Abstract
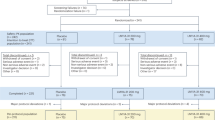
Congenital ornithine transcarbamylase (OTC) deficiency results in neuropathologic damage to the cerebral cortex, basal ganglia, and thalamus. However, the precise nature of the cell loss, as well as the pathophysiologic mechanisms responsible for it, have not been fully elucidated. In the present study, densities of the M1 and M2 subclasses of muscarinic cholinergic binding sites were assessed using quantitative receptor autoradiography in the brains of sparse-fur (spf) mice with congenital OTC deficiency and in age-matched CD-1 controls. Densities of binding sites for the muscarinic M1 subtype ligand[3H]pirenzepine were reduced by 24-54% (p < 0.01) in frontal cortex, caudate/putamen, and hippocampal CA1 and CA2 areas. Since muscarinic M1 sites are localized presynaptically, their selective loss, together with a previous report of reduced activities of the presynaptic cholinergic enzyme choline acetyltransferase, confirms that loss of cholinergic neurons is an important feature of congenital OTC deficiency. Densities of binding sites for the predominantly postsynaptic muscarinic M2 subtype ligand 3H-AFDX 384 were increased by up to 60%(p < 0.01) in cerebral cortex, hippocampus, globus pallidus, as well as in thalamic and hypothalamic structures of OTC-deficient mice. Increased M2 sites in the cerebral cortex, hippocampus, and thalamus are most likely the result of up-regulation of these sites after the loss of the presynaptic neuron. These findings support the presence of a central muscarinic cholinergic lesion in congenital OTC deficiency.
Similar content being viewed by others
Main
Congenital deficiencies of urea cycle enzymes result in chronic hyperammonemia and a spectrum of neurologic symptoms ranging from behavioral abnormalities and severe cognitive deficits to convulsions and mental retardation. The most common inherited metabolic disorder of the urea cycle in humans involves OTC (EC 2.1.3.3), the enzyme that catalyzes the second step of the urea cycle(1). Neuropathologic studies in OTC deficiency in humans reveal cortical neuronal loss, Alzheimer type II astrocytosis, and spongiform changes in basal ganglia and thalamus(2, 3). The exact pathophysiologic mechanism responsible for the neurologic abnormalities in OTC deficiency, however, is not known, but has been attributed to ammonia neurotoxicity(4).
The spf mouse with an X-linked inherited deficiency of OTC is an ideal animal model for the study of the neurochemical consequences of congenital OTC deficiency(5, 6). Serum and brain ammonia levels are significantly increased in OTC-deficient spf mutant mice compared with normal controls(7, 8). Several recent studies have identified alterations of monoamine neurotransmitter-related enzymes and of serotonin 5-HT1A and 5-HT2 receptors in the spf mouse brain(9, 10). In addition, changes in the concentrations of excitatory and inhibitory neurotransmitter amino acids(11) as well as significant deficits of cholinergic neuronal parameters(12, 13) have been reported in the brains of these mice. For example, using an immunohistochemical technique and MAb to ChAT, a significant loss of cholinergic neurons in frontal cortex, diagonal band, and medial septum of spf mutant mice was demonstrated(12). It was suggested that cholinergic neuronal loss could explain the cognitive deficits characteristic of congenital OTC deficiency. In the present study, to further elucidate the nature of the cholinergic lesions in OTC deficiency, we used a quantitative autoradiographic approach to evaluate muscarinic cholinergic binding sites in spf mouse brain and age-matched CD-1 controls. Both M1 and M2 subtypes of muscarinic sites were measured using [3H]PZ, a ligand which binds with high selectivity to the M1 subtype(14) and [3H]AFDX 384, a ligand with high selectivity for the M2 subtype(15, 16).
