Abstract
Study design:
Survey.
Objectives:
To describe and compare perceived barriers with patient flow in spinal rehabilitation units (SRUs).
Setting:
International. Ten SRUs (Australia, Canada, India, Ireland, Italy, Netherlands, Pakistan, Switzerland, UK and USA) that admit both traumatic and non-traumatic spinal cord injury patients.
Methods:
Survey completed between December 2010 and February 2013 on perception of barriers for admission into and discharge from SRUs. Opinion was sought from the participants regarding the utility of collecting data on the timeliness of access to SRUs and occurrence of discharge barriers for benchmarking and quality improvement purposes.
Results:
The perceived barriers in accessing SRUs ranged from no access problem to a severe access problem (no access problems n=3; minor access problems n=3; moderate access problems n=2; severe access problem n=1 and extreme n=1). Most units (n=9/10) agreed that collecting data on timeliness of access to SRUs for acute hospital patients may help improve patient outcomes and health system processes by providing information for benchmarking and quality improvement purposes. All units reported perceived barriers to discharge from SRUs. Compared with admission barriers, a greater perception of barriers to discharge was reported (minor problem n=3; moderate problem n=3; severe problem n=3; and extreme n=1). All units agreed that collecting data on barriers to discharge from SRU may help improve patient outcomes and system processes.
Conclusions:
Perceived barriers to patient flow in SRUs are reported in many countries. Projects to identify and minimise the occurrence and impact of admission and discharge barriers could increase access to rehabilitation and improve the rehabilitation outcomes for patients.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) medicine is a complex field, and delayed access to appropriate expertise at any point in the care continuum—pre-hospital, emergency, acute hospital, rehabilitation and community—can potentially compromise patient outcomes. Furthermore, an inability to transfer a patient from one phase of care in the management continuum to the next phase can result in inefficient resource utilisation. This problem can contribute to difficulty with other patients at different phases in the management continuum being unable to access their optimal setting of care.
Problems with patient flow in hospital systems have been well described in emergency departments1, 2, 3 and acute-care hospitals.4, 5, 6 Patient flow in rehabilitation has not been studied to the same degree, but in recent years, a number of reports have detailed problems in this area.7, 8, 9, 10, 11 A recent survey of rehabilitation physicians in Australia highlighted problems with access to, and especially discharge from, rehabilitation units.11 A few articles have previously highlighted problems for patients with non-traumatic SCI (NTSCI) not being able to access specialist spinal cord rehabilitation services as readily as patients with traumatic SCI (TSCI).7, 12, 13, 14 The occurrence of barriers for admission into spinal rehabilitation units (SRUs) for patients with recent onset of spinal cord damage or barriers to discharge from SRUs after the completion of necessary inpatient rehabilitation for patients with spinal cord damage from any cause are an issue that has received little attention in the literature.
We planned a survey of units participating in our research collaboration, the International Spinal Cord Rehabilitation (ISCoR) study group (previously known as the International Non-traumatic Spinal Cord Injury Study Group)15 on the perception of senior staff, regarding barriers for admission of patients into their SRU from acute hospitals and subsequent barriers to discharge. It is important to emphasis that all participating units admit patients with spinal cord damage from any cause, both NTSCI (median, interquartile range proportion 40%, 30–42%) and TSCI (median, interquartile range proportion 45%, 20–48),15 and that the survey responses were based on consideration of both these patient groups in combination. The objective was to (a) measure the perception of barriers for admission into SRU and subsequent barriers to discharge; (b) to identify the types of perceived barriers; and (c) to provide further understanding of the context of the SRUs in the ISCoR Study Group that will be important for interpreting the results from subsequent phases of this project when patient outcomes, including length of stay in rehabilitation, are reported.
Materials and methods
Participants
The participating units were chosen by the Principal Investigator on the basis that they included a broad international representation of SRUs, including a mix of developed and developing countries. It was initially planned to include at least one unit from each continent. Despite our best efforts, no unit from South America or Africa was located that was able to participate and meet the inclusion criteria (which included admitting a minimum of 50 patients with NTSCI over 3 years for inclusion into the ISCoR study group).
