Key Points
-
This article highlights some of the challenges facing NHS Dental Reform models.
-
Explores the current status of the Pilot and Prototype schemes, and alignment with their original aims and objectives.
-
Identifies possible challenges for those practices exiting the Pilot Schemes.
Abstract
This article covers the move forwards from pilot to prototype in the National Health Service (NHS) dental contract reform in England. The current status of the pilot and prototype schemes are summarised and some of the challenges for those practices who will be exiting the pilots discussed.
Similar content being viewed by others
Introduction
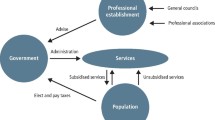
The Dental Contract Reform Group (UK Department of Health), state that dental access has increased by 1.5 million since 2010.1 This group also acknowledges that the current units of dental activity (UDA) system of remunerating dentists is focused on treatment and repair, with little emphasis on preventive approaches. Since 2011, the Department of Health (DH) have piloted NHS dental reform models based on patient care pathways, a quality and outcomes framework, and with a renewed interest in capitation and prevention. Following on from these pilots, the prototypes are intended to focus on remuneration for continued care (through capitation arrangements), prevention and activity-based systems in synergy with alignment of clinical and financial incentives.
In early 2015, the DH announced that 62 practices will move forwards to the prototype model, with additional practices (believed to be about 30 in number) to be announced at a later date. The DH are adopting a phased approach with the extension of the Capitation and Quality Scheme 2 regulations until 31 March 2016. Prototype rollout is expected by autumn 2015, with a reformed contract anticipated in 2018/19. Pilots and prototypes have both evolved data capture2,3 and engagement reports.4,5 The main differences between the pilots and the prototypes are outlined in Table 1.
This article discusses the move forwards from pilot to prototype in dentistry in England, and some of the challenges for those practices who will be exiting the pilots.
The prototypes
The prototype model encompasses UDAs, a series of Dental Quality Outcome Framework (DQOF) indicators, clinical effectiveness, capitation payments, and patient satisfaction data, all following on from the pilot pathway approach to dental service delivery. However, the pathway may be overridden by the clinician's decision based upon clinical need. The prototypes will continue to work towards providing equitable dental service delivery, increasing access and oral health.
The prototypes will test the remuneration system of the final reform. They will adopt a blended approach with blend A encompassing capitation and prevention oral health reviews, with UDA activity assigned to band 2 and 3 items of treatment (UDA remuneration). Blend B is similar to blend A, but assigns UDA activity remuneration to band 3 items of treatment only. There will be emphasis on patient home care, under the advice of the treating clinician.6 Capitation elements will be based upon a weighted system, prioritised by patient age and deprivation system (against national capitation values). However, oral health needs must be assessed on an individual basis, given today's transient population groups and widespread demographics. The question is will the capitation system lead to the reduction in health inequalities, increase access to dental care and refocus on quality?
Quality
Quality was historically described by Avedis Donebedian in 1966, and this model draws information on healthcare quality from three elements: structure, process and outcomes.7 Previous NHS systems have encompassed structure and process in terms of clinical governance frameworks, contractor audits, continued professional development and increasing regulation. The renewed focus is around the 'outcome' element, with a focus on the patient experience. As patient satisfaction is a highly subjective area, open to individual interpretation, and reliant upon data received for analysis, the validity of this as a true indicator of quality and successful service provision must be questioned.
The UDA-target-based remuneration system in dentistry has led to difficulties in contract management and service delivery, where numbers inevitably take precedent over quality of treatment and service delivery. This has been identified as cause for concern by many organisations and the profession itself, as such systems demonstrate diminished quality. This contributed to the launch of Professor Jimmy Steele's Independent Review of NHS Dentistry, with pilots formed on the findings of his further review in 2009.8
However, the UDA system is set to remain, contributing towards the anticipated remuneration in the prototype reform models, with up to 10% based upon DQOFs of clinical effectiveness (caries and periodontal health measures), best practice, patient experience, safety, and data quality. DQOFs are now intended to be integrated as best practice measures and encompass NICE guideline recall intervals9 and the Delivering better oral health document.10 Concerns still remain across the profession regarding the activity based system of remuneration.11
Discussion
Lessons learned from the pilots have steered reform towards risk assessments of treatment needs, with complex dentistry only being provided under NHS arrangements when patients demonstrate adequate oral and dental fitness and self-care. This increases the likelihood of patient complaints arising from those patients where complex treatment is declined due to their risk assessment outcomes. There are concerns that clinicians would override the assessment system in order to provide such treatment to prevent patient complaints, given that an element of the contract remuneration relies on patient satisfaction. Clinician concerns arise from the medico-legal aspect of accepting or declining the pathway, balancing patient management, clinical need, care pathways and evidence-based dentistry, all benchmarked against DQOFs. It is pertinent the dental profession agree on who defines the DQOF benchmarks and quality, and also agree on the gold standard parameters set. Deviation from the care pathway requires skill and enhanced pathway understanding, not always supported by the IT software capturing data for pilot analysis.
The pilot data have also identified a decrease in treatment provided, an area worthy of further investigation given the proposed strategic aims of increased access, increased oral health and the reduction of health inequalities are key drivers of the intended reforms. The introduction of weighted capitation may impact further upon such drivers.
