Abstract
Study design: A case report.
Objectives: To present and discuss some of the difficulties in the diagnosis of brucellar spondylitis.
Setting: Ankara University, Ibni Sina Hospital, Turkey.
Methods: We report a patient with paraplegia, misdiagnosed as having a malignancy or tuberculosis who actually suffered from brucellar spondylitis. Diagnosis was established by her history and a compatible clinical picture together with a standard tube agglutination (Wright test) titer of ⩾1/160 of antibodies for brucellosis. The patient was treated with oral doxycycline, rifampicin, and ciprofloxacin combination.
Results: At the end of the treatment, the blood Brucella Wright and anti-human globulin T titer levels decreased. Her lower limb weakness improved. She could walk, and climb stairs with the help of a cane. Urinary retention and fecal incontinence also resolved.
Conclusion: Brucellosis is a systemic infection involving the musculoskeletal and nervous systems. Spondylitis frequently occurs in elderly patients. An early diagnosis of brucellar spondylitis can often be difficult. In endemic regions, as in the case of our country, brucellar spondylitis should always be considered in the differential diagnosis of older patients with back pain and constitutional symptoms. An early diagnosis will help to prevent the development of more severe complications such as spinal cord compression.
Similar content being viewed by others
Introduction
Brucellosis is a zoonosis with a worldwide distribution. Over 500,000 cases of brucellosis are reported yearly to the World Health Organization from 100 countries. Brucella melitensis infection, distributed primarily in the Mediterranean region, Latin America, and Asia, accounts for the majority of cases.1 Brucellosis is still a health problem in Turkey.2
Brucellosis may involve any organ system but is most commonly found in the bone, joints, central nervous system, heart, lung, spleen, testes, liver, gall bladder, kidney, prostate, and skin. Osteoarticular disease is the most common complication of brucellosis and has been described in 10–85% of patients. While arthritis, bursitis, tenosynovitis, and sacroiliitis are more frequently observed in younger patients, the frequency of spondylodiscitis increases with aging, and its diagnosis may be difficult.1,2,3,4
In this paper, we report a patient first misdiagnosed in another clinic as having a tumor or tuberculosis. The patient presented with paraplegia due to a compression fracture and a paravertebral soft tissue mass in the thoracic spine, which was later found out in our clinic to be due to brucellar spondylitis.
Case report
A 65-year-old housewife, living in the central Anatolian region of Turkey, presented with upper back pain, fever, and sweating in September 2001. She was treated for presumed pneumonia, but her symptoms did not resolve. She was subsequently admitted to a neurology clinic in a state insurance hospital because of the acute development of lower limb weakness with sensory loss, urinary retention, and fecal incontinence. Magnetic resonance imaging (MRI) suggested malignancy, prompting the patient to be referred to the orthopedic clinic of our university.
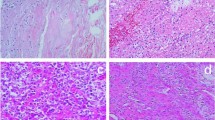
In the university hospital, the MRI interpretation demonstrated decreased signal intensity of the T2–4 vertebrae on T1-weighted images and increased signal intensity on T2-weighted images. There was T3–4 disc involvement and compression of the T3 vertebra. The presence of a paraspinal soft tissue mass was also noted, which was extending into the epidural space, most prominently at the T2 vertebra (Figures 1 and 2). The patient underwent a total T1–5 laminectomy and posterior fusion in December 2001 for presumed malignancy. The soft-tissue mass was not removed to prevent a probable injury of the spinal cord. Histopathology of the biopsied material revealed chronic inflammation in fibrous and bony tissues. There were no malignant cells identified.
Antibiotics were initiated for presumed tuberculosis and the patient was referred to a rehabilitation clinic. However, she was re-examined in a state insurance hospital and tuberculosis was excluded. The treatment was stopped and she was then referred to our rehabilitation clinic on February 4, 2002.
