Abstract
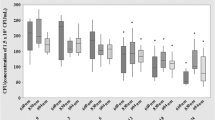
Low-intensity red lasers are proposed for treatment of oral aphthous ulcers based on biostimulative effects. However, effects of low-intensity lasers at fluences used in clinical protocols on DNA are controversial. The aim of this work was to evaluate the effects of low-intensity red laser on survival and induction of filamentation of Escherichia coli cells, and induction of DNA lesions in bacterial plasmids. Escherichia coli cultures were exposed to laser (660 nm, 100 mW, 25 and 45 J cm−2) to study bacterial survival and filamentation. Also, bacterial plasmids were exposed to laser to study DNA lesions by electrophoretic profile and action of DNA repair enzymes. Data indicate that low-intensity red laser: (i) had no effect on survival of E. coli wild type, exonuclease III and formamidopyrimidine DNA glycosylase/MutM protein but decreased the survival of endonuclease III deficient cultures; (ii) induced bacterial filamentation, (iii) there was no alteration in the electrophoretic profile of plasmids in agarose gels, (iv) there was no alteration in the electrophoretic profile of plasmids incubated with formamidopyrimidine DNA glycosylase/MutM protein and endonuclease III enzymes, but it altered the electrophoretic profile of plasmids incubated with exonuclease III. Low-intensity red laser at therapeutic fluences has an effect on the survival of E. coli endonuclease III deficient cells, induces bacterial filamentation in E. coli cultures and DNA lesions targeted by exonuclease III.
Similar content being viewed by others
References
I. Ratkay-Traub, B. Hopp, Z. Bor, L. Dux, D. L. Becker and T., Krenacs, Regeneration of rabbit cornea following excimer laser photorefractive keratectomy: a study on gap junctions, epithelial junctions and epidermal growth factor receptor expression in correlation with cell proliferation Exp. Eye Res. 2001 73 291–302
Y. G., Kim, Laser mediated production of reactive oxygen and nitrogen species; implications for therapy Free Radical Res. 2002 36 1243–1250
X. Gao and D., Xing, Molecular mechanisms of cell proliferation induced by low power laser irradiation J. Biomed. Sci. 2009 16 4
P. V. Peplow, T. Y. Chung and G. D., Baxter, Laser photobiomodulation of wound healing: a review of experimental studies in Mouse and Rat animal models Photomed. Laser Surg. 2010 28 291–325
L. Longo, S. Evangelista, G. Tinacci and A. G., Sesti, Effect of diodes-laser silver arsenide-aluminium (Ga-Al-As) 904 nm on healing of experimental wounds Lasers Surg. Med. 1987 7 444–447
L. Almeida-Lopes, J. Rigau, R. Zangaro, J. Guidugli-Neto and M. M., Jaeger, Comparison of the low level laser therapy effects on cultured human gingival fibroblasts proliferation using different irradiance and same fluence Lasers Surg. Med. 2001 29 179–184
A. N. Pereira, C. De P. Eduardo, E. Matson and M. M., Marques, Effect of low-power laser irradiation on cell growth and procollagen synthesis of cultured fibroblasts Lasers Surg. Med. 2001 31 263–267
T. O. De Souza, M. A. Martins, S. K. Bussadori, K. P. Fernandes, E. Y. Tanji, R. A. Mesquita-Ferrari and M. D., Martins, Clinical evaluation of low-level laser treatment for recurring aphthous stomatitis Photomed. Laser Surg. 2010 28 Suppl 2 S85–S88
T., Karu, Primary and secondary mechanisms of action of visible to near-IR radiation on cells J. Photochem. Photobiol., B 1999 49 1–17
T. Karu, L. Pyatibrat and G., Kalendo, Irradiation with HeNe laser can influence the cytotoxic response of HeLa cells to ionizing radiation Int. J. Radiat. Biol. 1994 65 691–697
S. W. Botchway, A. G. Crisostomo, A. W. Parker and R. H., Bisby, Near infrared multiphoton-induced generation and detection of hydroxyl radicals in a biochemical system Arch. Biochem. Biophys. 2007 464 314–321
D. H. Hawkins and H., Abrahamse, The role of laser fluence in cell viability, proliferation, and membrane integrity of wounded human skin fibroblasts following helium-neon laser irradiation Lasers Surg. Med. 2006 38 74–83
C. Godon, F. P. Cordelières, D. Biard, N. Giocanti, F. Mégnin-Chanet, J. Hall and V., Favaudon, PARP inhibition versus PARP-1 silencing: different outcomes in terms of single-strand break repair and radiation susceptibility Nucleic Acids Res. 2008 36 4454–4464
