Abstract
Isolated idiopathic growth hormone deficiency (GHD) and idiopathic short stature (ISS) can be difficult to distinguish, but the therapeutical consequences are different. In this report the data on final height of untreated and treated children with GHD and ISS are reviewed. Untreated GH-deficient individuals who underwent spontaneous puberty (22 male, 14 female patients) reached a mean final height of 4.7 SD (range 3.9 to 6.0) below the population's mean. If puberty was induced (19 male patients), mean final height SD score (SDS) was -3.1. Traditional regimens of GH administration (2-4 injections/wk) in 236 children (184 boys, 52 girls) with GHD and spontaneous puberty resulted in a final height SDS of -2.8 (range -1.5 to -4.7). In 190 children in whom puberty was induced (139 boys, 51 girls) mean final height was -1.6 (range - -1.1 to -2.4). The mean gain in final height SDS is therefore estimated at 1.5-2.0 in average cases, and 3.5 in extreme cases. Preliminary data suggest that on present regimens mean final height may approach target height. In untreated boys with ISS the mean final height was 2-5 cm lower than that predicted before puberty, whereas in girls it was almost equal to the prediction. After GH treatment the mean final height was 0.4-3.0 cm higher than the predicted adult height, which results in an average net gain in final height SDS of approximately 0.5-0.8 (3-5 cm).
Similar content being viewed by others
Main
The diagnosis of severe GHD is usually easy by the combination of a classical phenotype (truncal fat deposition, fat dimpling, and frontal bossing), persistent growth failure, delayed bone age, and a low GH output. However, in the diagnostic work-up of an asymptomatic child with growth retardation, it is often difficult to prove or disprove the diagnosis of isolated idiopathic GHD. This is caused by the fact that in none of the classical characteristics a clear separating line can be drawn between the findings in GHD and in the healthy population. This is particularly the case with respect to the assessment of pituitary GH secretion. None of the parameters of GH secretion, be it the maximum plasma GH level at a standard provocation test, the spontaneous secretion over 12-24 h measured in a plasma GH profile, or plasma IGF-I and IGF-binding protein 3 levels, shows a strong discriminative power(1–4). This situation is even worsened by the wide intraindividual variation of all tests, and the wide interassay variation of plasma GH concentration(5, 6). The problem in diagnosing GHD is further illustrated by the observation that retesting the GH secretion after completion of GH therapy leads to normal results in 21-26% of cases with idiopathic GHD(7, 8).
If the presence of GHD is felt unlikely by a combination of clinical and laboratory findings, and if pathologic findings suggestive for other disorders are absent, the diagnostic label of ISS can be applied. In a recent classification ISS is subclassified in familial short stature, constitutional delay, the combination of these two, and an unclassifiable subgroup(9). These subgroups have been distinguished on the basis of parental height, height velocity, bone age delay, and the age at onset of puberty. Generally speaking, familial short stature is described as being characterized by short parents and little bone age delay, in contrast to constitutional delay of growth and adolescence, in which bone age delay and late onset of puberty are typical, often associated with a positive family history of delayed pubertal development. Combinations of both conditions are frequent and lead to more severe growth retardation. It should be noted, however, that there is no consensus among investigators about the definitions of these subgroups and that it has even been argued that any subdivision of this heterogeneous group is arbitary. To complicate the nomenclature even further, some of these children may have a low spontaneous GH secretion, as measured by a 24-h profile, in contrast to normal plasma GH responses to provocative testing, a condition termed “neurosecretory dysfunction”(10, 11).
Although in many cases, even after extensive testing, insufficient certainty can be obtained about the diagnosis of isolated GHD or ISS, the therapeutical strategy for both conditions is completely different. For more than three decades(12) the administration of GH has been widely accepted for GHD patients, but such treatment in ISS is highly controversial(13–19). Still, experimental data on the natural history of both conditions are scarce, as well as data on the long-term response to GH treatment.
In this report the published data on the natural history in terms of growth of untreated children with GHD and ISS are reviewed, with emphasis on final height. Furthermore, the long-term effect of GH therapy in both conditions is summarized. All height data are presented as SDS, also if, in the original publication, height data were presented in centimeters. In these cases the transformation was based on British references(20). Plasma GH levels were all converted, if applicable, to micrograms/L (1 μg/L= 2 mU/L).
FINAL HEIGHT IN UNTREATED CHILDREN WITH GHD
In the regulation of human growth, GH and the GH-dependent growth factors(particularly IGF-I) play a central role, but other factors are also relevant, such as sex hormones, thyroxine, and insulin. In the context of this review, which is focused on final height, the role of sex hormones is of particular importance. Testosterone appears to exert its full growth-promoting action only in the presence of normal endogenous GH secretion or with sufficient GH replacement(21), although the pubertal growth spurt is mediated in part by direct effects of sex steroids in the growth plate(22). From clinical observations in patients with hypogonadism and precocious puberty it can be concluded that an early presence of sex steroids accelerates epiphyseal maturation in the long bones, whereas in the absence of sex steroids epiphyseal maturation is delayed, which allows the legs more time to grow. The epiphyseal plates of the spine appear relatively insensitive to sex steroids.