Interim care management (ICM) appointments for preventive dental intervention (based upon risk assessments), seem a logical step forward in principal. However, the fundamental patient management challenges do not seem to have been addressed sufficiently, with many patients declining ICM appointments with dental care professionals (DCPs) or extended duty nurses (EDNs), opting to wait until emergency/scheduled appointments with the dentist are required. Clearly, the intended pathway of the pilots has proven somewhat of a meander, all be it with lessons learned in order to refine certain aspects within the prototype models. Patient factors and attendance patterns also require further investigation, with 'failed to attend' appointments impacting heavily upon NHS resources.
Current challenges for selected prototype practices
For those practices moving forwards to prototypes, challenges exist in patient education, revised software and reporting systems, and increased risk of reducing patient access, as already demonstrated in the pilot schemes.
Current challenges for non-selected prototype practices
For those pilot practices that have not been selected to go forwards to the prototypes, the challenges are around increasing access to dental care to regain the original patient list size within the three-month notice period given to many pilot practices. Although the contracts will be based upon prior pilot activity, concerns remain that a diminished patient base will not be able to support the reverted UDA activity. Indeed, access has been one of the main defining entities in prototype selection.
Additional challenges relate to re-education of pilot dentists back into the current UDA system. Dentists who participated in the pilot scheme will require redirection of focus which will inevitably require time and resources in order to re-educate clinicians back into the NHS UDA system, a factor which seems to have been somewhat overlooked in the current transformational pathway of pilot to prototype. These factors may perhaps lead to claw-backs and underperformance issues at year end of reversion.
Workforce issues may also arise for those who embraced hygienists and other DCPs to deliver the preventive aspects of the pathway (ICMs), discouraging the skill-mix, which was created to run the pilots efficiently, based on remuneration factors.
Potential practice purchasers will need to exercise extreme due diligence, with attention to details such as active patient numbers, UDAs and DQOFs. Such information would need to be provided upon the sale of a practice, with additional clauses included in contracts of sale.
Conclusion
Although there are positive elements to the NHS dental reforms, the impact upon individual businesses and their patients may be varied and indeterminate. The ultimate aim in any healthcare system is to demonstrate value for money and financial sustainability, satisfying all stakeholders' strategic goals, aims, and objectives. Dentistry is no different in striving to provide safe, effective, efficient, equitable, quality dental services, appropriate to the needs of its population. However, while the target-based, systems approach remains integral to the proposed reforms, with little united definition of 'quality', it is unclear as to how successful the reforms will prove.
In many aspects dentistry seems to follow the general medical models, with limited successful transposition into the dental arena. Although the prototypes will test further proposals, some with renewed interest of older NHS dental models, the horizon remains somewhat hazy.
References
Health & Social Care Information Centre. NHS Dental Statistics for England, 2014-15. First quarterly report. 20 Nov 2014. Available online at http://www.hscic.gov.uk/article/2021/Website-Search?productid=16410&q=NHS+DENTAL+STATISTICS+FOR+ENGLAND&sort=Relevance&size=10&page=1&area=both#top (acessed 9 June 2015).
DH Dental & eye care services. NHS dental contract pilots - Early findings. Oct, 2012. Available online at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/212999/NHS-dental-contract-pilots-early-findings.pdf (accessed June 2015).
Steele J, Department of Health. NHS dental contract pilots – Learning after first two years of piloting, October 2012. Feb, 2014. Available online at https://www.gov.uk/government/publications/dental-contract-pilots-evidence-and-learning (accessed June 2015).
Dental contract reform programme: Engagement Exercise 2014. Available online at https://www.gov.uk/government/consultations/improving-dental-contracts (accessed June 2015).
Dental contract reform engagement exercise early findings. Available online at http://www.pcc-cic.org.uk/article/dental-contract-reform-engagement-exercise-early-findings (accessed June 2015).
NHS England. NHS Five Year Forward View: NHS England Business Plan 2015-2016. 2015. Available online at http://www.england.nhs.uk/wp-content/uploads/2015/03/business-plan-mar15.pdf (accessed June 2015).
Donabedian A. The quality of care: How can it be assessed? JAMA 1988; 260: 1743–1748.
Steele J, Clarke J, Rooney E, Wilson T . NHS dental services in England – an independent review. June 2009 Available online at http://www.sigwales.org/wp-content/uploads/dh_101180.pdf (accessed June 2015).
National Institute for Health and Care Excellence. NICE Guideline CG19. Dental Recall – Recall intervals between routine dental examinations. NICE, 2004. Available online at http://guidance.nice.org.uk/CG19 (accessed June 2015).
Public Health England. Delivering better oral health: an evidence based tool kit for prevention. 3rd edition. London: Public Health England. Available online at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/367563/DBOHv32014OCTMainDocument_3.pdf (accessed June 2015).
Henrik Overgaard-Nielsen (Chair of the BDA's General Dental Practice Committee). Press release. Available online at https://www.bda.org/news-centre/press-releases/bda-response-to-launch-of-dental-prototypes (accessed June 2015).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Woodington, J. Challenges facing NHS dental contract reforms: Pilot exit. Br Dent J 218, 695–697 (2015). https://doi.org/10.1038/sj.bdj.2015.441
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.441
This article is cited by
-
Exploring dentists' professional behaviours reported in United Kingdom newspaper media
British Dental Journal (2020)
-
Does capitation affect the delivery of oral healthcare and access to services? Evidence from a pilot contact in Northern Ireland
BMC Health Services Research (2017)