A. B. Mbene, N. N. Houreld and H. J., Abrahamse, DNA damage after phototherapy in wounded fibroblast cells irradiated with 16 J cm−2J. Photochem. Photobiol., B 2009 94 131–137
M. A. Turner and R. B., Webb, Comparative mutagenesis and interaction between near-ultraviolet (313 to 405 nm) and far-ultraviolet (254 nm) radiation in Escherichia coli strains with differing repair capabilities J. Bacteriol. 1981 147 410–417
A. G. Miguel and R. M., Tyrrell, Induction of oxygen-dependent lethal damage by monochromatic UVB (313 nm) radiation: strand breakage, repair and cell death Carcinogenesis 1983 4 375–380
R. Kohli and P. K., Gupta, Irradiance dependence of the He-Ne laser-induced protection against UVC radiation in E. coli strains J. Photochem. Photobiol., B 2003 69 161–167
A. S. Fonseca, T. O. Moreira, D. L. Paixão, F. M. Farias, O. R. Guimarães, S. Paoli, M. Geller and F., Paoli, Effect of laser therapy on DNA damage Lasers Surg. Med. 2010 42 481–488
A. S. Fonseca, M. Geller, M. B. Filho, S. S. Valença and F., Paoli, Low-level infrared laser effect on plasmid DNA Lasers Med. Sci. 2011 27 121–130
R. T. Chow, M. I. Johnson, R. A. Lopes-Martins and J. M., Bjordal, Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials Lancet 2009 374 9705 1897–1908
P. Angeletti, M. D. Pereira, H. C. Gomes, C. T. Hino and L. M., Ferreira, Effect of low-level laser therapy (GaAlAs) on bone regeneration in midpalatal anterior suture after surgically assisted rapid maxillary expansion Oral Surg., Oral Med., Oral Pathol., Oral Radiol. Endodontol. 2010 109 e38–e46
T. Dai, Y. Y. Huang and M. R., Hamblin, Photodynamic therapy for localized infections - state of the art Photodiagn. Photodyn. Ther. 2009 6 170–188
S. Perni, P. Prokopovich, J. Pratten, I. P. Parkin and M., Wilson, Nanoparticles: their potential use in antibacterial photodynamic therapy Photochem. Photobiol. Sci. 2011 10 712–720
G. B. Kharkwal, S. K. Sharma, Y. Y. Huang, T. Dai and M. R., Hamblin, Photodynamic therapy for infections: clinical applications Lasers Surg. Med. 2011 43 755–767
N. R. Asad, L. M. Asad, A. B. Silva, I. Felzenszwalb and A. C. Leitão Hydrogen peroxide induces protection against lethal effects of cumene hydroperoxide in Escherichia coli cells: an Ahp dependent and OxyR independent system? Mutat. Res. 1998 407 253–259
A. S. Fonseca, G. A. Presta, M. Geller and F., Paoli, Low intensity infrared laser induces filamentation in Escherichia coli cells Laser Phys. 2011 21 1–9
J. O. Blaisdell and S. S., Wallace, Abortive base-excision repair of radiation-induced clustered DNA lesions in Escherichia coli Proc. Natl. Acad. Sci. U. S. A. 2001 98 7426–7430
R. A. Slayden, D. L. Knudson and J. T., Belisle, Identification of cell cycle regulators in mycobacterium tuberculosis by inhibition of septum formation and global transcriptional analysis Microbiology 2006 152 1789–1797
B. Modenutti, E. Balseiro, G. Corno, C. Callieri, R. Bertoni and E., Caravati, Ultraviolet radiation induces filamentation in bacterial assemblages from North Andean Patagonian lakes Photochem. Photobiol. 2010 86 871–881
J. G. Cappuccino and N. Sherman, Microbiology: A Laboratory Manual, Benjamin Cummings Science Publishing, California, 1999
J. Sambrook, E. F. Fritsch and T. Maniatis, Extraction and purification of plasmid DNA, in Molecular cloning: A Laboratory Manual, Cold Spring Harbour Laboratory Press, New York, 1989
G. L. Klebanov, L. A. Strashkevich, T. V. Chichuk, T. M. Modestova and YuA., Vladimirov, Effects of endogenous photosensitizers on the laser-induced priming of leucocytes Membr. Cell Biol. 1998 12 339–354
M. Broccio, F. Della Rovere, F. Granata, U. Wanderlingh, A. Zirilli, A. Tanzariello, G. Pirrone and G., Broccio, Free radical erythrocyte damage in tumoral disease assessed by He-Ne laser and optical microscope through “Heinz Bodies” method Anticancer Res. 1998 18 1075–1078
A. S. Fonseca, G. A. Presta, M. Geller, F. Paoli and S. S. Valença Low-intensity infrared laser increases plasma proteins and induces oxidative stress in vitro Lasers Med. Sci. 2011 27 211–217
M. Atif, S. Firdous, A. Khurshid, L. Noreen, S. S. Z. Zaidi and M., Ikram, In vitro study of 5-aminolevulinic acid-based photodynamic therapy for apoptosis in human cervical HeLa cell line Laser Phys. Lett. 2009 6 886–891
C. S. Xu and A. W. N., Leung, Light-activated hypericin induces cellular destruction of nasopharyngeal carcinoma cells Laser Phys. Lett. 2010 7 68–72