METHODS
Animals. The parent stock for the colony of spf mutant mice maintained in our laboratory was originally supplied by Dr. L. B. Russell of the OakRidge National Laboratories, OakRidge, TN(5). The mutant gene was subsequently transferred to the CD-1 strain (Canadian Breeding Farms, St-Constant, Que.). All of the male progeny from spf/spf homozygous females and normal CD-1 males(6), being spf/Y were separated by simple sexing. Adult male spf mice (60-80 d of age) were used as normal controls. Animals were maintained on a 12-h light/12-h dark cycle with free access to diet (Purina Mouse Chow, Ralston Purina, St. Louis, MO) and water, and experiments were performed according to the guidelines of the Canadian Council on Animal Care (Guide to the Care and Use of Experimental Animals, Vol. 2, 1984).
Materials. [3H]PZ (71.92 Ci/mmol) and [3H]AFDX 384 (120 Ci/mmol) were purchased from DuPont NEN, Boston, MA. Atropine sulfate and other chemicals (reagent grade) were purchased from Sigma Chemical Co., St. Louis, MO.
Tissue preparation. Animals were decapitated, and the brains were removed and rapidly frozen in isopentane chilled on dry ice (-20 °C). Brain sections 20 μm thick were cut in the sagittal plane with a microtome cryostat at -18 °C and were thaw-mounted onto gelatinized slides. Sections were stored at -70 °C until use.
[3H]PZ autoradiography. Brain sections were preincubated for 15 min in Krebs buffer (pH 7.4) at room temperature, then incubated in buffer in the presence of 20 nM [3H]PZ(17). After a 60-min incubation, slides were transferred through three rinses (4 min each) of ice-cold 50 mM Tris-HCl buffer (pH 7.4), followed by a fast rinse in distilled water.
[3H]AFDX 384 autoradiography. Incubation of brain sections was carried out in Krebs buffer, pH 7.4, at 4°C for 1 h in the presence of 10 nM [3H]AFDX 384. From preliminary experiments using various incubation times and ligand concentrations, optimal results were obtained with an incubation time of 60 min at 4 °C in the presence of 10 nM [3H]AFDX 384. After incubation, slides were transferred sequentially through three rinses (4 min in each) of Krebs buffer at 4 °C followed by dipping in cold distilled water.
For both [3H]PZ and [3H]-AFDX 384, nonspecific binding (less than 15% of total binding for both radioligands) was determined in adjacent brain sections in the presence of 2 μM atropine. After washing in distilled water, slides were dried in a cold air stream. The labeled dried tissue sections along with tissue-calibrated standards of known 3H concentrations (Amersham microscales) were apposed to 3H-sensitive hyperfilm (Amersham Corp., Arlington Heights, IL) for 6 wk for [3H]PZ and 8 wk for [3H]AFDX 384. Films then were processed using Kodak D-19 developer and Kodak rapid fixer. The quantity of bound ligand was estimated by quantitative densitometry analysis using an MCID computer-based densitometer and image analysis system (Imaging Research, Ontario, Canada). The brain regions of interest were defined according to an established mouse brain atlas(18). The quantity of radiolabeled ligand bound to various brain regions was calculated from the specific activity of the respective ligands.
Statistics. Statistical analysis of binding site densities inspf versus CD-1 control brain regions was performed using oneway analysis of variance with Fisher's post hoc test.
RESULTS
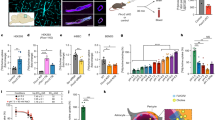
[3H]PZ binding to the M1 muscarinic cholinergic receptor subtype was highest in the caudate/putamen and hippocampus, followed by the cortical areas, whereas lower levels were observed in cerebellum and colliculi(Figs. 1 and2). There were no detectable[3H]PZ binding sites in trigeminal nucleus. This relative distribution of binding sites was similar to that previously reported(14, 19). Significant increases in [3H]PZ binding were seen in parietal cortex, temporal cortex, globus pallidus, anterodorsal and ventroposterior thalamic areas, and hypothalamus of congenitally OTC-deficient spf mice compared with normal CD-1/Y controls (Fig. 1).
