Abstract
To identify whether urolithiasis with or without hydronephrosis has an impact on acute kidney injury (AKI) in patients with urinary tract infection (UTI). This study aimed to identify whether urolithiasis with or without hydronephrosis has an impact on AKI in patients with UTI. This retrospective study enrolled hospitalized UTI patients who underwent imaging in an acute care setting from January 2006 to April 2019. Of the 1113 participants enrolled, 191 (17.2%) had urolithiasis and 76 (6.8%) had ureteral stone complicated with hydronephrosis. Multivariate logistic regression analysis showed that in UTI patients with urolithiasis, the presence of ureteral stone with concomitant hydronephrosis was an independent risk factor for AKI (odds ratio [OR] 2.299, 95% confidence interval [CI] 1.112–4.755, P = 0.025). In addition, urolithiasis was associated with an increased risk for AKI (OR 2.451, 95% CI 1.369–4.389, P = 0.003) in UTI patients without hydronephrosis. The presence of ureteral stone with hydronephrosis increases the risk for AKI of UTI patients with urolithiasis, and urolithiasis remains a risk factor of AKI in UTI patients without hydronephrosis.
Similar content being viewed by others
Introduction
Urolithiasis is a widespread problem with a male preponderance, showing a lifetime prevalence of 10% in men and 5% in women1,2. The worldwide prevalence of urolithiasis is also steadily increasing1,2,3, partially owing to its strong association with metabolic syndrome conditions such as obesity, hypertension, and diabetes4.
Urolithiasis can cause secondary complications, such as obstruction or urinary tract infection (UTI)5. Acute UTI may cause sudden deterioration of renal function, especially in the presence of urinary tract obstruction6. Our previous study showed that urolithiasis is a risk factor for acute kidney injury (AKI) among patients with UTI7, and AKI has been associated with short- and long-term mortality8. Since AKI leads to poor outcomes, recognizing the risk factors for its development in patients with urolithiasis and UTI is crucial. However, no study has focused on whether urolithiasis without hydronephrosis is a risk factor for the development of AKI in patients with UTI, or whether hydronephrosis caused by ureteral stone is a risk factor for the development of AKI in UTI patients with urolithiasis. Hence, we conducted this study to investigate these important issues.
Results
Characteristics of the study population
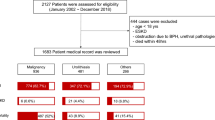
The demographic and clinical characteristics of the 1113 hospitalized UTI patients included in this study are shown in Table 1. The included patients were divided into three groups: UTI patients with no hydronephrosis or urolithiasis, UTI patients with ureteral stone and concomitant hydronephrosis, or UTI patients with urolithiasis but no hydronephrosis (Fig. 1). The mean age on admission was 66 ± 17 years. Most of the patients (816 [73.3%]) were women, and 375 (33.7%) had a history of prior UTI. Of the patients, 220 (19.8%) had uroseptic shock and 165 (14.8%) had AKI during hospitalization. The overall mortality rate was 0.6% (7/1113). Among UTI patients, 191 (17.2%) had urolithiasis and 76 (6.8%) had ureteral stone with hydronephrosis. Among 76 UTI patients with ureteral stone and hydronephrosis, five (6.6%) had bilateral ureteral stones complicated with bilateral hydronephrosis. Figure 2 shows a reduction in estimated glomerular filtration rate (eGFR) in different groups of hospitalized patients with UTI. The reduction in eGFR in UTI patients without urolithiasis or hydronephrosis, in those with urolithiasis but without hydronephrosis, and in those with ureteral stone and concomitant hydronephrosis was 13.45 (95% confidence interval [CI] 12.44–14.45), 20.54 (95% CI 16.34–24.73), and 27.65 (95% CI 21.77–33.53) mL/min/1.73 m2, respectively. Thirteen urolithiasis patients who had hydronephrosis but with no ureteral stone identified in imaging studies and 69 patients who did not have urolithiasis but had hydronephrosis were excluded from further analysis (Fig. 1). The use of antibiotics was not included in subsequent univariate and multivariate logistic regression analyses because there is no statistical significance in multivariate analysis or after excluding those developing AKI before antibiotic administration.