Her history revealed that she had consumed unpasteurized dairy products (fresh feta cheese) 3 months before the onset of her symptoms. Her daughter and son-in-law had a history of brucellosis during this period. The patient had been suffering from intermittent fevers, malodorous night sweats, anorexia, fatigue, and a 10 kg weight loss.
Her physical examination was remarkable for low-grade fever without splenomegaly, hepatomegaly, or lymphadenopathy. All the joints were normal. She had exaggerated thoracic kyphosis with tenderness over the lower cervical and upper thoracic spine.
Neurological examination revealed hyperactive patellar and achilles reflexes, bilaterally positive Babinski reflexes, normal proprioception, hypoesthesia below the T6 dermatome, and muscle weakness in the lower limbs. She was unable to stand. The anal reflex, bulbocavernous reflex, anal sensation, and voluntary anal contraction were intact. She had an indwelling urethral catheter. Her neurological findings were consistent with T1 incomplete paraplegia (ASIA D Impairment Scale). Total functional independence measure (FIM) score was 47 (motor FIM score: 14, cognitive FIM score: 33).
Laboratory evaluation revealed normal complete blood cell count, blood biochemistry, and urine analysis. The erythrocyte sedimentation rate was 26 mm/first hour and the C-reactive protein (CRP) was 19.5 mg/l. The blood brucella Wright titer was found to be 1/160. The Rose Bengal test was positive, and the brucella antihuman globulin T titer was 1/640. Blood cultures were negative.
X-ray of the thoracic spine demonstrated kyphosis of the spine, narrowing of the T3–4 disc space, and degenerative changes of the vertebrae. MRI findings were unchanged from the first MRI obtained months earlier. Gadolinium revealed enhancement of the involved discs and paravertebral soft-tissue mass only (Figure 3).
Technetium bone scanning demonstrated increased uptake at the affected thoracic spinal regions, sternoclavicular joint, and right patellar bone.
The patient was diagnosed with brucellosis and treated with oral doxycycline 100 mg BID, rifampicin 600 mg/day, and ciprofloxacin 500 BID, on March 1, 2002. She was transferred to a rehabilitation unit for her paraparesis and bowel and bladder incontinence. At that point, urodynamic examination demonstrated normal capacity, detrusor pressure, and bladder compliance. Despite the sensation of fullness, she was unable to initiate micturation, so intermittent catheterization was recommended.
The patient was also evaluated by a neurologist to rule out neurobrucellosis. Lumbar puncture demonstrated clear cerebrospinal fluid with a normal cell count, mildly elevated levels of protein, albumin, and IgG. Brucella Rose Bengal, Wright, IgM 2-ME, and CSF culture were negative. These results excluded neurobrucellosis (see below).
After 5 months of antibiotics, the sweating, fever, and anorexia resolved. The CRP returned to normal (0.29 mg/l). Blood brucella Wright and antihumanglobulin T only titer levels decreased to 1/40. Rose Bengal test was positive. No adverse reaction was observed due to medical treatment. Her lower limb weakness improved to the point that she could walk and even climb stairs with the help of a cane. Her urinary retention and fecal incontinence also resolved. The total FIM score increased to 103 (motor FIM score: 68, cognitive FIM score: 35).
Subsequent MRI demonstrated that the previous findings remained fairly unchanged; however, there was a slight regression of the paraspinal soft-tissue mass. Antibiotics were stopped at 6 months. The patient continues to be followed up at our clinic.
