Abstract
Study design:
Pressure ulceration and other complications constitute an encumbrance in the management of spinal cord injury in many services with limited resources in developing countries. These services undertake patients’ care without adequate prehospital care, limited modern infrastructure and limited number of trained staff.
Objectives:
To evaluate the associated risk factors for pressure ulceration in traumatic spinal cord injured managed in a resource constrained spinal injury unit in Lagos, Nigeria. A regional acute trauma and rehabilitation centre serving a population of >20 million.
Methods:
This is a prospective study in patients presenting with traumatic spinal cord injury between 1 October 2004 and 30 November 2006. The data collected include demographic characteristics, interval before admission in the unit, type of spinal cord injury and serum albumin. The incidence of pressure ulcers and the isolated organisms was recorded for patients who developed pressure ulcers on admission and during the period of stay in the unit. The length of hospital stay was also recorded for all the patients.
Results:
The overall incidence of pressure ulceration on admission was 57.1%. There was an average lengthening of hospital stay of 33.1 days in the group of patients with pressure ulceration compared to patients without pressure ulcers. The nutritional status on admission, interval before admission and the type of neurological injury were significant factors for the incidence of pressure ulcers.
Conclusion:
The incidence of pressure ulceration was high, delay in admission and poor nutritional status may be significant factors in the incidence of pressure ulceration in spinal cord injury.
Similar content being viewed by others
Introduction
Pressure ulcers though an ancient medical problem (found in autopsies on Egyptian mummies) still afflicts patients even up to the present day. Bedridden patients, who are neurologically impaired as in spinal cord injury, are highly predisposed. In the acute care setting with predominantly bedridden, supine patients, the common sites for pressure sores are sacral, heel, trochanteric, ischial and malleolar regions.1, 2, 3
The incidence of pressure ulceration in acute spinal injury varies from 12.4% to >50% and the reports have suggested that 94.7% of such ulcers occurred before the third week of admission. Previous reports have identified delayed presentation, low serum proteins, premorbid medical condition such as diabetes, and completeness of the spinal cord injury as risk factors for pressure ulceration.3, 4, 5, 6, 7, 8, 9, 10, 11
The organisation of healthcare in Nigeria is the responsibility of three tiers of the government. The federal government has the overall responsibility for the university teaching hospitals teachings in hospitals and the three National Orthopaedic Hospitals, which are involved in the management of major trauma such as spinal injury. However, the absence of a well-developed national health insurance scheme makes the funding of health services the responsibility of patients and their relatives at the time of delivery. Private healthcare institutions with varying level of infrastructure also have a significant role in management of trauma patients.
The National Orthopaedic Hospital, Lagos is a 450-bed Trauma and Orthopaedic centre, with 20 dedicated rehabilitation beds for spinal cord injured. Thus, spinal cord injured patients present to this centre in different phases of the injury that is acute phase (<24 h) and delayed phase. The patients presenting after 24 h of injury have usually had prior treatment at private hospitals, government funded general hospitals or non-orthodox medical facilities.
There is no clear guideline on the transfer and prehospital care of patients with spinal cord injury as yet. The prehospital care of trauma patients in Lagos state with a population of >15 million is shared between the Lagos state emergency medical services with 15 ambulance points and ‘good Samaritans’ (consisting of relatives and motorists at the scene of accidents without formal training). These ambulance points are emergency medical centres located in various parts of the Lagos metropolis, equipped for basic life support. The emergency services provided include triage, initial resuscitation and transfer to specialized trauma centres.
While most centres in the resource constrained countries undertake the care of patients with acute spinal cord injury in an informal prehospital care system, paucity of information about the complications of spinal cord injury, especially in the West African sub-region constitutes an encumbrance in the development of an effective spinal injury service in the sub-Saharan Africa.12, 13, 14
Objectives
To evaluate the associated risk factors for pressure ulceration in traumatic spinal cord injured managed in a resource constrained spinal injury unit in Lagos.
To determine the difference in the length of stay attributable to pressure ulceration.
Setting
The Spinal Unit of the National Orthopaedic Hospital Igbobi, Lagos, a regional acute spinal and rehabilitation centre serving a population of >20 million people.