It can therefore be expected that final height of untreated GHD individuals is dependent on the presence or absence of other pituitary deficiencies, particularly gonadotropin deficiency, and in fact most studies have shown this. Therefore the data on final height will be presented here in separate paragraphs.
Spontaneous puberty. Data on final height of untreated individuals with isolated GHD are extremely scarce. The largest group was published in 1968 by Rimoin et al.(23), who reported final heights of 16 (male:female, 8:8) subjects who were 27 y or older and were diagnosed as having “sexual ateliosis,” defined by clinical signs of GHD and the presence of spontaneous puberty. The cases were detected on the basis of recurrent hypoglycemic episodes or on the basis of genetic occurrence. Final height was 134.0 and 127.9 cm for men and women, respectively, which corresponds to -6.1 and -5.9 SDS according to the British references(20). It is likely, by the selection procedure, that the patients described in this report represent the extreme end of the spectrum of isolated GHD, although one should note that the biochemical methods to define GHD had not been developed at that time.
Ranke(24) found a mean (SD) height of 145.8 (4.3) cm in 8 male and 133.7 (7.3) cm in 6 female subjects, which is approximately 4.8 SD below the population's mean. Van der Werff ten Bosch and Bot(25) reported data on four patients with isolated GHD. Puberty started between 13 and 22 y at a height SDS of -4.4 and their mean final height SDS was -3.9 (range -2.3 to -5.0). On the average, final height was 1 cm higher than its prediction at onset of puberty. Personal observations on two brothers with the dominant form of isolated GHD revealed heights of 142 cm (-5.3 SDS). Thus, the available evidence from these 22 male and 14 female subjects suggests that a severe isolated GHD leads to an average final height SDS of -4.7 with a range of -3.9 to -6.1 in the four available studies. No data are available on final height of individuals with partial forms of isolated GHD.
Induced puberty. With respect to patients with multiple pituitary deficiencies, the only available data are those of 19 male individuals in the study of Van der Werff ten Bosch and Bot(25). All patients were supplemented with hydrocortisone, thyroxine, and sex steroids. Androgen treatment started at a mean age of 15.6 y. The mean pubertal growth period was 8.7 y, during which height increased by 6.5-37.0 cm (mean 20.4 cm). Their final height was -3.1 SDS. These results indicate that final height in patients with GHD combined with hypogonadism is better than in patients with isolated GHD. This could be due to the late start of pubertal induction, the long period of subtotal androgen substitution, or a combination of these. The observation that the mean final height was 7 cm lower than the prediction at the onset of puberty can be explained by the extreme bone age delay at that time.
FINAL HEIGHT OF GHD CHILDREN TREATED WITH GH
Table 1 summarizes the data of nine reports on the effect of GH treatment on final height according to sex and the presence of additional hypogonadism. In all studies, except the KIGS study in which the frequency varied between 2 and 7 injections/wk, the injection frequency was 2-4 times/wk and the GH dosage was variable and not always adapted to body mass. Such therapeutical regimens are nowadays considered inadequate(26–28). The only study available which presents data of patients treated with the now widely accepted regimen, a weekly dosage of 14-21 IU/m2/wk divided into daily injections(29), is discussed separately.
In several reports, subjects were not subdivided into the four categories based on sex and presence of gonadotropin deficiency(30, 31), and these were therefore not included in the table. However, the numerical data appear perfectly in line with the other reports.
Spontaneous puberty. In the nationwide studies in the United Kingdom, Finland, and the Netherlands mean final height SDS of male patients was remarkably similar: -2.1, -2.4, and -2.3, respectively. In contrast, the results in Japan were considerably lower (-3.4), whereas the recent data from the international database showed a final height of -1.3. In this last study the age and height deficit at the start of therapy were clearly lower than in the other studies, whereas the dosage and injection frequency varied widely.
The mean height SDS in male subjects from all studies with a low injection frequency was -2.8, which is approximately 2 SD more than observed in the 22 untreated patients. When final height is compared with the predicted adult height at start, both are approximately equal in the study with a relatively low dosage, whereas in the study using a higher dosage(32) an increment of 7.8 cm was observed. The relatively small difference between final height and the initial prediction may be due to a shortening of the duration of puberty(33).
The disadvantage of group analyses is that the view on the individual response may get blurred. Therefore, an anecdotal observation can sometimes provide relevant additional information. We had the opportunity to treat a boy with the dominant form of isolated GHD from the age of 2 y and to compare his height with that of his untreated father. During the first 10 y of the treatment period GH was given in a weekly dosage of 8 IU divided into 2 intramuscular injections. Later, the same dosage was divided into 4 s.c. injections for 3 y, followed by 14 IU/m2/wk in daily injections. His final height was 170 cm (-1.8 SDS), 28 cm (3.5 SDS) more than his untreated father (Drop, personal communication), showing that in complete GHD the benefit is much greater than would be deducted from a group analysis.
