Abstract
Purpose
Retinal neovascularization in diabetes has been thought to follow the release of local angiogenic factors in the retina. We hypothesize that neovascularization of diabetic retinopathy is a systemic vasculogenesis rather than a local angiogenesis. Thus, we evaluate the concentrations of circulating endothelial progenitor cells (EPCs) and stem cell modulation factors such as vascular endothelial growth factor (VEGF), erythropoietin (Epo), and substance p (SP) in the peripheral blood of diabetic retinopathy patients.
Methods
We studied 15 normal controls and 45 type II diabetic patients (no DR group (n=15), NPDR group (n=15), and PDR group (n=15)). We measured circulating CD34+mononuclear cells (CD34+MNCs), c-Kit+mononuclear cells (c-Kit+MNCs) by flow cytometry. VEGF, Epo, and SP in the peripheral blood were measured by ELISA.
Results
The circulating CD34+MNCs and c-Kit+MNCs increased in the NPDR and PDR groups compared with the control group (P<0.01). Serum level of VEGF increased in the NPDR and PDR groups compared with the control group (P<0.05). The level of Epo elevated exclusively in the no DR group compared with the other three groups (P<0.01). Circulating SP level increased in the NPDR and PDR groups compared with the control group (P<0.05). SP and CD34+MNCs were shown to have increased correlation according to the diabetic retinopathy in the NPDR and PDR groups (r=0.440, P<0.05 and r=0.460, P<0.05, respectively).
Conclusions
The present study is the first to demonstrate that CD34+MNCs, c-Kit+MNCs and their modulator are elevated in diabetic retinopathy patients. Therefore, it is possible that circulating EPCs and serum Epo, VEGF, and SP may be involved in the progression of diabetic retinopathy.
Similar content being viewed by others
Introduction
New vessel formation in diabetic retinopathy causes visual loss with vitreous haemorrhage, retinal detachment, and neovascular glaucoma.1, 2 Retinal neovascularization has been thought to occur due to the release of local angiogenic factors by ischaemic and hypoxic retina.3 Increased local expression of vascular endothelial growth factor (VEGF) has drawn much attention relating to the pathogenesis of diabetic retinopathy. Evidences suggest that VEGF, a cytokine that acts as an endothelial cell mitogen,4, 5 and induces increased microvascular permeability,6 is causally involved in the development of diabetic retinopathy.7, 8
Although intraocular levels of VEGF have been studied extensively, systemic vasculogenic factors have not been fully evaluated in previous studies. In particular, there appears to be a lack of strong association between systemic vasculogenic factors and diabetic retinopathy.
Recent studies have demonstrated that circulating endothelial progenitor cells (EPCs) go to the sites of neovascularization and differentiate into endothelial cell in situ in a manner consistent with a process termed postnatal vasculogenesis.9, 10, 11, 12 EPCs are characterized by CD34, Flk-1, and CD133 antigen-positive cells,13, 14 and these cells are localized predominantly in the bone marrow.15 In the peripheral circulation of adults, more mature, differentiated EPCs are found that are characterized by a decreased expression of CD133, are positive for VEGFR-2, and still express CD34. EPCs circulate in adult peripheral blood and contribute to neovascularization, and their putative precursor, CD34+monocuclear cells (CD34+MNCs) increase in acute ischaemic events in human.12 These EPCs are derived from adult bone marrow, and are known to be stimulated by several modulators such as VEGF, erythropoietin (Epo), substance P (SP), etc.9, 16, 17
Sublethal hypoxia induces upregulation and nuclear translocation of hypoxia-inducible factor, whose target gene is Epo.18, 19, 20, 21 Epo stimulates postnatal neovascularization at least in part by enhancing mobilization of EPCs from the bone marrow.22, 23 Epo is also known to enhance mobilization of EPCs from bone marrow and maintain normal endothelial differentiation of retina on ischemic tissue to help the wound healing process.22
Another modulating factor constitutes SP, which is a neuropeptide that could be released in the bone marrow in the ischaemic condition. SP interacts with specific receptors on resident cells in the bone marrow to modulate immune and haematopoietic functions.24, 25, 26 SP also has the same endothelial cell migratory effect at similar dosages as has VEGF, and induces vasoproliferation in vivo; that is, it has a vascular growth factor potential.27
With this background, we hypothesize that neovascularization of diabetic retinopathy is a systemic vasculogenesis rather than a local angiogenesis, and EPCs and other stem cell modulators may be involved in the pathogenesis of diabetic retinopathy. We investigated whether circulating EPC precursors (CD34+MNCs, c-Kit+MNCs) and other modulators (Epo, VEGF, SP) are changed with the progression of diabetic retinopathy, and tried to elucidate which vasculogenic factor is correlated with diabetic retinopathy.