Risk factors of hospitalized UTI patients with urolithiasis with respect to ureteral stone and concomitant hydronephrosis
The demographic and clinical characteristics of UTI patients with urolithiasis are shown in Table 2. Patients with ureteral stone and concomitant hydronephrosis had higher serum creatinine level on admission (2.35 ± 2.28 versus 1.58 ± 1.41 mg/mL, P = 0.02), longer hospital stay (12 ± 6 versus 9 ± 4 days, P < 0.001), higher prevalence of bacteremia (69.7% versus 49.0%, P = 0.006), AKI (40.8% versus 22.5%, P = 0.009) and the use of carbapenems (18.4% versus 2.9%, P = 0. 001), and lower prevalence of afebrile status (19.7% versus 40.2%, P = 0.004) and the use of cephalosporines (56.6% versus 72.5%, P = 0. 026) than those without ureteral stone and concomitant hydronephrosis. Univariate logistic regression analysis showed that older age (odds ratio [OR] 1.032, 95% CI 1.006–1.057, P = 0.014), uroseptic shock (OR 6.249, 95% CI 3.074–12.702, P < 0.001), and ureteral stone with concomitant hydronephrosis (OR 2.366, 95% CI 1.233–4.541, P = 0.01) were associated with an increased risk for AKI, whereas a higher platelet count (OR 0.995, 95% CI 0.991–1.000, P = 0.042) was associated with a decreased risk for AKI in UTI patients with urolithiasis. Multivariate logistic regression analysis revealed that older age (OR 1.030, 95% CI 1.000–1.060, P = 0.047), uroseptic shock (OR 5.605, 95% CI 2.683–11.709, P < 0.001), and ureteral stone with concomitant hydronephrosis (OR 2.299, 95% CI 1.112–4.755, P = 0.025) were independently associated with an increased risk for AKI in UTI patients with urolithiasis (Table 3).
Risk factors of hospitalized UTI patients without hydronephrosis with respect to urolithiasis
The demographic and clinical characteristics of UTI patients without hydronephrosis are shown in Table 4. Patients with urolithiasis had a higher prevalence of male gender (38.2% versus 25.3%, P = 0.005), prior history of UTI (45.1% versus 31.4%, P = 0.016), AKI (22.5% versus 9.6%, P < 0.001), and Proteus species (7.8% versus 1.6%, P = 0.001), but a lower prevalence of Escherichia coli (E. coli) (72.5% versus 80.9%, P = 0.047), than those without urolithiasis. Univariate logistic regression analysis showed that older age (OR 1.029, 95% CI 1.015–1.043, P < 0.001), diabetes mellitus (DM) (OR 1.549, 95% CI 1.031–2.326, P = 0.035), hypertension (OR 2.596, 95% CI 1.665–4.048, P < 0.001), congestive heart failure (CHF) (OR 2.691, 95% CI 1.282–5.646, P = 0.009), afebrile status (OR 1.556, 95% CI 1.034–2.340, P = 0.034), bacteremia (OR 1.696, 95% CI 1.128–2.550, P = 0.011), uroseptic shock (OR 4.318, 95% CI 2.814–6.627, P < 0.001), urolithiasis (OR 2.737, 95% CI 1.632–4.591, P < 0.001), and higher white blood cell (WBC) count (OR 1.059, 95% CI 1.027–1.092, P < 0.001) were associated with an increased risk for AKI, whereas a higher baseline eGFR (OR 0.982, 95% CI 0.976–0.989, P < 0.001) and the use of nephrotoxic agents (OR 0.447, 95% CI 0.296–0.675, P < 0.001) were associated with a decreased risk for AKI in UTI patients without hydronephrosis. Multivariate logistic regression analysis revealed that hypertension (OR 2.125, 95% CI 1.255–3.599, P = 0.005), uroseptic shock (OR 4.683, 95% CI 2.880–7.613, P < 0.001), urolithiasis (OR 2.451, 95% CI 1.369–4.389, P = 0.003), and higher WBC count (OR 1.069, 95% CI 1.034–1.105, P < 0.001) were independently associated with an increased risk for AKI in UTI patients without hydronephrosis. Conversely, a higher baseline eGFR (OR 0.987, 95% CI 0.979–0.996, P = 0.004) and the use of nephrotoxic agents (OR 0.510, 95% CI 0.319–0.816, P = 0.005) were independently associated with a decreased risk for AKI in UTI patients without hydronephrosis (Table 5).