In all studies except the Japanese, the results in terms of final height of female subjects with spontaneous puberty were inferior to those of male subjects. This appears to be caused by the fact that most girls enter puberty at a normal age(34–36). In the study of Joss et al.(37), where both sexes were combined, five patients with partial GHD (two male and three female) reached an average height SDS of -3.3, whereas their height SDS at the start of treatment was -5.2.
There is now preliminary evidence that the present therapeutical regimen can further improve the results. In the recent study on patients treated by daily injections(29), 16 patients (boys and girls) had an isolated GHD with a GH peak of <5 μg/L. Their mean height SDS at start was -2.6 and at the end of therapy -1.0, whereas their target height SDS was -0.8. The 12 patients with partial GHD (GH peak 5-10 μg/L) started treatment at a height SDS of -2.9 and ended up at -1.2, whereas their target height was -0.6. A similar initial and final height was found in the KIGS study(38). The higher efficacy of daily GH treatment in a dosage adapted to body size in comparison to a standard dosage divided into 2-3 injections was also shown in a recent study by our group. Over 4 y of therapy, the height SDS increment was 1.31 ± 0.81 on the old regimen and 2.02 ± 1.01 SDS on the present one(39).
Induced puberty. The average reported final height SDS of male and female subjects with induced puberty on traditional regimens is -1.6(range -1.1 to -2.4), clearly better than in patients with spontaneous puberty(see Table 1). For example, in our recent study(40), the final height SDS of 74 patients (male/female = 53/21) with spontaneous puberty was -2.4, compared with -1.8 in 62(male/female = 41/21) patients with induced puberty, although the initial height SDS was similar. In the Japanese and British studies(32, 41) the differences were even greater.
When the data of the European nationwide studies on final height after GH treatment are compared with those of the untreated Dutch patients (-3.1 SDS)(25), the effect of GH treatment can be estimated on 1.5 SD. This is confirmed if one considers that in untreated patients final height falls short to the prediction by 7 cm, whereas on treatment the prediction is generally reached, and even surpassed by 11 cm in the studies using a relatively high dosage(32, 37). A lower estimation of height gain (0.5 SD) was made by Van der Werff ten Bosch and Bot(42), but in this study patients were described who started treatment at a relatively advanced age and were treated with a low dosage divided into 2 injections/wk.
Girls showed similar values with respect to final height as the boys, except for the 7 girls who started at an early age in the KIGS study(38) and reached a final height SDS of -0.5. In the study in which daily GH treatment was given(29), 8 patients with multiple pituitary hormone deficiency started GH therapy at a height SDS of -2.1 and had a final height of -0.4, close to their target height.
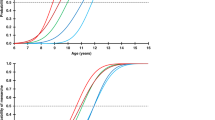
Factors influencing final height. Besides the presence of an additional gonadotropin deficiency, also other factors appear to affect final height. In several studies(38, 40, 43, 44) it was shown that height SDS at the start of therapy and height SDS at the onset of puberty were significantly correlated with final height, as well as mid-parental height (target height) SDS. The duration of puberty also showed a positive correlation with final height. The influence of height SDS at the start of therapy is also seen if the various studies summarized inTable 1 are compared. This implies that it is important to start GH therapy as early as possible.
Theoretically, it would be expected that final height would be affected by the GH dosage. In fact, a positive dose-response relationship has been observed during the first years of treatment, but a higher dosage also accelerated, although to a lesser extent, skeletal maturation(33, 45, 46). However, a positive influence of GH dosage on final height has not yet been shown.
As discussed above, the injection frequency is also important. In the KIGS study(38) the mean frequency of injections was positively correlated with final height. The results of the most recent study(29) suggest that a regimen of daily injections can bring final height close to target height.
The clear difference in final height between children with isolated GHD and those with induced puberty led Hibi et al.(41) to treat 24 children with isolated GHD and early puberty with gonadal suppression treatment (cyproterone acetate and/or medroxyprogesterone). After a mean period of 4.3 y, final height in this group was -2.2 SDS (17 boys) and -1.9 SDS (7 girls), substantially better than the patients who did not undergo gonadal suppression. However, patients in the unsuppressed group started GH treatment 2-3 y later than the suppressed group, which may have confounded the results. Along the same line, GnRH analogues have been added to GH therapy for a few years(47–49), but the effect on final height is not yet known.
The effect of the cause of GHD on the efficacy of GH therapy, in terms of final height, has been investigated in detail in British patients. Three reports presented data on 55 children with idiopathic GHD(32), 30 children with GHD after craniopharyngioma(50), and 27 children with a brain tumor other than craniopharyngioma(51). The data of the first two reports are summarized in Table 1. In the idiopathic group no differences were found between the height gain of boys and girls, nor between the height gain of children with partial (maximal GH response 3.5-7.5μg/L) or total GHD (response below 3.5 μg/L). Final height in children with craniopharyngioma was similar to that of idiopathic patients with gonadotropin deficiency. The results of GHD patients due to other brain tumors(16 boys, 11 girls) were also similar to that of idiopathic patients (final height of patients with spontaneous puberty -2.5 and patients with induced puberty -1.6). In all three groups of patients with additional gonadotropin deficiency, the body build was eunuchoid, with a mean sitting height between-2.8 and -2.9 and a leg length between -0.3 and +0.7. Less favorable results were reported of GH therapy in children who received cranial or craniospinal irradiation. Mean final height SDS was -2.1 and -1.7 after cranial irradiation for leukemia and facial tumors and -3.7 after craniospinal irradiation for medulloblastoma(52).