C. S. Xu, A. W. N. Leung, L. Liu and X. S., Xia, LED-activated pheophorbide a induces cellular destruction of colon cancer cells Laser Phys. Lett. 2010 7 544–548
M. Atif, M. Fakhar-e-Alam, S. Firdous, S. S. Z. Zaidi, R. Suleman and M., Ikram, Study of the efficacy of 5-ALA mediated photodynamic therapy on human rhabdomyosarcoma cell line (RD) Laser Phys. Lett. 2010 7 757–764
J. H. Park, M. Y. Ahn, Y. C. Kim, S. A. Kim, Y. H. Moon, S. G. Ahn and J. H., Yoon, In vitro and in vivo antimicrobial effect of photodynamic therapy using a highly pure chlorine 6 against Staphylococcus aureus Xen29 Biol. Pharm. Bull. 2012 35 509–514
L. Eibenschutz, S. Marenda, P. Buccini, P. De Simone, A. Ferrari, G. Mariani, V. Silipo and C. Catricalà Giant and large basal cell carcinoma treated with topical photodynamic therapy Eur. J. Dermatol. 2008 18 663–666
D. M. Wilson III, B. P. Engelward and L. Samson, Procaryotic base repair, in DNA Damage and Repair. Volume I: DNA Repair in Procaryotes and Lower Eukaryotes, ed. J. A. Nickoloff and M. F. Hoekstra, Humana Press, New Jersey, 1998, pp. 29-64
R. Jain, P. Kumar and U., Varshney, A distinct role of formamidopyrimidine DNA glycosylase (MutM) in down-regulation of accumulation of G, C mutations and protection against oxidative stress in mycobacteria DNA Repair 2007 6 1774–1785
T., Karu, Laser biostimulation: a photobiological phenomenon J. Photochem. Photobiol., B 1989 3 638–640
W. H. Koch and R. Woodgate, The SOS response, in DNA Damage and Repair. Volume I: DNA Repair in Procaryotes and Lower Eukaryotes, ed. J. A. Nickoloff and M. F. Hoekstra, Humana Press., New Jersey, 1998, pp. 107-134
L. J. Piddock and R. N., Walters, Bactericidal activities of five quinolones for Escherichia coli strains with mutations in genes encoding the SOS response or cell division Antimicrob. Agents Chemother. 1992 36 819–825
K. J. Davis, P. Vogel, D. L. Fritz, K. E. Steele, M. L. Pitt and S. L., Welkos, Bacterial filamentation of Yersinia pestis by beta-lactam antibiotics in experimentally infected mice Arch. Pathol. Lab. Med. 1997 121 865–868
B. Weiss, Regulation of endonuclease IV as part of an oxidative stress response in Escherichia coli, in DNA Damage and Repair. Volume I: DNA Repair in Procaryotes and Lower Eukaryotes, ed. J. A. Nickoloff and M. F. Hoekstra, Humana Press., New Jersey, 1998, pp. 85-105
J. A. Imlay and S., Linn, Mutagenesis and stress responses induced in Escherichia coli by hydrogen peroxide J. Bacteriol. 1987 169 2967–2976
S. Park and J. A., Imlay, High levels of intracellular cysteine promote oxidative DNA damage by driving the fenton reaction J. Bacteriol. 2003 185 1942–1950
H. Samaluru, L. Saisree and M., Reddy, Role of SufI (FtsP) in cell division of Escherichia coli: evidence for its involvement in stabilizing the assembly of the divisome J. Bacteriol. 2007 189 8044–8052
R. Kohli, B. Bose and P. K., Gupta, Induction of phr gene expression in E. coli strain KY706/pPL-1 by He-Ne laser (632.8 nm) irradiation J. Photochem. Photobiol., B 2001 60 136–142
R. E. Zirkle and N. R., Krieg, Development of a method based on alkaline gel electrophoresis for estimation of oxidative damage to DNA in Escherichia coli J. Appl. Microbiol. 2008 81 133–138
J. Kujawa, I. B. Zavodnik, A. Lapshina, M. Labieniec and M., Bryszewska, Cell survival, DNA, and protein damage in B14 cells under low-intensity near-infrared (810 nm) laser irradiation Photomed. Laser Surg. 2004 22 504–508
D. Hawkins and H., Abrahamse, Biological effects of helium-neon laser irradiation on normal and wounded human skin fibroblasts Photomed. Laser Surg. 2005 23 251–259
N. Grossman, N. Schneid, H. Reuveni, S. Halevy and R., Lubart, 780 nm low power diode laser irradiation stimulates proliferation of keratinocyte cultures: involvement of reactive oxygen species Lasers Surg. Med. 1998 22 212–218
K. Nakagiri, M. Okada, Y. Tsuji, M. Yoshida and T., Yamashita, Evaluation of local platelet deposition during laser thermal angioplasty Kobe J. Med. Sci. 1999 45 137–148
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
da Silva Marciano, R., da Silva Sergio, L.P., Polignano, G.A.C. et al. Laser for treatment of aphthous ulcers on bacteria cultures and DNA. Photochem Photobiol Sci 11, 1476–1483 (2012). https://doi.org/10.1039/c2pp25027f
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1039/c2pp25027f