Method
Study participants
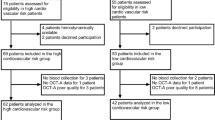
We studied 45 type II diabetic patients and 15 age- and sex-matched normal controls. To prevent confusion with other systemic hypoxic conditions, patients were excluded if they had undergone prior ocular and cardiac surgery or had a history of ischaemic cardiovascular disease (except hypertension), administration of statin or angiotensin-converting enzyme inhibitor, haematologic disorder, malignant disease, and human recombinant erythropoietin treatment that might influence EPC kinetics.15, 28, 29 Plasma fasting glucose, low-density lipoprotein cholesterol (LDL-C), and glycosylated haemoglobin (HbA1c) levels were assessed in all participants to address whether their blood glucose was controlled or not. All procedures were performed under the tenets of the Helsinki declaration and informed consent was obtained from all patients.
Grading procedure of diabetic retinopathy
Diabetic patients were classified into three groups according to the modified ETDRS retinopathy severity scale.30 No DR group (n=15) signifies no definite retinopathy in diabetic patients, NPDR group (n=15) signifies nonproliferative diabetic retinopathy, and PDR group (n=15) signifies proliferative diabetic retinopathy. Severity of diabetic retinopathy was confirmed by standardized fundus colour photography and fluorescein angiography.
Sample collection
Venous blood was collected from the antecubital vein and flow cytometric analysis was performed within 1 h of sample collection. For ELISA, samples were centrifuged at 3000 g for 5 min to obtain serum and then stored in a deep freezer at −70°C until they were assayed.
Measurement of circulating progenitor cells
Enumeration of CD34+MNCs, stained with a reagent kit (ProCOUNT, BD) was measured by flow cytometer (FACSCalibur, BD).
Peripheral blood c-Kit+cells were identified by their distinct pattern of surface markers. C-Kit+cells were measured using c-Kit monoclonal antibody (BD Phamigen) by the double-colour immunofluorescence technique.
Measurement of systemic vasculogenic factors
Serum levels of VEGF, Epo, and SP were measured with ELISA using human VEGF, Epo, and SP ELISA Kit (all from R&D Systems, Minneapolis, MN, USA). All procedures were performed following the instruction manuals.
Statistical analysis
Statistical analysis was performed with SAS statistical software (SAS Institute Inc., Cary, NC, USA). The differences among the groups were assessed by ANOVA followed by Duncan's multiple range test.31 Correlations between two variables were calculated by linear regression analysis. P-value <0.05 was considered to be significant.
Result
Demographic data of three diabetic groups
The data for age, sex ratio, and diabetes duration are shown as means in Table 1. There was no significant difference in age among the three groups of diabetic patients and the control group. The mean diabetes duration of 16.0±6.0 years for the PDR patients was significantly longer than that for the NPDR and the no DR patients (11.3±6.6, 4.8±2.3, respectively; P=0.02).
The mean fasting blood sugar (FBS) of the no DR patients (98.8±7.0) was significantly lower than that of the NPDR and PDR groups (133.7±21.3 and 143.2±34.5, respectively; P=0.013). No significant differences were found in the prevalence of hypertension, atherosclerotic cardiovascular disease, lipid profiles (esp. LDL-C), and HbA1c level.