Discussion
UTI is a common complication in patients with urolithiasis. Urolithiasis is a common cause of urinary tract obstruction predisposing to UTI9. A previous study showed that urinary obstruction is a predictor of the development of septic shock in UTI patients10. In this study, we identified that the presence of ureteral stone with hydronephrosis is a risk factor for AKI in UTI patients with urolithiasis. In addition, urolithiasis is a risk factor for AKI in UTI patients without hydronephrosis. To our knowledge, this is the first study to demonstrate that urolithiasis without hydronephrosis is associated with an increased risk for AKI in patients with UTI.
Urolithiasis is a major cause of obstructive pyelonephritis, accounting for 65% of obstructive pyelonephritis events11. Urinary stasis provides the time and opportunity for bacteria to adhere to the urothelium, multiply, and infect the host12. In addition, stones moving down the ureter result in inflamed narrowing of the ureter or injuries, which could easily cause infection13. Obstructive uropathy is not a rare cause of UTI. A previous study showed that the rate of obstructive uropathy in patients clinically diagnosed with a simple pyelonephritis was approximately 6%14. Obstructive UTI is associated with a high recurrence rate. In a long-term follow-up study in patients with obstructive pyelonephritis, the incidence of recurrent obstructive pyelonephritis and recurrent UTI was 11% and 33%, respectively11. The existence of ureteral stone is the most common cause of urosepsis in patients with urinary tract obstruction10. UTI in the presence of urinary tract obstruction is a serious clinical situation. In the case of acute obstructive uropathy, the increased intrarenal pelvic pressure decreases the drug delivery to the kidney15. Both urolithiasis and obstructive uropathy have an impact on the severity of urosepsis16, the presence of urinary tract obstruction in patients with acute pyelonephritis is associated with an increased risk for urosepsis and uroseptic shock17,18. In the current study, the presence of ureteral stone with hydronephrosis was an independent risk factor for AKI development in UTI patients with urolithiasis.