Inclusion criteria
The consecutive cases of new patients admitted with traumatic spinal cord injury from 1 October 2004 to 30 November 2006.
Exclusion criteria
-
1)
All patients with pressure ulcers from casts and plasters.
-
2)
Seventeen patients who sought discharge against medical advice before completion of rehabilitation were excluded. The time of discharge in this patients’ group vary, and assessment of the severity of pressure ulcer and serial changes in nutritional status was impossible.
-
3)
Six patients were known diabetics and were excluded on account of their premorbid medical condition and presence of foot ulcers.
Patients and methods
Informed consent
An informed consent was obtained from the patients before inclusion in the study.
Method
All the patients were reviewed on admission by the first author and patients’ demographics, aetiology of injury, time of injury, past medical history were recorded. The presence of pressure ulcers at the time of presentation was determined by examination of the pressure areas. The patients were evaluated using the American Spinal Injury Association Score (ASIA) impairment scale and the anatomical level of spinal cord injury and the type of the neurological lesion (complete or incomplete) were determined.
The patients were classified based on the time of injury to the time of presentation into two groups, <24 h (early) and >24 h (delayed). The serum albumin was measured on admission in all the patients and repeated at a weekly interval for all the patients. The serum albumin was measured using the Randox reagent, based on albumin binding to bromocresol green concentrate (Randox Laboratories Ltd., Crumlin, Co. Antrim, UK). The patients with serum albumin of <3.5 g per 100 ml were categorized as poorly nourished and patients with values above these were categorized as well nourished.
All the pressure areas were assessed for ulcers and graded at a regular interval until the patients were discharged using the National Pressure Ulcer Advisory staging system15 (Table 1). Wound swabs for microscopy, culture and sensitivity were obtained, where pressure sores have developed. The total length and cost of hospital stay were computed on discharge.
The data collated using the Microsoft excel package and analyzed with statistical package for social sciences (SPSS) version 14 (Copyright IBM Corporation 2010 IBM Corporation, Somers, NY, USA). The test of significant association was done using χ2 and Students’ t-test for qualitative and quantitative variables, respectively.
Results
Age distribution
All the 105 patients in this study were between 13 and 57 years of age, with a mean of 35.5±11.2 years. The majority were between 20 and 49 years of age (Figure 1). The mean age for patients who developed pressure sores was 33.7±11.3 years, while the mean age for the patients who were without pressure sores during hospitalisation 37.9±11.1 years. There was no significant association between age of the patient and incidence of pressure sores in this study (P=0.084).
Anatomic distribution of pressure sores
A total of 122 pressure ulcers were recorded in these patients. The sacral region was the most common pressure ulcer site in the study and this occurred in 56 cases (45.9%). The other pressure ulcer sites include trochanteric region in 44 cases (36.1%), the heel in 18 cases (14.8%), the elbow in 2 cases (1.6%), the shoulder blade and the occipital regions in 1 case each (0.8%) (Figure 2).
Isolated organisms
Staphylococcus spp. was the single most common organism isolated from the microbiological examination of these ulcers. A large number of ulcers had mixed growth of coliform organisms and Staphylococcus spp. (Figure 3).
Length of hospital stay
The length of hospital stay for all the patients ranged between 24 and 220 days, with a mean of 79.2±38.9 days. Patients with pressure sores had the mean length of hospital stay of 93.4±44.7 days. The patients without pressure ulcers had the mean length of stay of 60.3±17.7 days, with an average length of hospital stay by 33.1 days. The difference in the length of hospital stay between the two groups was statistically significant (P=0.022).
Interval before admission
There was pressure ulceration in 13.9% of patients at the time of admission (Table 2) this is because 57 (54%) of the patients presented ⩾24 h after spinal cord injury. The incidence of pressure ulceration in patients presenting within 24 h of injury was 35% compared to 74% among those presenting after 24 h. There was a significant association between the interval before presentation and incidence of pressure sores P=0.027.