The full inclusion and exclusion criteria, and the results dealing with the organisation of rehabilitation services and systems of care (funding sources, relationship with acute hospitals, catchment, referral process, the number of rehabilitation beds, proportion of patients with NTSCI and TSCI, determination of readiness to discharge, staffing ratios, provision of secondary non-core therapists and ancillary services, and relevant support programs) have been recently reported.15 Subsequent to the acceptance of the above manuscript, a site from the United Kingdom joined our Study Group, which also met the inclusion criteria.
Survey
A survey of participating units was developed by the Principal Investigator (PWN) based on clinical expertise and literature review. The survey questions on barriers to access and discharge were modified from a similar survey conducted on rehabilitation and aged-care physicians and senior hospital managers in Australia.11 The present paper is based on items concerning respondents’ perceptions regarding admission and discharge barriers for SRU patients, irrespective of aetiology of spinal cord damage (that is, the survey questions did not distinguish between TSCI and NTSCI). The survey used Likert scale (no problem, mild, moderate, severe or extreme problems) and closed questions, as well as a few open questions, allowing free-text answers (copy of the survey available from PWN). The respondents were able to select as many relevant reasons for barriers to admission and discharge from a list, with the opportunity to also add their own reasons.
The survey was completed electronically by a representative from each of the participating SRUs between December 2010 and February 2013. Given the time period over which the survey was completed, all authors reconfirmed the responses pertaining to their SRU were still applicable in March and April 2013. No specific data analysis was planned. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. Approval for the project was obtained separately by the participating units from their respective institute’s ethics committees, where required, and from the Alfred Health Human Research and Ethics Committee, Melbourne, Victoria, Australia.
Results
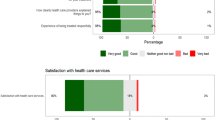
Ten SRUs agreed to participate in this project and completed the survey (Australia, Canada, Italy, Ireland, India, Netherlands, Pakistan, Switzerland, United Kingdom and USA). The responses regarding perceived barriers to admission are shown in Table 1. There was a wide diversity in the perception of barriers to admission (no access problems n=3; minor access problems n=3; moderate access problems n=2; severe access problem n=1; and extreme n=1). Despite the range of responses, most units (n=9/10) agreed that collecting data on timeliness of access to the SRU for acute hospital patients with SCI may help improve patient outcomes and health system processes by providing information for benchmarking and quality improvement purposes. Five units collected this type of information at the time of survey completion (time from ready for transfer from acute hospital until admission into SRU). The most common nominated reasons for barriers to admission were physical/environmental issues (n=7) and the number of available beds (n=5).
The responses regarding perceived barriers to discharge from the SRU are shown in Table 2. Compared with admission barriers, there was a greater perception of barriers to discharge reported (minor problem n=3; moderate problem n=3; severe problem n=3; extreme n=1). All units agreed that collecting data on barriers to discharge for SRU patients may help improve patient outcomes and health system processes. Four units collected this type of information at the time of survey completion. The most common reasons nominated for barriers to discharge from SRUs were as follows: lack of funding for caregivers (n=8), lack of funding for home modifications (n=7), waiting for nursing home (n=7) or other accommodation (n=7) and lack of funding for necessary equipment (n=6).
Discussion
Our results found that the perception of the degree of difficulty with barriers for transfer from acute hospital into SRUs varied between participating units. In contrast, there was a much more consistent perception of problems with barriers to discharge from SRUs. There was strong agreement that collecting data on both the timeliness of access to SRU and the barriers to discharge from SRU and using this information for benchmarking and quality improvement purposes may help improve patient outcomes and health system processes. Our findings highlight that problems with patient flow in SRUs are of international significance.
Our results are consistent with the survey results from Australian clinicians and health managers regarding perception of barriers to patient flow and the use of related process measures.11 In that study, 87% of rehabilitation physicians believed that there were moderate, severe or extreme discharge barriers for inpatients in their unit compared with 41% who reported the same degree of problems with barriers to admission. Although 45% of respondents in that survey reported collecting data related to the timeliness of acute hospital patients, accessing rehabilitation beds for quality improvement purposes, 70% agreed that this information would be useful for benchmarking and quality improvement purposes. Nineteen percent of respondents reported collecting data related to discharge barriers, but 71% agreed that this information would be useful. The reasons nominated as admission or discharge barriers from the Australian survey had many similarities with the reasons nominated by respondents in this report.
