Abstract
Objectives
We have shown that ezrin expression correlates with ovarian epithelial cancer (OVCA) cell proliferation and metastatic behavior. In this study, we evaluated ezrin expression in transformed ovarian superficial epithelial cells (OSE) in ovarian clefts and in culture.
Study Design
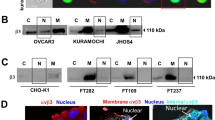
Immunohistochemistry and Western blotting for immunoreactive ezrin (ir-ezrin) in normal ovarian tissue, cultured OSE, and ovarian epithelial cancer cells.
Results
While ir-ezrin was not demonstrable in normal cuboidal surface cells or interior ovarian organelles, cells lining the ovarian clefts strongly expressed ir-ezrin. Long-term culture of OSE increased ezrin expression and cytological abnormalities. Administration of estradiol and insulin at levels reported in inclusions dramatically induced OSE ir-ezrin expression to OVCA levels and membrane specializations; ruffling, pseudopodia and filopodia. Moreover epidermal growth factor (EGF) drastically increased ezrin translocation in OSE cells in a time-dependent manner.
Conclusions
Ezrin expression by OSE increases during transformation. Ezrin expression is responsive to estradiol and growth factors previously shown to be present in ovarian inclusions. These findings suggest that the microenvironment in ovarian inclusions and clefts contributes to the development of OVCA. Our findings elaborate on the mechanism of the ovarian origin of OVCA.
Similar content being viewed by others
References
Okamura H, Katabuchi H. Pathophysiological dynamics of human ovarian surface epithelial cells in epithelial ovarian carcinogenesis. Int Rev Cytol. 2005;242:1–54.
Mittal KR, Goswami S, Demopoulos RI Immunohistochemical profile of ovarian inclusion cysts in patients with and without ovarian carcinoma. Histochem J. 1995;27(2):119–122.
Blaustein A, Kantius M, Kaganowicz A, Pervez N, Wells J. Inclusions in ovaries of females aged day 1-30 years. Int J Gynecol Pathol. 1982;1(2):145–153.
Jarboe EA, Folkins AK, Drapkin R, Ince TA, Agoston ES, Crum CP. Tubal and ovarian pathways to pelvic epithelial cancer: a pathological perspective. Histopathology. 2008;53(2): 127–138.
Vang R, Shih IeM, Kurman RJ. Ovarian low-grade and high-grade serous carcinoma: pathogenesis, clinicopathologic and molecular biologic features, and diagnostic problems. Adv Anat Pathol. 2009;16(5):267–282.
Auersperg N, Edelson MI, Mok SC, Johnson SW, Hamilton TC. The biology of ovarian cancer. Semin Oncol. 1998;25(3):281–304.
Bretscher A, Edwards K, Fehon RG. ERM proteins and merlin: integrators at the cell cortex. Nat Rev Mol Cell Biol. 2002;3(8): 586–599.
Chen Z, Fadiel A, Feng Y, Ohtani K, Rutherford T, Naftolin F. Ovarian epithelial carcinoma tyrosine phosphorylation, cell proliferation, and ezrin translocation are stimulated by interleukin lalpha and epidermal growth factor. Cancer. 2001;92(12): 3068–3075.
Song J, Fadiel A, Edusa V, et al. Estradiol-induced ezrin overex-pression in ovarian cancer: a new signaling domain for estrogen. Cancer Lett. 2005;220(l):57–65.
Bruce B, Khanna G, Ren L, et al. Expression of the cytoskeleton linker protein ezrin in human cancers. Clin Exp Metastasis. 2007; 24(2):68–78.
Ismail RS, Baldwin RL, Fang J, et al. Differential gene expression between normal and tumor-derived ovarian epithelial cells. Cancer Res. 2000;60(23):6744–6749.
Okamura H, Katabuchi H. Detailed morphology of human ovarian surface epithelium focusing on its metaplastic and neoplastic capability. Ital J Anat Embryol. 2001;106(2 suppl 2):263–276.
Gusberg SB, Deligdisch L. Ovarian dysplasia. A study of identical twins. Cancer. 1984;54(l):l–4.
Deligdisch L, Gil J. Characterization of ovarian dysplasia by interactive morphometry. Cancer. 1989;63(4):748–755.
Plaxe SC, Deligdisch L, Dottino PR, Cohen CJ. Ovarian intraepithelial neoplasia demonstrated in patients with stage I ovarian carcinoma. Gynecol Oncol. 1990;38(3):367–372.
Wong AS, Auersperg N. Ovarian surface epithelium: family history and early events in ovarian cancer. Reprod Biol Endocrinol. 2003; 1:70.
Crum CP. Intercepting pelvic cancer in the distal fallopian tube: theories and realities. Mol Oncol. 2009;3(2): 165–170.
Seidman JD, Yemelyanova A, Zaino RJ, Kurman RJ. The fallopian tube-peritoneal junction: a potential site of carcinogenesis. Int J Gynecol Pathol. 2011;30(1):4–11.
