposition of the sugar. Galactitol in large amounts was also excreted in the urine after the galactose load, indicating that this alternate pathway also functioned to handle the galactose burden. Thus, the tissue level of galactose may determine the flux through either alternate pathway in both control and galactosemic subjects. In normal subjects, however, the galactitol to galactonate ratio was less than 1, whereas, in all the urine specimens from older galactosemic subjects the ratio was 2 to 3, with some as high as 10 or 11 in newly treated infants. This reversal could be due to a relatively higher activity of the aldose reductase, the enzyme which produces galactitol, in galactosemic subjects who are continuously exposed to endogenously synthesized galactose(19) compared with normal subjects who dispose of galactose rapidly. An enhanced ability to convert galactose to galactitol in patients with a block in the Leloir pathway due to different GALT mutations may depend on both the duration and the degree to which galactose is elevated. Although the data suggest that galactitol formation may predominate as an alternate pathway of galactose metabolism, it should be recalled, however, that galactitol undergoes no further metabolism(20), whereas galactonate is capable of further metabolism and is only an intermediate in the galactose conversion to xylulose. In addition, the handling of the two compounds by the kidney may play a role in this urinary excretion pattern.
The previous demonstration of galactonate in the urine of galactose loaded subjects was performed using gas chromatography with identification by mass spectrometry(7). We have also used an equally sophisticated method. NMR. NMR is an ideal noninvasive tool for performing qualitative and quantitative analysis of biologic samples. We have previously used quantitative 31P NMR to measure red blood cell nucleotide sugars(21). Although the instrumentation is costly and requires special expertise for its operation, the ability to determine the urinary galactonate concentration in underivatized urine from galactosemic patients makes sample preparation simple. In this regard, we could not always detect galactonate in very dilute urine samples and resorted to routinely concentrating the urine specimens 10-fold. With this maneuver we could detect galactonate readily in galactosemic subjects, but not in normal subjects with a detection limit as low as 2 mmol/mol of creatinine or 3 mg/g of creatinine. In the concentrated urine, proton spectra are obtained in 4-17 min of scanning time. The quantitation of galactonate in the proton spectra is limited not just by its absolute concentration, however, but more importantly by the presence of other signals, which may overlap or interfere with the detection of the doublet signal of the H2 proton of galactonate.
The lower sensitivity of the 13C spectra with the Bruker 400 MHz instrument necessitated an acquisition time of several hours, usually performed by an overnight examination. The huge difference in time and cost is in part compensated by the information derived from the 13C spectra. There is much less overlap in the 13C spectrum, however, because each carbon in a molecule gives rise to a single line, and the resonances of carbohydrates are well separated. Furthermore, provided the acquisition conditions are adequate, the 13C spectrum allows for quantitation of both galactitol and galactonate and provides a direct and precise measurement of the galactitol/galactonate ratio. Galactitol cannot be measured in the proton spectrum because its resonances appear in a crowded region of the1 H spectrum. Our measurement of galactonate in the urine by both proton and 13C methods shows good agreement in most specimens. For practical purposes of analytical costs and time, the proton spectra offers advantages. Indeed, 13C NMR is not needed to measure galactitol, because it can be more cheaply measured by ordinary gas chromatography(11).
The urinary excretion of both galactitol and galactonate by galactosemic patients with an array of GALT gene mutations and who are well treated with lactose-free diets probably reflects our previously reported findings of significant endogenous production of galactose(21). That galactonate formation occurs in all of the patients thus far studied suggests that a consideration of this alternate oxidative pathway should be made in the evaluation of the metabolism of galactose in affected patients. An assessment of the extent of the function of this metabolic route may be important in relation to the longterm outcome of galactosemic patients(10, 24). Unlike galactitol, which is essentially an end-product of the polyol pathway, galactonate can be further metabolized to glucose. In the patient with GALT deficiency, flux through the oxidative galactonate pathway could account for the bulk of the endogenously synthesized galactose and, thus, needs to be carefully assessed as an important variable which might influence clinical outcome.
Abbreviations
- GALT:
-
galactose-1-phosphate uridylyltransferase
- NMR:
-
nuclear magnetic resonance
- TSP:
-
trimethylsilylpropionic acid
References
Cuatrecasas P, Segal S 1966; Galactose conversion to D-Xylulose: An alternate route of Galactose metabolism. Science 153: 549–531.
Rancour NJ, Hawkins ED. Wells WW 1979; Galactose oxidation in liver. Arch Biochem Biophys 193: 232–241.
Wada E 1986; r-Galactonolactone in experimental galactosemic animals. Arch Biochem Biophys 251: 215–221.
Rogers S, Lichtenstein G, Gentile D, Segal S 1984; Accumulation of galactonate in liver of suckling rats perfused with galactose. Biochem Biophys Res Commun 118: 304–309.