FINAL HEIGHT IN UNTREATED CHILDREN WITH ISS
Table 2 summarizes the results of several reports on the natural history in terms of growth in children with ISS. Although different definitions were used, there is a striking similarity among the various studies in terms of the relation between final height and its prediction before puberty. Average final height in boys was a few centimeters below the initial prediction, ranging between 2 and 5 cm, but for the individual patient the accuracy of the prediction was poor. A systematic inaccuracy is apparent if bone age is delayed by 2 y or more: this leads to significant overestimation of the predicted height(53). In girls mean final height was almost identical to its prediction. There were large differences with respect to the changes in height SDS between the studies, ranging from 0.5 to 1.9 SDS. This is probably caused by the differences among the studies with respect to the inclusion criteria: children with classical constitutional delay of growth and adolescence show a greater change in height SDS than children with classical forms of familial short stature.
FINAL HEIGHT OF CHILDREN WITH ISS AFTER GH THERAPY
Over the last years a number of studies have been published on the effect of GH therapy on growth over 1-3 y(54–59), generally indicating an increased growth velocity paralleled by an acceleration of skeletal maturation. So far, final height data are available only from four prospective studies(60–63) and from an analysis of an international collaborative study(64). Data from these studies and from one report on 5-6-y results are summarized in Table 3.
It is remarkable that all studies on this subject have provided similar data: average final height is only a few centimeters higher than the initial prediction, ranging from 0.4 to 3.0 cm. If one takes into account that untreated children with ISS fall a few centimeters short of their prediction, particularly boys (see above), the net benefit of GH treatment can be estimated on 3-5 cm.
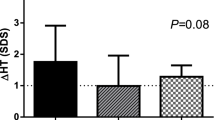
In our study(61) 27 prepubertal children with ISS were treated with recombinant GH in an initial dosage of 2 IU/m2 body surface/d s.c., which was doubled either after the first year if the height velocity increment was less than 2 cm/y, or thereafter if height velocity fell below the median velocity for bone age. Growth and maturation of the 21 remaining patients were compared with those of an untreated control group with ISS and a group of GH treated children with isolated GHD. In 9 patients still on treatment, mean height SDS increased from -3.9 to -2.5 and -2.3 after 4 and 6 y, whereas in matched controls height SDS did not change. In the GHD group height SDS increased from -3.9 to -1.8 after 4 y, significantly more than in the ISS group. Bone maturation was accelerated in both groups (5.4 and 5.0“years” per year, respectively), which led to no significant change in height SDS for bone age and predicted adult height. Final height has now been reached by 12 patients. Their average height and height gain was similar to untreated controls, but there was a wide interindividual variation. A low integrated GH concentration over 24 h, a low GH peak to provocative stimuli, and little bone age delay predicted a favorable outcome. In children with a great initial bone age delay, skeletal maturation advanced relatively fast.
There is still uncertainty about the effect of GH on the onset and duration of puberty. In our study, the age at onset of puberty was 13.7 ± 1.2 y in boys and 11.7 ± 0.8 y in girls, which is delayed compared with the general population(65, 66). However, due to the lack of a prospective control group it is unknown whether GH advances puberty in ISS. The mean duration of puberty, defined as the interval between Tanner stage 2 and 4, was relatively short in boys: 1.4 ± 0.6 yversus 1.9 in a reference population(66). A similar shortening of the pubertal period was described by Hopwood et al.(56). In a prospective study, however, no differences were found in age at onset of puberty, duration of puberty, prepubertal height gain, and pubertal height gain(60).
The effect of GH in this dosage range on the growth pattern of children with ISS can thus be summarized as a moderate acceleration of growth which is accompanied by a similar acceleration of skeletal maturation. The acceleration of skeletal maturation is observed before puberty as well as during puberty. This leads to a mean final height which is just above the initial prediction, whereas without treatment final height stays just below its prediction. Preliminary data would suggest that a higher dosage could lead to a better result(67), but data on final height have not yet been reported.
THE BENEFIT OF GH TREATMENT IN CHILDREN WITH GHD AND ISS
The benefit of GH therapy in the various patient groups should not only be seen as restricted to the issue of final height. For all patients the impact of therapy is much greater, if one takes into account the whole period of childhood and adolescence, and includes somatic as well as psychologic aspects. However, the impact is different for the various groups.
Unavailability of GH treatment for male subjects with complete or almost complete isolated GHD leads to severe short stature, associated with truncal adiposity and an immature physical appearance during childhood; a very delayed pubertal development with all its negative psychosocial consequences; and an average final height SDS of -4 down to -6. There is no doubt that this constitutes not only a severe handicap during childhood and adolescence, but that it remains a handicap for the whole life of the patient. GH treatment, if started early and if given in an appropriate regimen of daily injections, leads to a rapid catch-up growth in childhood up to approximately -1.0 SDS(68), and a stable height SDS thereafter. There are no data on the timing of puberty in such cases, but an average final height of-1.0 SDS appears possible. GH therapy in these patients can thus correct almost all negative consequences of the disorder.