Discussion
Osteoarticular disease is the most common complication of brucellosis and is found in approximately one-third of patients. The spectrum of involvement depends on the patient's age and brucella species. Involvement of the spine usually occurs in the elderly and is either focal or diffuse, with a predilection to the lumbar region,1,2 although the cervical or thoracic involvement is frequently associated with more neurological deficits. Clinical and radiological diagnoses of brucellar spondylitis may be difficult, since brucellar spondylitis may resemble many diseases that affect the spine, such as tuberculosis, pyogenic osteomyelitis, intervertebral disc herniation, and malignancy.5,6,7 Delayed diagnosis leads to increased morbidity. In our case, the delay in diagnosis was 6 months due to misdiagnosis of malignancy, tuberculosis, and pneumonia. Her back pain was initially attributed to pneumonia; however, back pain is the leading symptom in most patients with infectious spondylitis.8 A detailed initial history would have revealed that her daughter and son-in-law were diagnosed with brucellosis. Furthermore, brucellosis should have been considered primarily since it is endemic in our country.2
In all cases of spondylitis, a thorough search for neurobrucellosis should be made.9 Diagnosis is made on the basis of history of the exposure to brucella, of serum and cerebrospinal fluid positive serology, of quantitative change in cerebrospinal fluid, on EEG, CT, and MRI. Neurobrucellosis is the second most common complication of brucellosis and includes acute meningitis, meningoencephalitis, cerebellitis, and myelopathy. Neurobrucellosis requires a longer treatment duration (18–24 months).10
The treatment of brucellosis is controversial. The World Health Organization has recommended a combination of doxycycline, and rifampicin for 6 weeks,1 but this combination has been proven to be less effective than doxycycline and streptomycin.11 Recently, fluoroquinolones1 have also been recommended. The duration of treatment is longer in patients with spondylitis than in patients without spondylitis. The treatment duration varies from 6 weeks to 6 months.1,12
As a conclusion, particularly in endemic regions such as our country, brucellar spondylitis should be kept in mind in the differential diagnosis in elderly patients with back pain and constitutional symptoms. An early diagnosis will prevent the development of more severe complications such as spinal cord compression.
References
Salata RA . Brucellosis. In: Bennett JC, Plum F (eds). Textbook of Medicine, 20th edn WB Saunders: Philadelphia, 1996. pp, 1678–1682.
Tasova Y, Saltoglu N, Sahin G, Aksu HSZ . Osteoarticular involvement of brucellosis in Turkey. Clin Rheumatol 1999; 18: 214–219.
Lifeso RM, Harder E, Mc Corkell . Spinal brucellosis. J Bone Joint Surg 1985; 67: 345–351.
Sankaran-Kutty M, Marwah S, Kutty MK . The skeletal manifestations of brucellosis. Int Orthop 1991; 15: 17–19.
Ozates M et al. Lumbar epidural brucellar abscess causing nerve root compression. Spinal Cord 1999; 37: 448–449.
Sharif HS et al. Brucellar and tuberculosis spondylitis: comparative imaging features. Radiology 1989; 171: 419–425.
Harman M et al. Brucellar spondylodiscitis MRI diagnosis. Clin Imaging 2001; 25: 421–427.
Stabler A, Reiser MF . Imaging of spinal infection. Radiol Clin North Am 2001; 39: 115–135.
Mousa AM et al. Neurological complications of brucella spondylitis. Acta Neurol Scand 1990; 81: 16–23.
Bingol A, Yucemen N, Meco O . Medically treated intraspinal brucella granuloma. Surg Neurol 1999; 52: 570–576.
Ariza J et al. Treatment of human brucellosis with doxycycline plus rifampin or doxycycline plus streptomycin. Ann Intern Med 1992; 117: 25–30.
Nas K et al. Management of spinal brucellosis and outcome of rehabilitation. Spinal Cord 2001; 39: 223–227.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sonel Tur, B., Suldur, N., Ataman, S. et al. Brucellar spondylitis: a rare cause of spinal cord compression. Spinal Cord 42, 321–324 (2004). https://doi.org/10.1038/sj.sc.3101571
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101571
Keywords
This article is cited by
-
Noncontiguous multifocal Brucella spondylodiscitis with paravertebral abscess: a case report
Journal of Medical Case Reports (2022)
-
Spinal brucellosis: Turkish experience based on 452 cases published during the last century
Acta Neurochirurgica (2006)
-
Could remembering the prozone phenomenon shorten our diagnostic journey in brucellosis? A case of Brucella spondylodiscitis
Rheumatology International (2006)