Obstructive nephropathy is the major cause of non-infectious urolithiasis associated AKI19. Renal vasoconstriction and inflammation can occur in response to increased intratubular pressure, and cause ischemia injury. If ischemia persists, glomerulosclerosis, tubular atrophy, and interstitial fibrosis occur20. In a rat model, complete unilateral obstruction for 24 h resulted in irreversible loss of function in 15% of the nephrons of the affected kidney21. Obstructive AKI caused by urolithiasis is not common, accounting for only approximately 1–2% of all AKI events19. A previous study reported that the prevalence of AKI among patients with non-infectious ureteral stone was 0.72%22. Infection is one of the leading causes of AKI in patients with ureteral stone23, and infection with concomitant obstructive uropathy causes loss of function far more rapidly than a simple obstructive uropathy24. Yamamoto et al. found that approximately 80% of patients with acute obstructive pyelonephritis induced by upper ureteral stone had elevated serum creatinine levels above the normal range25. AKI is associated with an increased risk for mortality in patients with upper ureteral stone with concomitant urosepsis26. Untreated infection with concomitant urinary tract obstruction can lead to life-threatening sepsis. After the administration of appropriate antibiotics, interventions, such as drainage for source control, should be performed within 12 h after the diagnosis of sepsis, according to the recommendation from the Surviving Sepsis Campaign 201627. The management of infected hydronephrosis secondary to urolithiasis is prompt decompression of the renal collecting system28. Optional methods of decompression include percutaneous nephrostomy and retrograde ureteral stenting16. Decompression of the renal collecting system increases the renal plasma flow and delivery of antibiotics to both the renal parenchyma and urine29. Moreover, the release of inner pressure from the upper urinary tracts reduces the invasion of bacteria into the bloodstream or renal parenchyma30. Both the increase of antibiotic penetration into the affected renal unit and the decrease of bacterial invasion can facilitate infection control. Further, the severity of tubular atrophy and interstitial fibrosis increases if the duration of obstruction is extended31, and a delayed relief of ureteral obstruction decreases long-term renal function32. If obstruction is relieved early and infection is controlled, the renal parenchyma has a great potential for recovery23. Delay or omission of renal decompression will increase the rate of sepsis and mortality11. Because UTI patients with concomitant ureteral stone resulting in urinary tract obstruction are predisposed to develop severe complications, such as septic shock or AKI, timely decompression of the renal collecting system through percutaneous nephrostomy or retrograde ureteral stenting after starting empiric antibiotic therapy is recommended for those with a critical status33.
Urolithiasis is a source of infection34, and UTIs are frequently associated with almost all chemical types of kidney stones35. Urolithiasis is the one of most common urological disorders associated with complicated pyelonephritis36 and is also a risk factor for treatment failure in patients with acute pyelonephritis37. Because the amount of bacteria on the stone surface can increase despite antibiotic therapy, eradication of the associated UTI is only possible after the stone has been completely removed38. According to the Nationwide Inpatient Sample survey between 1999 and 2009, the incidence of urolithiasis-associated sepsis and severe sepsis is increasing39. Urolithiasis is also a risk factor of septic shock in patients with UTI7, and sepsis is one of the most common etiologies of AKI40. In the current study, urolithiasis without hydronephrosis was associated with an increased risk for AKI in patients with UTI. Early imaging examination to identify urolithiasis and complete removal of urolithiasis after ameliorating the symptoms of sepsis are crucial for patients with UTI.
Our study had several limitations. First, this was a single-center study with a retrospective design. A multicenter prospective study with a larger sample size will be needed to confirm our results. Second, we did not routinely examine the stone characteristics in this study. Further studies evaluating the chemical types of stones will be needed to confirm their impact on AKI in patients with UTI. Third, nephrotoxic agents were usually avoided in hospitalized patients with impaired baseline renal function or at risk of AKI. Because of the selection bias, the use of nephrotoxic agents was associated with decreased risk of AKI in univariate analysis and/or multivariate analysis. Forth, patients with history of recurrent AKI may be prone to developing AKI in the presence of UTI and urolithiasis. However, this is a retrospective study, data regarding the frequency of AKI episode before the study period was incomplete to determine their impact on the subsequent development of AKI in patients with UTI and urolithiasis. Fifth, serum bicarbonate was examined if patients develop severe AKI. Most of our patients did not experience severe AKI [overall 57 of 1113 patients (5.1%) had AKI stage 3], data of serum bicarbonate was incomplete for analysis of its relation with AKI.
In conclusion, we demonstrated that patients with ureteral stone complicated with hydronephrosis have a higher risk of developing AKI among UTI patients with urolithiasis, and urolithiasis remains a risk factor for AKI among UTI patients without hydronephrosis. Therefore, timely decompression of the renal collecting system for infectious hydronephrosis secondary to urolithiasis and complete stone removal after controlling infection are crucial for UTI patients with urolithiasis.