Our findings reinforce the assertions of others that there are problems with rehabilitation patient flow generally,9, 10 as well as patients with spinal cord damage.7, 8 Two previous reports have highlighted the problems with timely access to appropriate expertise in the SCI management continuum, particularly admission to SRU.7, 8 None of the units in our survey reported health policies limitations or constraints to either admission or discharge, as others have reported,16, 17, 18 but this may be due to the number of units included and non-random participation in the survey. A survey from The Netherlands highlighted problems with the amount of time some patients spent arranging their home modifications or alternative accommodation, with a third of patients reporting that their discharge was delayed by a median of 15 weeks while this issue was resolved.19 A recent study from the United States of America that classified the barriers to community integration for patients with SCI report that the two most common barriers were equipment issues and lack of environmental and home assistance, which coincides with the common reporting among our units of these as barriers to discharge.20
Problems with patient flow in rehabilitation can result in a number of potential adverse consequences, as well as wasting health-care resources that could be better utilised. When patients are in hospital for longer than necessary, for each additional day of hospitalisation, the risk of iatrogenic complications, such as medication errors, nosocomial infections and falls, increases by 6%.21 Stroke22 and trauma patients23 are reported to have better outcomes when transferred to rehabilitation sooner, with a shorter rehabilitation length of stay and better functional outcomes at discharge.22, 23 Similar findings have also been reported in patients with spinal cord damage. Patients with a shorter acute hospital admission have been reported to have a shorter rehabilitation admission,24, 25 fewer pressure ulcers24 and a more efficient functional improvement.25, 26
A detailed discussion of the implications of each barrier reported would be quite lengthy; however, it is apparent that in order to adequately address the range of barriers reported, more resources may be required to meet the needs of NTSCI and TSCI patients. Some of these resources may be needed by the SRUs and others by community organisations, with the specific requirements varying between settings. These resources include physical and material goods, workforce, health and disability services, and the timely availability of accommodation options for disabled. The responsibility for implementing the required solutions would vary between SRUs, but would typically lie at either a regional, State or National level. Unfortunately, given the current global economic outlook, many countries would have difficulty in adequately addressing the need highlighted here in the short term.
The implications of our results are that health funders, managers, policymakers and senior clinicians need to address patient flow inefficiencies through the whole hospital system, and not just focus on the emergency department. Our results highlight the potential to improve the flow for patients with spinal cord damage through the hospital system. Further study of this problem will facilitate the wise use of scarce resources and the best achievable patient outcomes. The problems we highlight are an important opportunity for improvement of health-care and hospital systems. A detailed understanding of access and discharge barriers would allow resources to be optimally directed. An international study group will allow cross-cultural comparisons. Efficient patient transfer to the optimal level of care may be able to reduce the total cost of care and also the chance of iatrogenic complications, and help improve functional outcomes. It is quite likely that developing solutions to access and discharge barriers would result in a significant improvement in length of stay, in both acute and rehabilitation hospitals. It is important to note that addressing the barriers to discharge for patients who have completed rehabilitation and for those whose discharges have been delayed will consequently improve access for patients waiting for transfer into the SRU.
Research is needed to measure the occurrence and causes of barriers to patient flow for SCI patients across the management continuum. A necessary requirement for future studies includes key principles to guide this research—because this field has not been well studied to-date—including the development of trans-cultural definitions, classifications and key performance indicators of patient flow in rehabilitation that can facilitate patient flow barriers being identified and addressed.27 Risk adjustment strategies will also be necessary to allow meaningful comparisons across centres. In order to improve the health-care experiences for patients, it is also suggested that future work in this field include patients' perspectives on admission and discharge barriers.
Study limitations
Limitations of our survey include the possibility of responder bias, which could have influenced answers in either direction, and the small number of participating units. We believe, however, based on discussion with colleagues in our respective countries and internationally in other SRUs, that our findings are generalisable to many other SRUs around the world, not just in the countries that participated in this survey. Furthermore, we believe that there are likely to be problems with patient flow in rehabilitation that affect other impairment groups besides those with spinal cord damage.
