Abstract
Study design:
Case report and literature review.
Objective:
To illustrate that ossification of the proximal thoracic ligamenta flava can be a rare cause of acute myelopathy in a Caucasian patient and that timely surgery can lead to a good outcome.
Setting:
Nottingham, UK.
Methods:
Proximal multiple contiguous ossified thoracic ligamenta flava from T3/T4 to T5/T6 causing acute myelopathy was diagnosed in a Caucasian man based on history and examination followed by magnetic resonance imaging and computed tomography scanning. The literature is reviewed for all reported cases of ossified ligamenta flava causing myelopathy in Caucasians.
Results:
Following prompt diagnosis and T3 to T5 laminectomies, our patient made near-complete neurological recovery over a 10-month period. This condition usually affects the lower thoracic spine. Although chronic and subacute myelopathy secondary to this circumstance has been reported in Caucasians, acute myelopathy has not been reported and proximal thoracic involvement has been reported twice.
Conclusion:
Ossification of the proximal thoracic ligamenta flava can be a rare cause of acute myelopathy in Caucasians. Prognosis following decompressive surgery is usually good.
Similar content being viewed by others
Introduction
Proximal thoracic myelopathy is mainly due to neoplastic disease in Caucasians. A less recognised cause is the ossification of the ligamenta flava (OLF), a condition that is rarely reported in the Western literature. Although thoracic OLF usually occurs in the lower thoracic spine,1, 2, 3, 4, 5, 6, 7, 8, 9, 10 it has been reported to occur at higher thoracic levels resulting in proximal myelopathy.11, 12 This is particularly important because, regardless of the level and severity of the disease, OLF is easily treatable by decompressive laminectomy if the diagnosis is made early.
Case report
A 45-year-old Caucasian man presented with a 3-week history of acute progressive lower limb weakness, walking difficulties and loss of sensation below the epigastrium. His upper limbs were unaffected and he remained doubly continent. Examination revealed a 6 feet 6 inches tall and obese gentleman who walked with a very unsteady broad-based gait. He had a sensory level at T6 with bilateral loss of lower limb proprioception. Both lower limbs were hypertonic with weakness of the proximal hip girdle musculature, but normal power in the distal muscle groups. There were bilateral ankle cloni, lower limb hyper reflexia and up-going plantars. Rectal examination was normal.
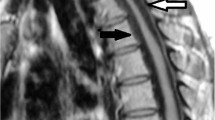
Haematological investigations and plain radiographs were normal. Magnetic resonance imaging (MRI) scans showed multiple contiguous hypointense posteriorly based lesions extending from T3/T4 to T5/T6 causing spinal cord compression and myelomalacia at T3/T4 level (Figure 1). Computed tomography (CT) scans showed a right-sided posterolateral hyperdense mass at T3/T4 interlaminar space, causing extradural compression of the spinal cord. Similar but smaller lesions were identified at T4/T5 and T5/T6 (Figure 2).
Bilateral laminectomies at T3, T4 and T5 were performed revealing OLF at all three levels. A generous and careful decompression of the spinal cord was performed. There were no intra- or postoperative complications. At 10 months follow-up, he was walking unaided within the house, was using one stick for short distances and a wheelchair for long distances. The motor power and sensation, including proprioception in his lower limbs, returned to normal. However, there was persistent bilateral lower limb hyper-reflexia, up-going plantars but no ankle cloni.