Circulating progenitor cells in diabetic retinopathy
Table 2 shows levels of circulating CD34+MNCs and c-Kit+MNCs in each group. The circulating CD34+MNCs count gradually increased with diabetic retinopathy progression. Compared with the control group, the level of CD34+MNCs significantly increased in the NPDR and PDR groups (P<0.05 and <0.001, respectively). Of the three DR groups, the level of CD34+MNCs in the PDR group was significantly higher than that in the no DR group. C-Kit+MNCs, which reflects the total stem cell count including haematopoietic and endothelial lineage, significantly increased in the NPDR and PDR groups when compared with the control and no DR group (P<0.0001). However, in the PDR group, c-Kit+MNCs decreased slightly compared to the NPDR group.
Systemic vasculogenic factors affecting mobilization of EPCs in diabetic retinopathy
Table 3 shows levels of serum VEGF, Epo, and SP in the control, no DR, NPDR, and PDR groups. Serum level of VEGF increased in the NPDR and PDR groups compared with the control group (P<0.05). However, the level of VEGF among the three DR groups did not show a significant difference. Epo was exclusively elevated in the no DR group compared with the control group (P<0.001). In the NPDR and PDR groups, Epo level showed no significant difference from that of the control group. There was a trend towards increasing serum SP level with the progression of diabetic retinopathy (P<0.05). Especially, compared with the control group, the level of SP in the NPDR and PDR groups significantly increased.
Correlation between vasculogenic factors and endothelial progenitor cells
To identify the relationship between factors in diabetic retinopathy progression, we performed a correlation test in three DR groups. There was no correlation between VEGF and EPCs. Epo was significantly correlated with CD34+MNCs only in the NPDR group (r=0.6085, P<0.05). SP was significantly correlated with CD34+MNCs in the NPDR and PDR groups (r=0.440, P<0.05 and r=0.460, P<0.05, respectively). VEGF level was inversely correlated with Epo level in the PDR group (r=−0.61196, P<0.05), but did not correlate with other parameters (data not shown).
Discussion
In this study, we found that circulating endothelial precursor cells (CD34+MNCs) were increased in the NPDR and PDR groups compared with normal control. Similar results reported that vasculogenesis-related progenitor cells were increased in coronary heart diseases.12 Taken together with ours, these results suggest that retinal ischaemic signal may stimulate bone marrow by certain systemic factors that are diffused into systemic circulation, and CD34+MNCs were subsequently mobilized into peripheral blood and differentiated into endothelial cells on ischaemic foci. Even though these consequences of EPC elevation in diabetic patients are only speculative, our results have significance in the demonstration of EPC elevation in diabetic patients in vivo.
These results raise the question of whether elevated EPC levels in PDR patients play a beneficial role on ischaemic tissue or not. Previous reports demonstrated the therapeutic potential of EPC transplantation in animal models of hindlimb and myocardial ischaemia.12 However, EPC elevation seems to be less helpful or harmful to diabetic retinopathy. Tepper et al32 reported that diabetic EPCs exhibit alterations in functions important for blood vessel growth and may represent a mechanism by which diabetic EPCs are impaired in their ability to form collaterals. Neovascularization induced by altered EPCs may be structurally disorganized and insufficient for tissue oxygenation, thus elevated altered EPCs give rise to diabetic vascular complications. Based on this theory, we suggest that a supplement of normal healthy EPCs to the diabetic patients might prevent the progressive vascular changes.
Vascular endothelium as well as mesenchymal cells may be derived from bone marrow and contribute to organ regeneration and maintenance.9 C-Kit+MNCs reflect total stems, including mesenchymal stem cells. As the increase of c-Kit+MNCs was found to be less pronounced than that of CD34+MNCs in the PDR group, it might be speculated that an imbalance between endothelial and mesenchymal lineage cells cause excessive endothelial sprouting in the absence of mesenchymal architectural support. Thus, these vulnerable neovascularizations may lead to vitreous haemorrhage and release of angiogenic cytokines into the vitreous cavity.