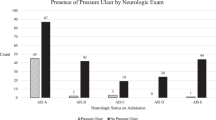
Type of neurological lesion
Sixty-three patients had complete neurological lesion (ASIA A) and 46 patients (73%) in this group developed a single or multiple pressure ulcers. Forty-two patients had incomplete lesion and 14 patients (33%) in this group developed pressure ulcers (ASIA B, C, D). There was significant association between the type of neurological injury and incidence of pressure sore (P=0.016).
Serum albumin levels
In the first week of admission, 38 patients (36.2%) presented with low serum albumin and were categorized as poorly nourished. The number in the poorly nourished spinal cord injured group increased to 58 (55.2%) by the third week of admission, all the patients spent a minimum of 3 weeks on admission which was the minimum number of weeks all the patients spent in hospital (Table 3).
At the time of admission, 38 patients were in the ‘poorly nourished’ group, among whom 33 patients (86.8%) developed pressure sores. Sixty-seven patients were in the ‘well nourished’ group on admission, among whom 27 (40.3%) developed pressure sores. There was significant association between the nutritional status at the time of admission and the incidence of pressure sores (P=0.037).
Discussion
In the population studied, most patients with traumatic spinal cord injury belong to the active age group (mean age was 35.5±11.2 years). However, there was no significant association between the age of the patient and the incidence of pressure sores. Perhaps the younger age of the patients with traumatic spinal cord injury renders aging as one of the less important risk factors for pressure ulceration.
The overall incidence of pressure sores in this study was 45.9%, this is a high figure when compared to many other reports.3, 16 Resource constraints in the number of trained staff and in the number of modern pressure relieving devices prompted dependence on relatives and other untrained personnel in patients’ nursing care. These are the likely contributory factors to a higher incidence of pressure ulceration.
The family members participating in the care of the acutely spinal cord injured should be provided with better education on skin care to reduce the incidence of pressure ulceration. Previous reports suggest better outcome where responsible relatives were involved in the early in-hospital care, and were provided with basic education about the care of the spinal cord injured.17
Delayed presentation is still a problem in the management of the spinal cord injured patients in the developing countries such as Nigeria. The quality of care received at the initial facility may be non-orthodox or sub-optimal probably contributory to the higher incidence of pressure ulceration in this group of patients.
The patients with complete neurological injury had increased incidence of pressure ulceration. These patients usually have anaesthesia in the involved body parts, limiting their awareness of skin changes due to pressure. Complete injury is also associated with maceration from incontinence, which increases the risk of pressure sores. However, patients with incomplete injury can usually be educated and motivated to use the upper limb for support in turning the body regularly. Such manoeuvre has been reported to reduce the risk of pressure sores.5, 18
The improvement in prehospital care for spinal cord injured, and the provision of a national guideline for the treatment of the spinal cord injured may reduce incidence of pressure ulcer. Emphasis should be placed on early referral to specialised centres, better hospital patient flow, and training of specialist wound care nurses and provision of free nutritional supplements.
The association between the incidence of pressure sore and low serum proteins indicate that dysmetabolism may be contributory to the aetiology of pressure ulceration. However, some evidence suggests that this may be an effect rather than the cause of the ulcer. There is no doubt that ulcer healing and immunity against wound infections is greatly dependent on the nutritional status of the individual patient.
Furthermore, serum albumin has been reported as a cost-effective measure of nutritional status and risk of adverse surgical outcome. That this relatively simple and affordable test is underutilized has also been highlighted by previous studies among in-hospital patients.3, 6, 10, 11, 19 The utilization of prognostic indicators such as serum albumin in early detection of spinal cord injured with adverse outcome may reduce the incidence of complications.
There is a need for more prospective studies on the predictive factors for complications and adverse outcome in trauma patients especially, spinal cord injured in sub-Saharan Africa.
References
Kottner J, Balzer K, Dassen T, Heinze S . Pressure ulcers: a critical review of definitions and classifications. Ostomy Wound Manage 2009; 55: 22–29.
Black J, Baharestani M, Cuddigan J, Dorner B, Edsberg L, Langemo D et al. National Pressure Ulcer Advisory Panel (2007) National Pressure Ulcer Advisory Panel's updated pressure ulcer staging system. Dermatol Nurs 2007; 19: 343–349.