Discussion
Tumour and less commonly bacterial infections are the two major causes of thoracic myelopathy in Caucasians. Myelopathy due to other causes occurs less frequently in the thoracic spine, because it is less prone to degeneration as the ribs restrict movement.3 Thoracic compressive stenotic syndromes are primarily due to the lamina, facet or ligamentum flaval hypertrophy13, 14 and rarely due to an intervertebral disc herniation.15 Three conditions causing ossification of the spinal ligaments have been described. Diffuse idiopathic skeletal hyperostosis (DISH) and ossification of posterior longitudinal ligament (OPLL) are comparatively much more common conditions than OLF, the latter being almost exclusively reported from Asian centres.4, 5, 16
Aetiology
The pathoaetiology of OLF remains uncertain. The higher prevalence in Japan implicates genetic and/or environmental factors.17 Patients with OLF have higher frequency of non-insulin dependent diabetes,17 obesity, hyperinsulinism, haemochromatosis and calcium metabolism abnormalities.6 However, the pathomechanism remains unclear. Our patient suffered from both obesity and non-insulin-dependent diabetes. Thoracic OLF usually occurs at T9–T12,1, 4, 5 this region being particularly prone to degenerative process.14 Otani et al18 noted a high incidence in cases with thoracic hyperkyphosis and suggested that the altered mechanical stresses as a consequence of this predispose to the development of OLF. Although our patient had a normal thoracic kyphosis, his MRI scan showed multilevel thoracic disc degeneration. Recent studies revealed that fibronectin, bone morphogenic proteins and transforming growth factor beta played an important role in the development of ossification of the spinal ligaments.17
Clinical course
OLF predominantly affects middle-aged men with a male to female ratio of approximately 2.7:1.6 The clinical course is characterised by progressive myelopathy. The most common symptoms are altered gait, weakness and numbness in the lower limbs, and the signs include spastic paraparesis with hyper-reflexia, up-going plantars, clonus; and sensory deficits mainly involving deep sensation and proprioception.5, 6, 19 Sphincter disturbance and radicular symptoms are rare.
Radiological findings
The combination of MRI and CT is required for the precise diagnosis of OLF.1 MRI accurately delineates the location and extent of spinal cord compression in several planes, but has difficulty differentiating between an ossified or hypertrophied ligament.16 CT scanning best demonstrates the increased density of the ossific changes. Plain spinal radiographs may show beak-like bone projections from the apophyseal joints into the spinal canal on the lateral views.17
Histology
Age-related enlargement of the ligamenta flava is common. Ono et al17 reported that ossification of the spinal ligaments have the following characteristics: (1) ectopic bone formation within the ligaments; (2) tissue hyperplasia and cellular proliferation; (3) before ossification, sequential occurrence of fibrocartilaginous cellular proliferation followed by calcification, tissue resorption with vascular ingrowth and (4) specific site of predilection and often occurring in combination with senile ankylosing vertebral hyperostosis or DISH.
Surgery
The surgical procedure most commonly performed is a laminectomy with removal of ossified ligaments (Table 1). Okada et al4 recommended a laminoplasty. This may provide better stability in patients with extensive lesions and may reduce the incidence of postoperative kyphosis and restenosis owing to the scar tissue. Medial facetectomy with or without supplemental internal fixation can be performed if degenerative hypertrophy of the articular masses is present.20
Prognosis depends not only on the extent of the lesions but also on the time to diagnosis and treatment.19 The clinical outcome is usually good if early surgical decompression is performed1, 19 (Table 1). Regular follow-up is necessary as recurrence or development of ossification at other levels has been reported.2, 20
Conclusion
Over the past few decades, OLF has been occasionally reported in non-Asian patients. This is the first report of acute proximal thoracic myelopathy caused by OLF in a Caucasian. OLF is an eminently treatable condition if diagnosed early. Hence OLF should be considered in the differential diagnosis of all patients presenting with thoracic myelopathy, even when the upper thoracic spine is involved.
References
Hanakita J, Suwa H, Ohta F, Nishi S, Sakaida H, Iihara K . Neuroradiological examination of thoracic radiculomyelopathy due to ossification of the ligamentum flavum. Neuroradiology 1990; 32: 38–42.
Payer M, Bruder E, Fischer JA, Benini A . Thoracic myelopathy due to enlarged ossified yellow ligaments. Case report and review of the literature. J Neurosurg 2000; 92: 105–108.