Many of the diabetic patients who have impaired blood vessel growth after ischaemic events also have increased retinal neovascularization in diabetic retinopathy. This so-called ‘diabetic paradox’ is at present poorly understood.33, 34 We could presume a plausible solution for diabetic paradox via EPC dysfunction and imbalance of circulating stem cells.
In this study, VEGF significantly increased in the peripheral blood especially in the NPDR and PDR groups. However, VEGF level did not correlate with the severity of diabetic retinopathy. Similar results have reported that there was no difference in plasma immunoreactive VEGF level in type II diabetic patients,35 and they found no association of serum VEGF level with retinopathy status in a larger number of diabetic patients.36 Moreover, serum VEGF level did not correlate with CD34+MNCs and c-Kit+MNCs in this study, which suggests that other unrecognized factors could be present, affecting the initiation of neovascularization and modulation of EPCs in diabetic retinopathy.
Epo is known to enhance mobilization of EPCs from bone marrow and to maintain normal endothelial differentiation of the retina on ischaemic tissue.22 Epo in diabetic retinopathy was first described by Berman and Friedman.37 They reported three cases in which resorption of foveal hard exudates was observed after initiation of recombinant Epo treatment in anaemic patients. Friedman et al38 reported that an increased haematocrit, induced by Epo, might slow the progression of diabetic nephropathy and improve visual acuity because of resolution of macular oedema in diabetic retinopathy.
In this study, Epo was significantly elevated in the early diabetic group with normal fundus findings, and decreased in the NPDR and PDR groups. These results suggest that Epo may be upregulated in the early stage of ischaemic disorders to maintain homeostasis against progressive diabetic retinal vascular changes. Epo may act as an endogenous neuroprotective factor against ischaemic retinal disorder. However, vascular change may begin as Epo level decreases according to the renal dysfunction.
Epo level was positively correlated with CD34+MNCs count only in the NPDR group. This result may represent that Epo stimulates mobilization of EPCs from bone marrow in early diabetic retinopathy. Whether Epo administration to diabetic patients prevents progression of retinopathy, or whether Epo level may be used as a biologic indicator for early detection of diabetic retinopathy needs to be elucidated.
Another unrecognized factor may be SP, which has endothelial cell migratory effect,27 and induces vasoproliferation in vivo; that is, it has a vascular growth factor potential.39 Troger et al40 reported that SP acts as a proangiogenic signal; thus, if SP is reduced, neovascularization does not occur even though VEGF and its receptors are upregulated. This fact can account for our result that VEGF level in the PDR group is less elevated than in the NPDR group. Even though VEGF level is not increased, elevated SP (proangiogenic signal) may induce neovascularization. SP shows positive correlation with CD34+MNCs in the NPDR and PDR groups. We predict that SP may be responsible for transducing ischaemic signal, which is stimulated by ischaemic damage of the microangiopathic retina, and may upregulate other vasculogenic factors and EPCs to promote neovascularization in ischaemic tissue. However, EPCs in diabetes are altered in function and make vulnerable vasculatures, upregulation of vasculogenic factors do not abate ischaemic signal, and SP may sustain high levels especially in proliferative retinopathy patients.
Many studies have been performed to identify the association between intraocular level and peripheral blood level of vasculogenic factors.41, 42, 43, 44 Most of the results on VEGF showed a higher level in the vitreous than in the peripheral blood. However, there were few associations between intraocular level and peripheral blood level. In the case of Epo and SP, some reported that Epo and SP was elevated in the vitreous in inflammatory condition, but no studies were performed to confirm the association with systemic level. In the process of our study, we hypothesized that these vasculogenic factors increased in the eye diffuse into the systemic circulation and reach the target organ, bone marrow and stimulate EPC mobilization into systemic circulation.