Quantitative autoradiographic analysis of [3H]PZ binding sites in selected brain regions of CD-1 control and spf mutant mice. Values are expressed as mean ± SEM from duplicate sections of five different animals. *p < 0.001 compared with control mice by ANOVA. Abbreviations: FC, frontal cortex;PC, parietal cortex; ST, striate cortex; CP, caudate putamen; CC, corpus callosum; CA1, CA1 horn of hippocampus; CA2, CA2 horn of hippocampus; CA3, CA3 horn of hippocampus;DG, dentate gyrus; IC, inferior colliculus; SC, superior colliculus; DT, dorsal thalamus; VT, ventral thalamus; PT, ventroposterior thalamus; SN, substantia nigra; GP, globus pallidus; AG, amygdala; TN, trigeminal nucleus; MG, medial geniculate nucleus; HD, horizontal diagonal band; MS, medial septum; HY, hypothalamus; CE, cerebellum.
Densities of [3H]AFDX 384 binding sites in CD-1 mice were highest in caudate/putamen followed by cerebral cortex, superior colliculi, diagonal band, and medial septum with lowest densities of binding sites being observed in cerebellum (Figs. 3 and4). In general, congenital OTC deficiency resulted in decreased densities of the M2 subtype of muscarinic cholinergic sites in spf mouse brain with regional differences in the magnitude of these decreases. In the spf mutant mouse there was a significant decrease of [3H]AFDX 384 binding sites in all cortical areas as well as in caudate/putamen, medial septum, diagonal band, CA1 and CA2 regions of hippocampus, anterodorsal thalamus, and superior colliculi compared with that of CD-1 controls(Fig. 3). There were no significant changes in the densities of these binding sites in other brain areas.
Quantitative autoradiographic analysis of[3H]AFDX 384 binding sites in selected brain regions of CD-1 control and spf mutant mice. Values are expressed as mean ± SEM from duplicate sections of five different animals. Abbreviations as inFigure 1.
DISCUSSION
Results of the present study demonstrate region-selective decreases in densities of binding sites for [3H]AFDX-384 in the brains of congenitally OTC-deficient spf mice. [3H]AFDX 384 is a radioligand with high selectivity for the M2 subtype of muscarinic cholinergic receptor(15, 16). Loss of M2 sites in OTC-deficient mouse brain was particularly apparent throughout the cerebral cortex, caudate nucleus, and septal area as well as in the diagonal band, CA1 and CA3 areas of hippocampus, anterodorsal thalamus, and superior colliculus. The previous report that M2 muscarinic agonists, including AFDX-384, enhance acetylcholine release from rat brain slices via inhibition of a negative autoreceptor(20) strongly suggests that these compounds bind to presynaptic M2 receptors. This proposal is strengthened by the results of studies of the regional distribution of the presynaptic cholinergic nerve terminal enzyme ChAT which generally shows a good regional correlation with the distribution of M2 binding sites(21). Furthermore, partial destruction of extrinsic cholinergic inputs to cerebral cortex results in a 50-60% reduction of both ChAT activity and of muscarinic M2 receptor densities(22). A previous report described significantly reduced activities of ChAT as well as reduced ChAT immunolabeling in the cerebral cortex, medial septum, and the diagonal band in the brains ofspf mutant mice with congenital OTC deficiency(12). These findings, together with those of the present study, strongly suggest that loss of cholinergic neurons is an important feature of congenital OTC deficiency in the mouse. Neuropathologic studies in both human and mouse OTC deficiency have consistently revealed substantial neuronal loss in cerebral cortex, basal ganglia, and thalamus with relative sparing of brainstem and cerebellar structures(3, 23, 24). This pattern of neuronal loss parallels the reduced activities of ChAT in a previous study(12) as well as the loss of muscarinic M2 binding sites in OTC deficiency observed in the present study.