Arafat QW, Jackowski A, Chavda SV, West RJ . Case report: ossification of the thoracic ligamenta flava in a Caucasian: a rare cause of myelopathy. Br J Radiol 1993; 66: 1193–1196.
Okada K, Oka S, Tohge K, Ono K, Yonenobu K, Hosoya T . Thoracic myelopathy caused by ossification of the ligamentum flavum. Clinicopathologic study and surgical treatment. Spine 1991; 16: 280–287.
Yonenobu K et al. Thoracic myelopathy secondary to ossification of the spinal ligament. J Neurosurg 1987; 66: 511–518.
Celli P, Caroli E, Trillo G, Ferrante L . Ossification of the ligamentum flavum in a Caucasian. Case report. J Neurosurg Sci 2002; 46: 96–99; discussion 9.
Omojola MF, Cardoso ER, Fox AJ, Drake CG, Durward QJ . Thoracic myelopathy secondary to ossified ligamentum flavum. J Neurosurg 1982; 56: 448–450.
Parekh HC, Gurusinghe NT, Perera SS, Prabhu SS . Ossification of the ligamentum flavum in a Caucasian: case report. Br J Neurosurg 1993; 7: 687–690.
Shiraishi T, Crock HV, Lewis P . Thoracic myelopathy due to isolated ossification of the ligamentum flavum. J Bone Joint Surg Br 1995; 77: 131–133.
Vera CL et al. Paraplegia due to ossification of ligamenta flava in X-linked hypophosphatemia. A case report. Spine 1997; 22: 710–715.
Kruse JJ, Awasthi D, Harris M, Waguespack A . Ossification of the ligamentum flavum as a cause of myelopathy in North America: report of three cases. J Spinal Disord 2000; 13: 22–25.
van Oostenbrugge RJ, Herpers MJ, de Kruijk JR . Spinal cord compression caused by unusual location and extension of ossified ligamenta flava in a Caucasian male. A case report and literature review. Spine 1999; 24: 486–488.
Jaspan T, Holland IM, Punt JA . Thoracic spinal canal stenosis. Neuroradiology 1987; 29: 217.
Smith DE, Godersky JC . Thoracic spondylosis: an unusual cause of myelopathy. Neurosurgery 1987; 20: 589–593.
Arseni C, Nash F . Thoracic intervertebral disc protrusion: a clinical study. J Neurosurg 1960; 17: 418–430.
Yamashita Y et al. Spinal cord compression due to ossification of ligaments: MR imaging. Radiology 1990; 175: 843–848.
Ono K, Yonenobu K, Miyamoto S, Okada K . Pathology of ossification of the posterior longitudinal ligament and ligamentum flavum. Clin Orthop 1999; 359: 18–26.
Otani K, Aihara T, Tanaka A, Shibasaki K . Ossification of the ligamentum flavum of the thoracic spine in adult kyphosis. Int Orthop 1986; 10: 135–139.
Shiokawa K, Hanakita J, Suwa H, Saiki M, Oda M, Kajiwara M . Clinical analysis and prognostic study of ossified ligamentum flavum of the thoracic spine. J Neurosurg 2001; 94: 221–226.
Nishiura I, Isozumi T, Nishihara K, Handa H, Koyama T . Surgical approach to ossification of the thoracic yellow ligament. Surg Neurol 1999; 51: 368–372.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tokala, D., Lam, K. & Prince, H. Ossification of the proximal thoracic ligamenta flava causing acute myelopathy in a Caucasian: case report and literature review. Spinal Cord 45, 310–313 (2007). https://doi.org/10.1038/sj.sc.3101953
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101953
Keywords
This article is cited by
-
Genetics of Diffuse Idiopathic Skeletal Hyperostosis and Ossification of the Spinal Ligaments
Current Osteoporosis Reports (2023)
-
BMP2 Modified by the m6A Demethylation Enzyme ALKBH5 in the Ossification of the Ligamentum Flavum Through the AKT Signaling Pathway
Calcified Tissue International (2020)