Fife C, Otto G, Capsuto EG, Brandt K, Lyssy K, Murphy K et al. Incidence of pressure ulcers in a neurologic intensive care unit. Crit Care Med 2001; 29: 283–290.
Pagliacci MC, Celani MG, Spizzichino L, Zampolini M, Aito S, Citterio A et al. Spinal cord lesion management in Italy: a 2-year survey. Spinal Cord 2003; 41: 620–628.
Richardson RR, Meyer Jr PR . Prevalence and incidence of pressure sores in acute spinal cord injuries. Paraplegia 1981; 19: 235–247.
Gurcay E, Bal A, Gurcay AG, Cakci A . Evaluation of blood and serum markers in spinal cord injured patients with pressure sores. Saudi Med J 2009; 30: 413–417.
Amin A, Bernard J, Nadarajah R, Davies N, Gow F, Tucker S . Spinal injuries admitted to a specialist centre over a 5-year period: a study to evaluate delayed admission. Spinal Cord 2005; 43: 434–437.
Aito S . Complications during the acute phase of traumatic spinal cord lesions. Spinal Cord 2003; 41: 629–635.
Rodriguez GP, Garber SL . Prospective study of pressure ulcer risk in spinal cord injury patients. Paraplegia 1994; 32: 150–158.
Fuoco U, Scivoletto G, Pace A, Vona VU, Castellano V . Anaemia and serum protein alteration in patients with pressure ulcers. Spinal Cord 1997; 35: 58–60.
Scivoletto G, Fuoco U, Morganti B, Cosentino E, Molinari M . Pressure sores and blood and serum dysmetabolism in spinal cord injury patients. Spinal Cord 2004; 42: 473–476.
Mock CN, Tiska M, Adu-Ampofo M, Boakye G . Improvements in prehospital trauma care in an African country with no formal emergency medical services. J Trauma 2002; 53: 90–97.
Oluwadiya KS, Olakulehin AO, Olatoke SA, Kolawole IK, Solagberu BA, Olasinde AA et al. Pre-hospital care of the injured in South Western Nigeria: a hospital based study of four tertiary level hospitals in three states. Annu Proc Assoc Adv Automot Med 2005; 49: 93–100.
Gosselin RA, Coppotelli C . A follow-up study of patients with spinal cord injury in Sierra Leone. Int Orthop 2005; 29: 330–332.
Witowski JA . Pressure ulcers prevalence, cost and risk assessment: consensus development conference statement—The National Pressure Ulcer Advisory Panel. Decubitus 1989; 2: 24–28.
Hammond MC, Bozzacco VA, Stiens SA, Buhrer R, Lyman P . Pressure ulcer incidence on a spinal cord injury unit. Adv Wound Care 1994; 7: 57–60.
Nwankwo OE, Katchy AU . Outcome of a 12-week programme for management of the spinal cord injured with participation of patient's relations at Hilltop Orthopaedic Hospital, Enugu, Nigeria. Spinal Cord 2003; 41: 129–133.
Correa GI, Fuentes M, Gonzalez X, Cumsille F, Piñeros JL, Finkelstein J . Predictive factors for pressure ulcers in the ambulatory stage of spinal cord injury patients. Spinal Cord 2006; 44: 734–739.
Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF et al. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg 1999; 134: 36–42.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Idowu, O., Yinusa, W., Gbadegesin, S. et al. Risk factors for pressure ulceration in a resource constrained spinal injury service. Spinal Cord 49, 643–647 (2011). https://doi.org/10.1038/sc.2010.175
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.175
Keywords
This article is cited by
-
The global burden of pressure ulcers among patients with spinal cord injury: a systematic review and meta-analysis
BMC Musculoskeletal Disorders (2020)
-
Pressure ulcers after traumatic spinal injury in East Africa: risk factors, illustrative case, and low-cost protocol for prevention and treatment
Spinal Cord Series and Cases (2020)
-
Predictors of pressure ulcer incidence following traumatic spinal cord injury: a secondary analysis of a prospective longitudinal study
Spinal Cord (2018)
-
Outcomes after acute traumatic spinal cord injury in Botswana: from admission to discharge
Spinal Cord (2017)
-
Pressure ulcers in people with spinal cord injury in developing nations
Spinal Cord (2015)