In contrast to the M2 subtype of muscarinic cholinergic binding sites, binding of the selective M1 subtype ligand [3H]PZ was significantly increased in the cerebral cortical, thalamic, and subthalamic structures of OTC-deficient mice. Previous studies demonstrate that[3H]PZ binds with high selectivity to muscarinic M1 receptors in the cerebral cortex, hippocampus, and caudate nucleus(25), and studies of the regional distribution of muscarinic receptor mRNAs suggest that the M1 subtype of receptors is predominantly localized postsynaptically in the cerebral cortex and hippocampus, terminal fields from basal forebrain cholinergic neurons(26). The most likely explanation for the increased M1 sites in parietal and striatal cortex, CA1 of hippocampus, as well as in dorsal and ventroposterior thalamus of OTC-deficient mice is the up-regulation of these sites after the loss of the presynaptic neuron. M1 receptor up-regulation has previously been proposed to explain the increases in M1 binding sites in hippocampus and caudate nucleus in Alzheimer's disease(27). Furthermore, like congenital OTC deficiency, cerebral cortex from patients with Alzheimer's disease as well as from rats with experimental denervation of cerebral cortex manifests significant cholinergic neuronal loss as evidenced by reductions in activity of ChAT and concomitant reductions of muscarinic M2 sites(28). It has been proposed that cholinergic deficits in patients with Alzheimer's disease could result from the retrograde degeneration of cerebral cortical and hippocampal innervation(29). Basal forebrain cholinergic neuronal loss, therefore, offers a possible explanation for the severe cognitive dysfunction characteristic of both Alzheimer's disease and congenital OTC deficiency.
Cholinergic dysfunction and, ultimately, cholinergic neuronal loss in brain in OTC deficiency are consistent with previously established neurochemical findings in this syndrome. Significant reductions of acetyl-CoA, the substrate for acetyl-choline synthesis, have been reported in the brains of OTC-deficient mice(30) and sustained hyperammonemia, a major metabolic consequence of OTC deficiency, results in significant reductions in acetylcholine synthesis in the brain(31). However, the correlation between degree of cerebral damage and duration of hyperammonemia, rather than peak plasma ammonia levels, in congenital urea cycle diseases including OTC deficiency(32), suggests that a metabolite of ammonia rather than ammonia per se is responsible for the damage. Alternatively (or additionally), neuronal loss in OTC deficiency could conceivably result from exposure to neurotoxins generatedin situ in brain in this disorder. In this regard, a recent study demonstrated increased brain concentrations of quinolinic acid in cerebrospinal fluid of children with OTC deficiency(33). This observation is particularly noteworthy because quinolinic acid is a potent neurotoxin. Intrastriatal injections of quinolinic acid result in a dose-dependent loss of activity of ChAT and addition of this toxin in vitro inhibits the growth of neostriatal cholinergic neurons(34). Similar mechanisms could be implicated in the pathogenesis of the muscarinic cholinergic lesion in congenital OTC deficiency.