Segal S, Cuatrecasas P 1968; The oxidation of14 C-galactose by patients with congenital galactosemia: evidence for a direct oxidative pathway. Am J Med 44: 340–347
Segal S, Blair A 1961; Some observations on the metabolism of d-galactose in normal man. J Clin Invest 40: 2016–2025.
Bergren WR, Ng WG, Donnell GN, Markey SP 1972; Galactonic acid in galactosemia: identification in the urine. Science 176: 683–684.
Quan Ma R, Wells HJ, Wells WW 1966; Galactitol in the tissues of a galactosemic child. Am J Dis Child 112:477-478. Am J Dis Child 112: 477–478.
Roe TF, NG WG, Bergren WR. Donnell GN, 1973; Urinary galactitol in galactosemic patients. Biochem Med 7: 266–273
Berry GT, Palmieri M, Gross KC, Acosta PB, Henstenburg JA, Mazur A, Reynolds R and Segal S 1993; The effect of dietary fruits and vegetables on urinary galactitol excretion in galactose-1-phosphate uridyltransferase deficiency. J Inherited Metab Dis 16: 91–100.
Jakobs C, Schweitzer S, Dorland B 1995; Galactitol in Galactosemia. Eur J Pediatr 154:S50–S52.
Rakotomanga S. Baillet A, Pellerin F, Baylocq-Ferrier D 1991; Simultaneous determination of gluconolactone, galactonolactone and galactitol in urine by reversedphase liquid chromatography: application to galactosemia. J Chromatogr 570: 277–284.
Elsas LJ, Langley S, Paulk EM Hjelm LN Dembure PP 1995; A molecular approach to galactosemia. Eur J Pediatr 154:S21–S27.
Langley SD, Lai K, Dembure PP Hjelm LN Elsas LJ 1997; Molecular basis for Duarte and Los Angeles variant galactosemia. Am J Hum Genet 60: 366–372.
Gibson JB, Berry GT, Mazur AT, Palmieri MJ, Reynolds RA, Segal S 1995; Effect of glucose and galactose loading in normal subjects on red and white blood cell uridine diphosphate sugars. Biochem Mol Med 55: 8–14.
Bock K, Petersen C 1983; Carbon-13 nuclear magnetic resonance spectroscopy of monosaccharides. Adv Carbohydr Chem Biochem 41: 27–65.
Bax A, Freeman R, Morris G 1981; Correlation of proton chemical shifts by two-dimensional Fourier transform NMR. J Magn Res 42: 164–168.
Bax A, Griffey RH, Hawkins BL 1983; Correlation of proton and nitrogen-15 chemical shifts by multiple quantum NMR. J Magn Reson 55: 301–315.
Lai K, Langley SD, Singh RH, Dembure PP, Hjelm LN, Elsas LJ 1996; A prevalent mutation for galactosemia among black Americans. J Pediatr 128: 89–95.
Baker L, Mellman WJ, Tedesco TA, Segal S 1966; Galactosemia: symptomatic and asymptomatic homozygotes in one Negro sibship. J Pediatr 68: 551–558.
Berry GT, Nissim I, Zhiping L 1995; Endogenous synthesis of galactose in normal men and patients with herediatary galactosemia. Lancet 346: 1073–1074.
Weinstein AN, Segal S 1968; The metabolic fate of[1-14]galactitol in mammalian tissue. Biochim Biophys Acta 156: 9–16.
Wehrli SL, Palmieri MJ, Berry GT, Kirkman HN, Segal S 1992; 31P NMR analysis of red blood cell UDP glucose and UDP galactose: comparison with HPLC and enzymatic methods. Anal Chem 202: 105–110.
Waggoner DD. Buist NR. Donnell GN Buirst NR Donnell GN 1990; Long-term prognosis in galactosemia: results of a survey of 350 cases. J Inherited Metab Dis 13: 802–818.
Acknowledgements
The authors thank Dr. Rosemary Casey, Director of the General Pediatrics Clinic, Children's Hospital of Philadelphia, who aided the study by obtaining urine samples from normal infants and children.
Author information
Authors and Affiliations
Additional information
Supported by a program project Grant HD29847 from the National Institutes of Health. The NMR instrument used is in the Core Facility of the Joseph Stokes, Jr. Research Institute, Children's Hospital of Philadelphia.
Rights and permissions
About this article
Cite this article
Wehrli, S., Berry, G., Palmieri, M. et al. Urinary Galactonate in Patients with Galactosemia: Quantitation by Nuclear Magnetic Resonance Spectroscopy. Pediatr Res 42, 855–861 (1997). https://doi.org/10.1203/00006450-199712000-00022
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199712000-00022
This article is cited by
-
Classical Hereditary galactosemia: findings in patients and animal models
Metabolic Brain Disease (2023)
-
Sweet and sour: an update on classic galactosemia
Journal of Inherited Metabolic Disease (2017)
-
Quantitative analysis of metabolite concentrations in human urine samples using 13C{1H} NMR spectroscopy
Metabolomics (2009)
-
Classical galactosaemia revisited
Journal of Inherited Metabolic Disease (2006)