There have been no studies that attempted to explain a progression of diabetic retinopathy incorporating vasculogenesis rather than just local angiogenesis. In this study, increased CD34+MNC and c-Kit+MNC levels suggest that circulating vasculogenic factors may play a role in the progression of diabetic retinopathy. The present study is the first to demonstrate that systemic vasculogenic factors are elevated in diabetic retinopathy patients. Therefore, it is possible that systemic circulating EPCs and serum Epo, VEGF, and SP may be involved in progression of diabetic retinopathy. However, the precise functional roles of EPCs and modulating factors in diabetic retinopathy should be determined further in an in vivo study. Identification of such vasculogenic triggering factor and detection of an early biologic marker for diabetic retinopathy may help us to prevent progression of neovascularization and lead to the development of other therapeutic approaches, in order to improve the outcome of patients with diabetic retinopathy.
References
Moss SE, Klein R, Klein BE . Ten-year incidence of visual loss in a diabetic population. Ophthalmology 1994; 101: 1061–1070.
Moss SE, Klein R, Klein BE . The 14-year incidence of visual loss in diabetic population. Ophthalmology 1998; 105: 998–1003.
Frank RN . On the pathogenesis of diabetic retinopathy. A 1990 update. Ophthalmology 1991; 98: 586–593.
Keck PJ, Hauser SD, Krivi G, Sanzo K, Warren T, Feder J et al. Vascular permeability factor, an endothelial cell mitogen related to PDGF. Science 1989; 246: 1309–1312.
Leung DW, Cachianes G, Kuang WJ, Goeddel DV, Ferrara N . Vascular endothelial growth factor is a secreted angiogenic mitogen. Science 1989; 246: 1306–1309.
Senger DR, Galli SJ, Dvorak AM, Perruzzi CA, Harvey VS, Dvorak HF . Tumor cells secrete a vascular permeability factor that promotes accumulation of ascities fluid. Science 1983; 219: 983–985.
Hideharu F . Relationship between vascular endothelial growth factor and interleukin-6 in diabetic retinopathy. Retina 2001; 21: 469–477.
Shimada K, Baba T, Neugebauer S, Onozaki A, Yamada D, Midorikawa S et al. Plasma vascular endothelial growth factor in Japanese Type 2 diabetic patients with and without nephropathy. J Diabetes Complications 2002; 16: 386–390.
Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, Silver M et al. Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res 1999; 85: 221–228.
Kalka C, Tehrani H, Laudenberg B, Vale PR, Isner JM, Asahara T et al. VEGF gene transfer mobilizes endothelial progenitor cells in patients with inoperative coronary disease. Ann Thorac Surg 2000; 70: 829–834.
Lee SH, Wolf PL, Escudero R, Deutsch R, Jamieson SW, Thistlethwaite PA . Early expression of angiogenesis factors in acute myocardial ischemia and infarction. N Eng J Med 2000; 342: 626–633.
Shintani S, Murohara T, Ikeda H, Ueno T, Honma T, Katoh A et al. Mobilization of endothelial progenitor cells in patients with acute myocardial infarction. Circulation 2001; 103 (23): 2776–2779.
Gehling UM, Ergun S, Schumacher U, Wagener C, Pantel K, Otte M et al. In vitro differentiation of endothelial cells from AC133-positive progenitor cells. Blood 2000; 95 (10): 3106–3112.
Peichev M, Naiyer AJ, Pereira D, Zhu Z, Lane WJ, Williams M et al. Expression of VEGFR-2 and AC133 by circulating human CD34(+) cells identifies a population of functional endothelial precursors. Blood 2000; 95 (3): 952–958.
Gill M, Dias S, Hattori K, Rivera ML, Hicklin D, Witte L et al. Vascular trauma induces rapid but transient mobilization of VEGFR2(+)AC133(+) endothelial precursor cells. Circ Res 2001; 88: 167–174.