Abbreviations
- OTC:
-
ornithine transcarbamylase
- ChAT:
-
choline acetyltransferase
- PZ:
-
pirenzepine
- spf :
-
sparse-fur
References
Cathelineau L 1979 L'hyperammoniemie dans la pathologie pediatrique. Arch Fr Pediatr 36: 724–735
Kornfeld M, Woodlin BM, Papile L, Davis LE, Bernard LR 1985 Neuropathology of ornithine carbamyl transferase deficiency. Acta Neuropathol 65: 261–264
Dolman CL, Clasen RA, Dorovini-Zis K 1988 Severe cerebral damage in ornithine transcarbamylase deficiency. Clin Neuropathol 7: 10–15
Levin B, Abraham JM, Oberholzer VG, Burgess EA 1969 Hyperammonemia: a deficiency of liver ornithine transcarbamylase. Arch Dis Child 44: 152–161
DeMars R, LeVan SL, Trend BL, Russell LB 1976 Abnormal ornithine carbamyl-transferase in mice having the sparse-fur mutation. Proc Natl Acad Sci USA 73: 1693–1697
Qureshi IA, Letarte J, Ouellet R 1979 Ornithine transcarbamylase deficiency in mutant mice. 1. Studies on the characterization of enzyme defect and suitability as animal model of human disease. Pediatr Res 13: 807–811
Batshaw ML, Hyman SL, Coyle JT, Robinson MB, Qureshi IA, Mellits ED, Quaskey S 1988 Effect of sodium benzoate and sodium phenylacetate on brain serotonin turnover in the ornithine transcarbamylase deficient sparse-fur mouse. Pediatr Res 23: 368–374
Ratnakumari L, Qureshi IA, Butterworth RF 1992 Effects of congenital hyperammonemia on the cerebral and hepatic levels of the intermediates of energy metabolism in spf mice. Biochem Biophys Res Commun 184: 745–751
Robinson MB, Anegawa NJ, Gorry E, Qureshi IA, Coyle JT, Lucki I, Batshaw ML 1992 Brain serotonin2 and serotonin1A receptors are altered in the congenitally hyperammonemic sparse-fur mouse. J Neurochem 58: 1016–1022
Raghavendra Rao VL, Qureshi IA, Butterworth RF 1994 Activities of monoamine oxidase-A and -B are altered in the brains of congenitally hyperammonemic sparse-fur (spf) mice. Neurosci Lett 170: 27–30
Ratnakumari L, Qureshi IA, Butterworth RF 1994 Regional amino acid neurotransmitter changes in brains of spf/Y mice with congenital ornithine transcarbamylase deficiency. Metab Brain Dis 9: 43–51
Ratnakumari L, Qureshi IA, Butterworth RF 1994 Evidence for cholinergic neuronal loss in brain in congenital ornithine transcarbamylase deficiency. Neurosci Lett 178: 63–65
Ratnakumari L, Qureshi IA, Butterworth RF 1995 Developmental deficiency of the cholinergic system in congenitally hyperammonemic spf mice: effect of acetyl-L-carnitine. J Pharmacol Exp Ther 274: 437–443
Fitzgerald BB, Costa LG 1992 Modulation of M1 and M2 muscarinic receptor subtypes following repeated organophosphate exposure in rats. Toxicol Appl Pharmacol 117: 122–125
Entzeroth M, Mayer N 1990 Labeling of rat heart muscarinic receptors using the new M2 selective antagonist[3H]AFDX 384. Biochem Pharmacol 40: 1674–1676
Castoldi AF, Fitzgerald B, Manzo L, Tonini M, Costa LG 1991 Muscarinic M2 receptors in rat brain labeled with [3H]AF-DX 384. Res Commun Chem Pathol Pharmacol 74: 371–374
Quirion R, Araujo D, Regenold Q, Boksa P 1989 Characterization and quantitative autoradiographic distribution of[3H]acetylcholine muscarinic receptors in mammalian brain. Neuroscience 29: 271–289
Sidman RL, Angevine JB, Pierce TE 1971 Atlas of the Mouse Brain and Spinal Cord. Harvard University Press, Cambridge, MA
Schwab C, Bruckner G, Rothe T, Castellano C, Oliverio A 1992 Autoradiography of muscarinic cholinergic receptors in cortical and subcortical brain regions of C57BL/6 and DBA/2 mice. Neurochem Res 17: 1057–1062
Lapchak PA, Araujo DM, Quirion R, Collier B 1989 Binding sites for [3H]AF-DX 116 and effect of AF-DX 116 on endogenous acetylcholine release from rat brain slices. Brain Res 496: 285–294