Other limitations are the range of factors considered in the survey questions. For example, there was no rating of the degree to which the nominated reasons for a barrier contributed to the access or discharge barriers or quantification of the rating of barrier severity. We did not record perceptions about lack of awareness of SRUs among acute hospital staff or the lack of availability of such units, and we did not attempt to measure actual duration of the barriers or their impact on length of stay. A future project plans to measure the occurrence, causes and duration of barriers to the flow of patients into and out of our units. There is also the possibility that the perceptions regarding the severity and causes of barriers to admission or discharge may have changed, either for better or worse, since the survey was conducted. Finally, we have not considered internal processes in acute hospital units or the SRU that can also impact on length of stay and contribute to admission or discharge barriers. Recent publications using the operations research methodology have highlighted the opportunities for improving these internal processes for patients with SCI.28, 29
Conclusions
We have found that many SRUs have problems with timely access for acute hospital patients to their beds and most have problems with barriers to discharge. These problems contribute to hospital inefficiency and compromise patient outcomes. Further research is warranted to quantify the extent and impact of barriers to the flow of patients with spinal cord damage through the care continuum. Systems improvement processes designed to minimise the barriers identified could result in benefits for individual patients and major improvements in the flow of patients through the entire hospital system.
Data archiving
There were no data to deposit.
References
Trzeciak S, Rivers EP . Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J 2003; 20: 402–405.
Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 2009; 16: 1–10.
Eitel DR, Rudkin SE, Malvehy MA, Killeen JP, Pines JM . Improving service quality by understanding emergency department flow: a White Paper and Position Statement prepared for the American Academy of Emergency Medicine. J Emerg Med 2010; 38: 70–79.
Weaver FM, Guihan M, Hynes DM, Byck G, Conrad KJ, Demakis JG . Prevalence of subacute patients in acute care: results of a study of VA hospitals. J Med Syst 1998; 22: 161–172.
Flintoft VF, Williams Jl, Williams RC, Basinski AS, Blackstien-Hirsch P, Naylor CD . The need for acute, subacute and nonacute care at 105 general hospital sites in Ontario. CMAJ 1998; 158: 1289–1296.
Carey MR, Sheth H, Braithwaite RS . A prospective study of reasons for prolonged hospitalizations on a general medical teaching service. J Gen Intern Med 2005; 20: 108–115.
Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S et al. An Italian survey of traumatic spinal cord injury. The gruppo Italiano studio epidemiologico mielolesioni study. Arch Phys Med Rehabil 2003; 84: 1266–1275.
Amin A, J B, Najarajah R, Davies N, Gow F, Tucker S . Spinal injuries admitted to a specialist centre over a 5-year period: a study to evaluate delayed admission. Spinal Cord 2005; 43: 434–437.
Bradley LJ, Kirker SG, Corteen E, Seeley HM, Pickard JD, Hutchinson PJ . Inappropriate acute neurosurgical bed occupancy and short falls in rehabilitation: implications for the National Service Framework. Br J Neurosurg 2006; 20: 36–39.
New PW, Poulos CJ . Functional improvement of the Australian health care system — can rehabilitation assist? Med J Aust 2008; 189: 340–343.
New PW, Cameron PA, Olver JH, Stoelwinder JU . Key stakeholders’ perception of barriers to admission and discharge from inpatient subacute care in Australia. Med J Aust 2011; 195: 538–541.
Smith M . Efficacy of specialist versus non-specialist management of spinal cord injury within the UK. Spinal Cord 2002; 40: 11–16.
New PW . Non-traumatic spinal cord injury: what is the ideal setting for rehabilitation? Aust Health Rev 2006; 30: 353–361.
New PW, Simmonds F, Stevermuer T . Comparison of patients managed in specialised spinal rehabilitation units with those managed in non-specialised rehabilitation units. Spinal Cord 2011; 49: 909–916.
New PW, Townson A, Scivoletto G, Post MWM, Eriks-Hoogland I, Gupta A et al. International comparison of the organisation of rehabilitation services and systems of care for patients with spinal cord injury. Spinal Cord 2013; 51: 33–39.
Anzai K, Young J, McCallum J, Miller B, Jongbloed L . Factors influencing discharge location following high lesion spinal cord injury rehabilitation in British Columbia, Canada. Spinal Cord 2006; 44: 11–18.
Dobrez D, Heinemann AW, Deutsch A, Manheim L, Mallinson T . Impact of Medicare’s prospective payment system for inpatient rehabilitation facilities on stroke patient outcomes. Am J Phys Med Rehabil 2010; 89: 198–204.