Auersperg N, Wong AS, Choi KC, Kang SK, Leung PC. Ovarian surface epithelium: biology, endocrinology, and pathology. Endocr Rev. 2001;22(2):255–288.
Heller DS, Hameed M, Baergen R. Lack of proliferative activity of surface epithelial inclusion cysts of the ovary. Int J Gynecol Cancer. 2003;13(3):303–307.
Werness BA, Afify AM, Bielat KL, Eltabbakh GH, Piver MS, Paterson JM. Altered surface and cyst epithelium of ovaries removed prophylactically from women with a family history of ovarian cancer. Hum Pathol. 1999;30(2):151–157.
Dewially D, Catteau-Jonard S, Poncelet E. Which morphological investigations and how to interpret them to make the diagnosis of PCOS? Ann Endocrinol. (Paris). 2010;71(3):183-188.
Judd HL, Fournet N. Changes of ovarian hormonal function with aging. Exp Gerontol. 1994;29(3–4):285–298.
Fathalla MF. Incessant ovulation-a factor in ovarian neoplasia? Lancet. 1971;2(7716):163.
Albrecht ED, Aberdeen GW, Niklaus AL, Babischkin JS, Suresch DL, Pepe GJ. Acute temporal regulation of vascular endothelial growth/permeability factor expression and endothelial morphology in the baboon endometrium by ovarian steroids. J Clin Endocrinol Metab. 2003;88(6):2844–2852.
Punnonen R, Teisala K, Kuoppala T, Bennett B, Punnonen J. Cytokine production profiles in the peritoneal fluids of patients with malignant or benign gynecologic tumors. Cancer. 1998; 83(4):788–796.
Malik S, Balkwill F. Epithelial ovarian cancer: a cytokine propelled disease? Br J Cancer. 1991;64(4):617–620.
Okamura H, Katabuchi H, Nitta M, Ohtake H. Structural changes and cell properties of human ovarian surface epithelium in ovarian pathophysiology. Microsc Res Tech. 2006; 69(6):469–481.
Louvet-Vallee S. ERM proteins: from cellular architecture to cell signaling. Biol Cell. 2000;92(5):305–316.
Mangeat P, Roy C, Martin M. ERM proteins in cell adhesion and membrane dynamics. Trends Cell Biol. 1999;9(5):187–192.
Sato N, Funayama N, Nagafuchi A, Yonemura S, Tsukita S, Tsukita S. A gene family consisting of ezrin, radixin and moesin. Its specific localization at actin filament/plasma membrane association sites. J Cell Sci. 1992;103(pt 1):131–143.
MacLusky NJ, Voit R, Lazo JS, et al. Aromatase activity in human ovarian cancer. Steroids. 1987;50(4–6):423–433.
Schwartz PE, MacLusky N, Merino MJ, Livolsi VA, Kohorn EI, Eisenfeld A. Are cytosol estrogen and progestin receptors of prognostic significance in the management of epithelial ovarian cancers? Obstet Gynecol. 1986;68(6):751–758.
Schwartz PE, LiVolsi VA, Hildreth N, MacLusky NJ, Naftolin FN, Eisenfeld AJ. Estrogen receptors in ovarian epithelial carcinoma. Obstet Gynecol. 1982;59(2):229–238.
Li AJ, Baldwin RL, Karlan BY. Estrogen and progesterone receptor subtype expression in normal and malignant ovarian epithelial cell cultures. Am J Obstet Gynecol. 2003;189(1): 22–27.
Wong AS, Leung PC. Role of endocrine and growth factors on the ovarian surface epithelium. J Obstet Gynaecol Res. 2007;33(1): 3–16.
Garcia-Segura LM, Olmos G, Tranque P, Naftolin F. Rapid effects of gonadal steroids upon hypothalamic neuronal membrane ultrastructure. J Steroid Biochem. 1987;27(l–3): 615–623.
Simoncini T, Scorticati C, Mannella P, et al. Estrogen receptor alpha interacts with Galpha13 to drive actin remodeling and endothelial cell migration via the RhoA/Rho kinase/moesin pathway. Mol Endocrinol. 2006;20(8):1756–1771.
Roby KF, Taylor CC, Sweetwood JP, et al. Development of a syngeneic mouse model for events related to ovarian cancer. Carcinogenesis. 2000;21(4):585–591.
Ohtani K, Sakamoto H, Rutherford T, Chen Z, Satoh K, Naftolin F. Ezrin, a membrane-cytoskeletal linking protein, is involved in the process of invasion of endometrial cancer cells. Cancer Lett. 1999;147(l–2):31–38.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fadiel, A., Chen, Z., Ulukus, E. et al. Ezrin Overexpression by Transformed Human Ovarian Surface Epithelial Cells, Ovarian Cleft Cells, and Serous Ovarian Adenocarcinoma Cells. Reprod. Sci. 19, 797–805 (2012). https://doi.org/10.1177/1933719111433884
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719111433884