Regenold W, Araujo DM, Quirion R 1989 Quantitative autoradiographic distribution of [3H]AF-DX 116 muscarinic M2 receptor binding sites in rat brain. Synapse 4: 115–125
Johnston MV, McKinney M, Coyle JT 1981 Neocortical cholinergic innervation: a description of extrinsic and intrinsic components in the rat. Exp Brain Res 43: 159–172
Harding BN, Leonard JV, Erdohazi M 1984 Ornithine carbamyltransferase deficiency. Pediatrics 141: 215–220
Hopkins KJ, Robinson MB, Batshaw ML, Oster-Granite ML 1994 Neuropathologic changes associated with ornithine transcarbamylase deficiency in mice. Soc Neurosci Abstr 343: 14
Mash DC, Potter LT 1986 Autoradiographic localization of M1 and M2 muscarinic receptors in the rat brain. Neuroscience 19: 551–564
Weiner DM, Brann MR 1989 Distribution of m1-m5 muscarinic receptor mRNAs in rat brain. FEBS Lett 253: 207–213
Araujo DM, Lapchak PA, Robitaille Y, Gauthier S, Quirion R 1988 Differential alteration of various cholinergic markers in cortical and subcortical regions of human brain in Alzheimer's disease. J Neurochem 50: 1914–1923
Mash DC, Flynn DD, Potter LT 1985 Loss of M2 muscarine receptors in the cerebral cortex in Alzheimer's disease and experimental cholinergic denervation. Science 228: 1115–1117
Perry EK, Curtis M, Dick DJ, Candy JM, Atack JR, Bloxham CA, Blessed G, Fairbairn A, Tomlinson BE, Perry RH 1985 Cholinergic correlates of cognitive impairment in Parkinson's disease: comparisons with Alzheimer's disease. J Neurol Neurosurg Psychiatry 48: 413–421
Ratnakumari L, Qureshi IA, Butterworth RF 1993 Effect of sodium benzoate on cerebral and hepatic energy metabolites in spf mice with congenital hyperammonemia. Biochem Pharmacol 45: 137–146
Parker TH, Roberts RK, Vorhees CV, Schmidt DE, Schenker S 1977 The effect of acute and subacute ammonia intoxication on regional cerebral acetylcholine levels in rats. Biochem Med 18: 235–244
Msall M, Monahan PS, Chapanis N, Batshaw ML 1988 Cognitive development in children with inborn errors of urea synthesis. Acta Paediatr Jpn 30: 435–441
Batshaw ML, Robinson MB, Hyland K, Djali S, Heyes MP 1993 Quinolinic acid in children with congenital hyperammonemia. Ann Neurol 34: 676–681
Alberch J, Perez-Navarro E, Calvao NE, Marssal J 1993 Trophic factors protect neostriatal cholinergic neurons against quinolinic acid lesions. Soc Neurosci Abstr 19: 276.12
Acknowledgements
The authors thank D. D. Roy for secretarial assistance.
Author information
Authors and Affiliations
Additional information
Supported by grants P.G.11118 (to R. F. B.) and MT-9124 (to I. A. Q.) from The Medical Research Council of Canada.
Rights and permissions
About this article
Cite this article
Ratnakumari, L., Qureshi, I. & Butterworth, R. Central Muscarinic Cholinergic M1 and M2 Receptor Changes in Congenital Ornithine Transcarbamylase Deficiency. Pediatr Res 40, 25–28 (1996). https://doi.org/10.1203/00006450-199607000-00005
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199607000-00005
This article is cited by
-
Impaired novelty acquisition and synaptic plasticity in congenital hyperammonemia caused by hepatic glutamine synthetase deficiency
Scientific Reports (2017)
-
Ammonia toxicity to the brain
Journal of Inherited Metabolic Disease (2013)
-
Evidence for forebrain cholinergic neuronal loss in congenital ornithine transcarbamylase deficiency
Metabolic Brain Disease (2000)
-
Ornithine transcarbamylase deficiency: Pathogenesis of the cerebral disorder and new prospects for therapy
Metabolic Brain Disease (1997)