In patients with multiple pituitary deficiencies, particularly gonadotropin deficiency, the impact of GH therapy is perhaps even more dramatic. Unavailability of GH therapy, as is still the case in many countries in the world, would not only lead to severe short stature, but would also bring the physician in a difficult dilemma: postponing androgen or estrogen substitution might lead to a somewhat higher final height, but deprives the patient of going through puberty at the appropriate age. To illustrate this, one should note that the age at onset of androgen therapy in the Dutch study(25) ranged from 11 to 30 y, with 16 out of 19 patients starting at an age of more than 14 y. The psychologic consequences of this are substantial. In contrast, adequate and timely GH therapy would normalize body stature during childhood, which would remove any hesitation to start sex steroid substitution therapy later than 13-14 y.
The situation with respect to children with ISS is different mainly with respect to the natural history. The general growth pattern during childhood of these children is parallel to, but up to 10-15 cm below, the 3rd percentile. During this phase some of these children experience psychologic problems(69), although such changes were not found in 7-9-y-old children(70). As a group, puberty starts approximately 2 y later than in the general population, which further diminishes height in comparison to controls and adds the psychologic problems of delayed puberty to those of short stature. Every clinician knows that this can cause serious problems to the affected teenager. However, after the onset of puberty the difference in height with that of peers diminishes rapidly, and final height reaches the normal distribution in a substantial percentage of patients, particularly in patients with constitutional delay of growth and adolescence. If GH therapy is started in childhood, height velocity increases, particularly over the first years, so that height deficit is diminished in late childhood and as a teenager. Also during adolescence height is closer to that of age-mates. Clinically, this appears important for the youngsters, but the psychologic benefit has not yet been proved in controled studies. Final height is only a few centimeters higher than it would have been otherwise. The“gain” of therapy is thus that the patient is less different from his peers in terms of height in late childhood and adolescence, at a“cost” of daily injections and a substantial amount of medical consumption and community funds.
Although it is thus obvious that the cost-benefit ratio is quite different between the classical forms of GHD and ISS, the key question remains how a partial GHD can be distinguished from ISS. In our study of children with so-called “normal” results on the GH provocation tests(61) the 24-h serum GH profile and the growth response to GH treatment were extremely variable. The response ranged from the typical result which would be expected in GHD-a substantial improvement of height SDS and a higher final height than the initial prediction-to even a loss of height potential. The integrated GH concentration correlated negatively with the response, although the predictive power was insufficient to enable its use on an individual basis. There is an urgent need to refine the clinical and laboratory methods to quantify the degree of GH insufficiency versus GH sensitivity, to obtain tests that can better discriminate between good and poor responders than our present tools. On one hand, this would prevent GH therapy being given to children who would not benefit sufficiently, saving a lot of personal displeasure and community funds; on the other hand it would ensure that GH is allowed to children who would benefit substantially.
Abbreviations
- GH:
-
growth hormone
- GHD:
-
growth hormone deficiency
- SDS:
-
SD score
- ISS:
-
idiopathic short stature
- KIGS:
-
Kabi Pharmacia International Growth Study
References
Rose SR, Ross JL, Uriarte M, Barnes KM, Cassorla FG, Cutler Jr GB 1988 The advantage of measuring stimulated as compared with spontaneous growth hormone levels in the diagnosis of growth hormone deficiency. N Engl J Med 319: 201–207
Albertsson-Wikland K, Rosberg S 1988 Analysis of 24-hour Growth Hormone profiles in children: relation to growth. J Clin Endocrinol Metab 67: 493–500