Takahashi T, Kalka C, Masuda H, Chen D, Silver M, Kearney M et al. Ischemia and cytokine induced mobilization of bone marrow derived endothelial progenitor cells for neovascularization. Nat Med 1999; 5: 434–438.
Shi Q, Rafii S, Wu MH, Wijelath ES, Yu C, Ishida A et al. Evidence for circulating bone marrow-derived endothelial cells. Blood 1998; 92: 362–367.
Grimm C, Wenzel A, Groszer M, Mayser H, Seeliger M, Samardzija M et al. HIF-1-induced erythropoietin in the hypoxic retina protects against light-induced retinal degeneration. Nat Med 2002; 8: 718–724.
Cai Z, Manalo DJ, Wei G, Rodriguez ER, Fox-Talbot K, Lu H et al. Hearts from rodents exposed to intermittent hypoxia or erythropoietin are protected against ischemia–reperfusion injury. Circulation 2003; 108 (1): 79–85.
Bernaudin M, Nedelec AS, Divoux D, MacKenzie ET, Petit E, Schumann-Bard P . Normobaric hypoxia induces tolerance to focal permanent cerebral ischemia in association with an increased expression of hypoxia-inducible factor-1 and its target genes, erythropoietin and VEGF, in the adult mouse brain. J Cereb Blood Flow Metab 2002; 22 (4): 393–403.
Ruscher K, Freyer D, Karsch M, Isaev N, Megow D, Sawitzki B et al. Erythropoietin is a paracrine mediator of ischemic tolerance in the brain: evidence from an in vitro model. J Neurosci 2002; 22 (23): 10291–10301.
Heeschen C, Aicher A, Lehmann R, Fichtlscherer S, Vasa M, Urbich C et al. Erythropoietin is a potent physiologic stimulus for endothelial progenitor cell mobilization. Blood 2003; 102 (4): 1340–1346.
Zhao ZC, Jing-Qiong K, Kenneth A . Angiogenesis and plasticity: role of erythropoietin in vascular system. J Hematother Stem Cell Res 2002; 11: 863–871.
Bost KL, Pascual DW . Substance P. A late-acting B lymphocyte differentiation cofactor. Am J Physiol 1992; 262 (3 Part 1): C537–C545.
Ho WZ, Lai JP, Zhu XH, Uvaydova M, Douglas SD . Human monocytes and macrophages express substance P and neurokinin-1 receptor. J Immunol 1997; 159 (11): 5654–5660.
Hiramoto M, Aizawa S, Iwase O, Nakano M, Toyama K, Hoque M et al. Stimulatory effects of substance P on CD34 positive cell proliferation and differentiation in vitro are mediated by the modulation of stromal cell function. Int J Mol Med 1998; 1 (2): 347–354.
Ziche M, Morbidelli L, Geppetti P, Maggi CA, Dolara P . Substance P induces migration of capillary endothelial cells: a novel NK-1 selective receptor mediated activity. Life Sci 1991; 48 (2): PL7–PL11.
Walter DH, Zeiher AM, Dimmeler S . Effects of statins on endothelium and their contribution to neovascularization by mobilization of endothelial progenitor cells. Coron Artery Dis 2004; 15 (5): 235–242.
Marusic-Vrsalovic M, Dominis M, Jaksic B, Kusec R . Angiotensin I-converting enzyme is expressed by erythropoietic cells of normal and myeloproliferative bone marrow. Br J Haematol 2003; 123 (3): 539–541.
Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs-an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology 1991; 98 (5 Suppl): 786–806.
Duncan DB . Multiple range and multiple F tests. Biometrics 1955; 11: 1–42.
Tepper OM, Galiano RD, Capla JM, Kalka C, Gagne PJ, Jacobowitz GR et al. Human endothelial progenitor cells from type II diabetics exhibit impaired proliferation, adhesion, and incorporation into vascular structures. Circulation 2002; 106 (22): 2781–2786.
Duh E, Aiello LP . Vascular endothelial growth factor and diabetes: the agonist versus antagonist paradox. Diabetes 1999; 48 (10): 1899–1906.