Pezzin LE, Roberts BA, Miao H, Dillingham TR . Regulatory policies, the ‘‘75% rule,’’ and post-acute care discharge setting. Am J Phys Med Rehabil 2011; 90: 954–958.
Post MWM, van Asbeck FWA, van Dijk AJ, Schrijvers AJP . Services for spinal cord injured: availability and satisfaction. Spinal Cord 1997; 35: 109–115.
Silver J, Ljungberg I, Libin A, Groah S . Barriers for individuals with spinal cord injury returning to the community: a preliminary classification. Disabil Health J 2012; 5: 190–196.
Andrews LB, Stocking C, Krizek L, Gottlieb L, Krizek C, Vargish T et al. An alternative strategy for studying adverse events in medical care. Lancet 1997; 349: 309–313.
Maulden SA, Gassaway J, Horn SD, Smout RJ, DeJong G . Timing of initiation of rehabilitation after stroke. Arch Phys Med Rehabil 2005; 86 (Suppl 2): S34–S40.
Sirois M, Lavoie A, Dionne C . Impact of transfer delays to rehabilitation in patients with severe trauma. Arch Phys Med Rehabil 2004; 85: 184–191.
Aung TS, El Masry WS . Audit of a British centre for spinal injury. Spinal Cord 1997; 35: 147–150.
Sumida M, Fujimoto M, Tokuhiro A, Tominaga T, Magara A, Uchida R . Early rehabilitation effects for traumatic spinal cord injury. Arch Phys Med Rehabil 2001; 82: 391–395.
Scivoletto G, Morganti B, Molinari M . Early versus delayed inpatient spinal cord injury rehabilitation: An Italian study. Arch Phys Med Rehabil 2005; 86: 512–516.
New PW, Cameron PA, Olver JH, Stoelwinder JU . Defining barriers to discharge from inpatient rehabilitation, classifying their causes, and proposed performance indicators for rehabilitation patient flow. Arch Phys Med Rehabil 2013; 94: 201–208.
Atkins D, Noonan VK, Santos A, Lewis R, Fehlings M, Burns A et al. Secondary complications in SCI across the continuum: using operations research to predict the impact and optimize management strategies. Top Spinal Cord Inj Rehabil 2012; 1: 57–66.
Noonan VK, Soril L, Atkins D, Lewis R, Santos A, Fehlings MG et al. The application of operations research methodoligies to the delivery of care model for traumatic spinal cord injury: the access to care and timing (ACT) project. J Neurotrauma 2012; 29: 2272–2282.
Acknowledgements
For assisting in refining the pilot version of the survey, we thank Michele New; Associate Professor Christopher J Poulos, Hammond Chair of Positive Ageing and Care, University of New South Wales, Australia; Dr Richard Bignell; Associate Professor Fary Kahn, Principal Fellow, Department of Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia; and Dr Hean See Tan, Rehabilitation and Aged Services, Medicine Program, Kingston Centre, Southern Health, Victoria, Australia. The following people are thanked for their assistance with facilitating the data collection: Bianca Fedele (Caulfield Hospital, Australia), Michael Baumberger (Swiss Paraplegic Center, Switzerland), Joost van Middendorp and Salman Lari (National Spinal Injuries Centre, Stoke Mandeville Hospital).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
New, P., Scivoletto, G., Smith, É. et al. International survey of perceived barriers to admission and discharge from spinal cord injury rehabilitation units. Spinal Cord 51, 893–897 (2013). https://doi.org/10.1038/sc.2013.69
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.69
Keywords
This article is cited by
-
Unmet healthcare needs and health inequalities in people with spinal cord injury: a direct regression inequality decomposition
International Journal for Equity in Health (2023)
-
Challenges and potential improvements in the admission process of patients with spinal cord injury in a specialized rehabilitation clinic – an interview based qualitative study of an interdisciplinary team
BMC Health Services Research (2017)
-
Understanding the Role of Rehabilitation Medicine in the Care of Patients with Tumor Causing Spinal Cord Dysfunction
Current Physical Medicine and Rehabilitation Reports (2017)
-
Time-series analysis of the barriers for admission into a spinal rehabilitation unit
Spinal Cord (2016)
-
Developing human rights based indicators to support country monitoring of rehabilitation services and programmes for people with disabilities: a study protocol
BMC International Health and Human Rights (2015)