Phillip M, Chalew SA, Kowarski AA, Stene MA 1993 Plasma IGFBP-3 and its relationship with quantitative growth hormone secretion in short children. Clin Endocrinol 39: 427–432
Smith WJ, Nam TJ, Underwood LE, Busby WH 1993 Use of insulin-like growth factor-binding protein-2 (IGFBP-2), IGFBP-3, and IGF-I for assessing growth hormone status in short children. J Clin Endocrinol Metab 77: 1294–1299
Rochicchioli P, Pienkowski C, Tauber MT, Uboldi F 1991 Association of pharmacological tests and study of 24-hour growth hormone secretion in the investigation of growth retardation in children: analysis of 257 tests. Horm Res 35: 70–75
Georges P, Roger M, Carton F, Garnier P, Job JC 1990 Comparison of immunoreactivity of five pharmaceutical hGH preparations and WHO standard (66/217) by means of two monoclonal sandwich assays. Horm Res 33: S3–18
Cacciari E, Tassoni P, Parisi G, Pirazzoli P, Zucchini S, Mandini M, Cicognani A, Balsamo A 1992 Pitfalls in diagnosing impaired growth hormone (GH) secretion: retesting after replacement therapy of 63 patients defined as GH deficient. J Clin Endocrinol Metab 74: 1284–1289
Clayton PE, Price DA, Shalet SM 1987 Growth hormone state after completion of treatment with growth hormone. Arch Dis Child 62: 222–226
Ranke MB 1991 The Kabi Pharmacia International Growth Study: Aetiology classification list with comments. Acta Paediatr Scand Suppl 379: 87–92
Spiliotis BE, August SP, Hung W, Sonis W, Mendelson W, Bercu BB 1984 Growth hormone neurosecretory dysfunction. A treatable cause of short stature. JAMA 251: 2223–2230
Bercu BB, Shulman D, Root AW, Spiliotis BE 1986 Growth hormone (GH) provocative testing does not reflect endogenous GH secretion. J Clin Endocrinol Metab 63: 709–716
Raben MS 1958 Treatment of a pituitary dwarf with human growth hormone. J Clin Endocrinol Metab 18: 901–903
Allen DB, Fost NC 1990 Growth hormone therapy for short stature: panacea or pandora's box?. J Pediatr 117: 16–21
Lantos J, Siegler M, Cuttler L 1989 Ethical issues in growth hormone therapy. JAMA 261: 1020–1024
Lippe B, Frasier SD 1989 How should we test for growth hormone deficiency, and whom should we treat?. J Pediatr 115: 585–587
Milner RDG 1990 Proper use of growth hormone. Arch Dis Child 65: 70–71
Frasier DS, Lippe BM 1990 Clinical review 11: the rational use of growth hormone during childhood. J Clin Endocrinol Metab 71: 269–273
Hindmarsh PC, Bridges NA, Brook CGD 1991 Wider indications for treatment with biosynthetic human growth hormone in children. Clin Endocrinol 34: 417–427
Brook CGD 1991 Who's for growth hormone?. BMJ 304: 131–132
Tanner JM, Whitehouse RH, Takaishi M 1966 Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. Arch Dis Child 41: 454–471
Aynsley Green A, Zachmann M, Prader A 1976 Interrelation of the therapeutic effects of growth hormone and testosterone on growth in hypopituitarism. J Pediatr 89: 992–999
Attie KM, Ramirez NR, Conte FA, Kaplan SL, Grumbach MM 1990 The pubertal growth spurt in eight patients with true precocious puberty and growth hormone deficiency: evidence for a direct role of sex steroids. J Clin Endocrinol Metab 71: 975–983
Rimoin DL, Merimee TJ, Rabinowitz D, McKusick VA 1968 Genetic aspects of clinical endocrinology. Rec Prog Horm Res 24: 365–437
Ranke MB 1987 A note on adults with growth hormone deficiency. Acta Paediatr Scand Suppl 331: 80–82
van der Werff ten Bosch JJ, Bot A 1990 Growth of males with idiopathic hypopituitarism without growth hormone treatment. Clin Endocrinol 32: 707–717
Kastrup DW, Christiansen JS, Anderson JK, Orskov H 1983 Increased growth rate following transfer to daily sc. administration from three weekly im. injection of hGH in growth hormone deficient children. Acta Endocrinol 104: 148–152
Albertsson-Wikland K, Westphal O, Westgren U 1986 Daily subcutaneous administration of human growth hormone in growth hormone deficient children. Acta Paediatr Scand 75: 89–97
Smith PJ, Hindmarsh PC, Brook CGD 1988 Contribution of dose and frequence of administration to the therapeutic effect of growth hormone. Arch Dis Child 63: 491–494
Brämswig JH, Schlösser H, Kiesse K 1995 Final height in children with growth hormone deficiency. Horm Res ( in press)
Job JC, Joab N, Toublanc JE, Canlorbe P 1984 Resultats a terme des traitements par l'hormone de croissance humaine. Arch Fr Pediatr 41: 477–482
Libber SM, Plotnick LP, Johanson AJ, Blizzard RM, Kwiterovich PO, Migeon CJ 1990 Long-term follow-up of hypopituitary patients treated with human growth hormone. Medicine 69: 46–55