Waltenberger J . Impaired collateral vessel development in diabetes: potential cellular mechanisms and therapeutic implications. Cardiovasc Res 2001; 49 (3): 554–560.
Wasada T, Kawahara R, Katsumori K, Naruse M, Omori Y . Plasma concentration of immunoreactive vascular endothelial growth factor and its relation to smoking. Metabolism 1998; 47 (1): 27–30.
Chaturvedi N, Fuller JH, Pokras F, Rottiers R, Papazoglou N, Aiello LP . Circulating plasma vascular endothelial growth factor and microvascular complications of type 1 diabetes mellitus: the influence of ACE inhibition. Diabet Med 2001; 18 (4): 288–294.
Berman DH, Friedman EA . Partial absorption of hard exudates in patients with diabetic end-stage renal disease and severe anemia after treatment with erythropoietin. Retina 1994; 14 (1): 1–5.
Friedman EA, Brown CD, Berman DH . Erythropoietin in diabetic macular edema and renal insufficiency. Am J Kidney Dis 1995; 26 (1): 202–208.
Ziche M, Morbidelli L, Pacini M, Geppetti P, Alessandri G, Maggi CA . Substance P stimulates neovascularization in vivo and proliferation of cultured endothelial cells. Microvasc Res 1990; 40 (2): 264–278.
Troger J, Neyer S, Heufler C, Huemer H, Schmid E, Griesser U et al. Substance P and vasoactive intestinal polypeptide in the streptozotocin-induced diabetic rat retina. Invest Ophthalmol Vis Sci 2001; 42 (5): 1045–1050.
Burgos R, Simo R, Audi L, Mateo C, Mesa J, Garcia-Ramirez M et al. Vitreous levels of vascular endothelial growth factor are not influenced by its serum concentrations in diabetic retinopathy. Diabetologia 1997; 40 (9): 1107–1109.
Deng J, Wu DZ, Gao R . Elevated vascular endothelial growth factor levels in the vitreous of patients with proliferative diabetic retinopathy. Yan Ke Xue Bao 1999; 15 (1): 17–21.
Noma H, Funatsu H, Yamashita H, Kitano S, Mishima HK, Hori S . Regulation of angiogenesis in diabetic retinopathy: possible balance between vascular endothelial growth factor and endostatin. Arch Ophthalmol 2002; 120 (8): 1075–1080.
Hernandez C, Lecube A, Segura RM, Sararols L, Simo R . Nitric oxide and vascular endothelial growth factor concentrations are increased but not related in vitreous fluid of patients with proliferative diabetic retinopathy. Diabet Med 2002; 19 (8): 655–660.
Acknowledgements
We thank J Kim for critically reading the manuscript and A Park for technical support. This study was supported in part by research funds from the Research Institute for Biochemical and Pharmaceutical Science, by Chung-Ang University and in part by research funds from the Ministry of Commerce, Industry and Energy, Republic of Korea.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, I., Chae, S. & Kim, J. Involvement of circulating endothelial progenitor cells and vasculogenic factors in the pathogenesis of diabetic retinopathy. Eye 20, 546–552 (2006). https://doi.org/10.1038/sj.eye.6701920
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701920
Keywords
This article is cited by
-
Endothelial progenitor cells as biomarkers of diabetes-related cardiovascular complications
Stem Cell Research & Therapy (2023)
-
Serum and vitreous vascular endothelial growth factor levels in diabetic retinopathy
International Ophthalmology (2022)
-
Fenofibrate increases circulating haematopoietic stem cells in people with diabetic retinopathy: a randomised, placebo-controlled trial
Diabetologia (2021)
-
Serum erythropoietin concentration and its correlation with stage of diabetic retinopathy
BMC Ophthalmology (2019)
-
KC21 Peptide Inhibits Angiogenesis and Attenuates Hypoxia-Induced Retinopathy
Journal of Cardiovascular Translational Research (2019)