Burns EC, Tanner JM, Preece MA, Cameron N 1981 Final height and pubertal development in 55 children with idiopathic growth hormone deficiency, treated for between 2 and 15 years with human growth hormone. Eur J Pediatr 137: 155–164
Darendeliler F, Hindmarsh PC, Preece MA, Cox L, Brook CG 1990 Growth hormone increases rate of pubertal maturation. Acta Endocrinol 122: 414–416
Milner RDG, Russel-Fraser T, Brook CGD, Cotes PM, Farquhar JW, Parkin JM, Preece MA, Snodgrass GJAI, Stuart Mason A, Tanner JM, Vince FP 1979 Experience with human growth hormone in Great Britain: the report of the MRC Working Party. Clin Endocrinol 11: 15–38
Zuppinger KA, Joss E, Roten A 1980 Endresultate bei hypophysarem Kleinwuchs nach Wachstumshormontherapie. Schweiz Rundsch Med Prax 69: 1167
Lenko HL, Leisti S, Perheentupa J 1982 The efficacy of growth hormone in different types of growth failure. An analysis of 101 cases. Eur J Pediatr 138: 241–249
Joss E, Zuppinger K, Schwarz HP, Roten H 1983 Final height of patients with pituitary growth failure and changes in growth variables after long term hormonal therapy. Pediatr Res 17: 676–679
Price DA, Ranke MB 1994 Final height following growth hormone treatment. In: Ranke, MB, Gunnarsson, R. (eds) Progress in Growth Hormone Therapy-5 Years of KIGS. J&J Verlag, Mannheim, pp 129–144
Rikken B, Wit JM, Petrov R, de Muinck Keizer-Schrama SMPF, Otten B, Van den Brande JL, Dutch Growth Hormone Working Group 1994 A regimen of daily growth hormone (GH) injections of 2 IU/m2 in GH deficient children does not lead to complete catch-up within 4 years but is favourable compared to older schemes. Horm Res 41: 92
Rikken B, Massa GG, Wit JM, Dutch Growth Hormone Working Group, 1995 Final height in a large cohort of Dutch patients with growth hormone deficiency treated with growth hormone. Horm Res 43: 135–137
Hibi I, Tanaka T, Tanae A, Kagawa J, Hashimoto N, Yoshizawa A, Shizume K 1989 The influence of gonadal function and the effect of gonadal suppression treatment on final height in growth hormone(GH)-treated GH-deficient children. J Clin Endocrinol Metab 69: 221–226
van der Werff ten Bosch JJ, Bot A 1988 Does hGH treatment promote adult height of hypopituitary children?. Neth J Med 32: 217–225
Leheup B, Palandri Y, Pierson M 1985 Final height of patients with idiopathic pituitary growth failure. Correlation with 5 adult height prediction methods at the onset and after one year of treatment. Pediatr Res 19: 607
Bourguignon JP, Vandeweghe M, Vanderschueren-Lodeweyckx M, Malvaux P, Wolter R, Du Caju M, Ernould C 1986 Pubertal growth and final height in hypopituitary boys: a minor role of bone age at onset of puberty. J Clin Endocrinol Metab 63: 376–382
Bundak R, Hindmarsh PC, Smith PJ, Brook CG 1988 Long-term auxologic effects of human growth hormone. J Pediatr 112: 875–879
Vicens-Calvet E, Vendrell JM, Albisu M, Potau N, Audi L, Gusine M 1984 The dosage dependency of growth and maturity in growth hormone deficiency treated with human growth hormone. Acta Paediatr Scand 73: 120–126
Toublanc JE, Couprie C, Garnier P, Job JC 1989 The effects of treatment combining an agonist of gonadotropin-releasing hormone with growth hormone deficiency. Acta Endocrinol 120: 795–799
Stanhope R, Brook CGD 1988 The effect of gonadotrophin releasing hormone analogue on height prognosis in growth hormone deficiency and normal puberty. Eur J Pediatr 148: 200–202
Cara JF, Kreiter ML, Rosenfield RL 1992 Height prognosis of children with true precocious puberty and growth hormone deficiency-effect of combination therapy with gonadotropin releasing hormone agonist and growth hormone. J Pediatr 120: 709–715
Burns EC, Tanner JM, Preece MA, Cameron N 1981 Growth hormone treatment in children with craniopharyngioma: final growth status. Clin Endocrinol 14: 587–595
Herber SM, Dunsmore IR, Milner RDG 1985 Final stature in brain tumors other than craniopharyngioma: effect of growth hormone. Horm Res 22: 63–67
Sulmont V, Brauner R, Fontoura M, Rappaport R 1990 Response to growth hormone treatment and final height after cranial or craniospinal irradiation. Acta Paediatr Scand 79: 542–549
Holl RW, Sorgo W, Teller WM, Heinze E 1990 How reliable are Bayley-Pinneau predictions of adult height? A study in 88 men with short stature followed to final height. Horm Res 33( suppl 3): 35.
Hindmarsh PC, Brook CGD 1987 Effect of growth hormone on short normal children. BMJ 295: 573–577
Moore WV, Moore KC, Gifford R, Hollowell JG, Donaldson DL 1992 Long-term treatment with growth hormone of children with short stature and normal growth hormone secretion. J Pediatr 120: 702–708
Hopwood NJ, Hintz RL, Gertner JM, Attie KM, Johanson AJ, Baptista J, Kuntze J, Blizzard RM, Cara JF, Chernausek SD, Kaplan SL, Lippe BM, Plotnick LP, Saenger P 1993 Growth response of children with non-growth-hormone deficiency and marked short stature during three years of growth hormone therapy. J Pediatr 123: 215–222
Albertsson-Wikland K 1993 Characteristics of children with idiopathic short stature in the Kabi Pharmacia International Growth Study, and their response to growth hormone treatment. Acta Paediatr Suppl 391: 75–78
Tanaka T, Hibi I, Takano K, Suwa S, Shizume K 1993 Effect of two-year growth hormone treatment in children with non-endocrine short stature. Clin Pediatr Endocrinol 2: 107–117
Ranke MB, Lindberg A 1994 Growth hormone treatment of idiopathic short stature: analysis of the database from KIGS, the Kabi Pharmacia International Growth Study. Acta Paediatr Suppl 406: 18–23
Zadik Z, Mira U, Landau H 1992 Final height after growth hormone therapy in peripubertal boys with a subnormal integrated concentration of growth hormone. Horm Res 37: 150–155
Wit JM, Boersma B, de Muinck Keizer-Schrama SMPF, Ni Nienhuis HE, Oostdijk W, Otten BJ, Delemarre-van de Waal HA, Reeser M, Waelkens JJJ, Rikken B, Massa GG 1995 Long term results of growth hormone therapy in children with short stature, subnormal growth rate and normal growth hormone response to secretagogues. Clin Endocrinol 42: 365–372
Loche S, Cambiaso P, Setzu S, Carta D, Marini R, Borrelli P, Cappa M 1994 Final height after growth hormone therapy in non-growth hormone-deficient children with short stature. J Pediatr 125: 196–200
Bierich JR, Nolte K, Drews K, Brugmann G 1992 Constitutional delay of growth and adolescence. Results of short-term and long-term treatment with GH. Acta Endocrinol 127: 392–396
Guyda HJ 1994 Final height attainment in normal children with short stature treated with growth hormone. Trends Endocrinol Metab 5: ( in press)
Marshall WA, Tanner JM 1969 Variations in pattern of pubertal changes in girls. Arch Dis Child 44: 291–303
Marshall WA, Tanner JM 1970 Variations in the pattern of pubertal changes in boys. Arch Dis Child 45: 12–23
Lesage C, Walker J, Landier F, Chatelain P, Chaussain JL, Bougneres PF 1991 Near normalization of adolescent height with growth hormone therapy in very short children without growth hormone deficiency. J Pediatr 119: 29–34
Boersma B, Rikken B, Wit JM, Dutch Growth Hormone Working Group, 1995 Catch-up growth in early treated patients with growth hormone deficiency. Arch Dis Child 72: 427–431
Siegel PT, Clopper R, Stabler B 1991 Psychological impact of significantly short stature. Acta Paediatr Scand Suppl 377: 14–18
Voss LD, Bailey BJR, Mulligam J 1991 Short stature and school performance-the Wessex growth study. Acta Paediatr Scand Suppl 377: 29–31
Van den Broeck J, Vanderschueren-Lodeweyckx M, Eggermont E 1988 Prediction of final height in boys with non-tumorous hypopituitarism. Eur J Pediatr 147: 245–247
Volta C, Ghizzoni L, Buono T, Ferrari F, Virdis R, Bernasconi S 1988 Final height in a group of untreated children with constitutional growth delay. Helv Paediatr Acta 43: 171–176
Ranke MB, Aronson AS 1989 Adult height in children with constitutional short stature. Acta Paediatr Scand Suppl 362: 27–31
Bramswig JH, Fasse M, Holthoff ML, von Lengerke HJ, von Petrykowski W, Schellong G 1990 Adult height in boys and girls with untreated short stature and constitutional delay of growth and puberty: accuracy of five different methods of height prediction. J Pediatr 117: 886–891
Von Kalckreuth G, Haferkamp F, Kessler M, Rosskamp RH 1991 Constitutional delay of growth and puberty: do they really reach their target height?. Horm Res 35: 222–225
Willig RP, Mahnke K, Stahnke N, Commentz JC, Sinnecker G, Winkler P 1990 Height predictions and final height in boys with constitutional delay of growth and puberty (CDGP). Horm Res 33: S3–34
Crowne EC, Shalet SM, Wallace WHB, Eminson DM, Price DA 1990 Final height in boys with untreated constitutional delay in growth and puberty. Arch Dis Child 65: 1109–1112
Crowne EC, Shalet SM, Wallace WHB, Eminson DM, Price DA 1991 Final height in girls with untreated constitutional delay in growth and puberty. Eur J Pediatr 150: 708–712
LaFranchi S, Hanne CE, Mandel SH 1991 Constitutional delay of growth: expected versus final adult height. Pediatrics 87: 82–87
Author information
Authors and Affiliations
Additional information
Manuscript dedicated to Professor H.K.A. Visser in honor of his retirement.
Rights and permissions
About this article
Cite this article
Wit, J., Kamp, G. & Rikken, B. Spontaneous Growth and Response to Growth Hormone Treatment in Children with Growth Hormone Deficiency and Idiopathic Short Stature. Pediatr Res 39, 295–302 (1996). https://doi.org/10.1203/00006450-199602000-00018
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199602000-00018
This article is cited by
-
Lebensqualität von kleinwüchsigen Kindern und Jugendlichen und Wachstumshormontherapie
Monatsschrift Kinderheilkunde (2023)
-
Growth hormone — past, present and future
Nature Reviews Endocrinology (2018)
-
Possible effects of an early diagnosis and treatment in patients with growth hormone deficiency: the state of art
Italian Journal of Pediatrics (2017)
-
A randomized pilot trial of growth hormone with anastrozole versus growth hormone alone, starting at the very end of puberty in adolescents with idiopathic short stature
International Journal of Pediatric Endocrinology (2015)
-
Treatment of children and adolescents with idiopathic short stature
Nature Reviews Endocrinology (2013)