Methods
Patient selection
This retrospective observational study covered the period from January 2006 to April 2019 and was conducted at Chia-Yi Christian Hospital, a tertiary referral center in the southwestern part of Taiwan. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. This retrospective observational study was performed after obtaining ethical approval from the Institutional Review Board of Chiayi Christian Hospital (approval no. CYCH-IRB-2019061). This retrospective observational study was using de-identified and routine diagnosis/treatment data, thus CYCH-IRB-2019061 approved waiver of informed consent from all patients for being included in the study.
A total of 1113 consecutive hospitalized patients with UTI without any other concurrent infectious disease were enrolled. All enrolled patients fulfilled the following criteria: (a) with UTI symptoms and > 105 colony-forming units/mL of bacterial isolates from a urine specimen; (b) had available antimicrobial susceptibility test results; and (c) underwent complete imaging examination, including ultrasonography, intravenous urography, or computed tomography, and had complete data of the required laboratory tests. Patients aged < 18 years, with concurrent infection other than UTI, without imaging studies, with incomplete data, or undergoing regular dialysis therapy were excluded from this study. In patients with AKI, BUN/creatinine ratio was examined for pre-renal diseases, patients’ drug history was reviewed to find the use of nephrotoxic agents. All patients had received imaging survey to detect anatomical abnormality of urinary tract. Those patients who hydronephrosis was found by sonography study would receive CT scan to identify the etiology of hydronephrosis.
Inpatients were assessed using standard laboratory and diagnostic procedures. For further analysis, we collected clinical data in a standard form, including demographic characteristics (age and sex), comorbidities (coronary artery disease, CHF, stroke, DM, or hypertension), presence of an indwelling Foley catheter, vital signs (blood pressure and ear temperature), laboratory results (WBC count, platelet count, serum creatinine level, and eGFR at baseline and after hospitalization), prior history of UTI, existence of a urinary tract abnormality (urolithiasis or hydronephrosis), length of hospital stay, causative microorganisms (E. coli, Proteus species, Klebsiella species, Enterococcus species, and Pseudomonas species), antimicrobial resistance pattern, and the use of antibiotics or nephrotoxic agents.
Definition and examples of clinical covariates
The eGFR was determined using the Chronic Kidney Disease Epidemiology Collaboration creatinine equation and expressed in mL/min/1.73 m241,42. AKI was defined as an increase in serum creatinine to ≥ 2.0 times the baseline value according to the Kidney Disease: Improving Global Outcomes Clinical Practice Guideline criteria for serum creatinine value for AKI stages 2 and 343. Hydronephrosis was defined as dilatation of the renal pelvis and calyces in imaging studies. Uroseptic shock was defined as sepsis-induced hypotension (systolic blood pressure [SBP] < 90 mmHg or mean arterial pressure < 70 mmHg or a decrease in SBP by > 40 mmHg lasting for at least 1 h, despite adequate fluid resuscitation and in the absence of other causes of hypotension)44. An afebrile status was defined as a single temperature not increasing to > 38.3 °C (101°F)45. Nephrotoxic agents were defined as the use of nonsteroidal anti-inflammatory drugs, aminoglycosides, or contrast media. Multiple drug resistance (MDR) was defined as non-susceptibility to at least three antimicrobial categories 46.
Statistical analysis
All analyses were performed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are expressed as mean ± standard deviation, and categorical variables are expressed as number (percentage). Univariate analyses were performed using Student’s t-test and Mann–Whitney U-test for continuous variables, and the chi-square test and Fisher’s exact test for categorical variables. Multivariate logistic regression analyses were applied to identify risk factors associated with AKI during hospitalization. Only variables significant at the 0.05 level in univariate logistic regression analysis were selected for the subsequent multivariate analysis. The goodness-of-fit of the logistic regression model was assessed using the Cox & Snell test, and the explanatory power was reported with Nagelkerke’s pseudo-R-square. P < 0.05 was considered statistically significant.
References
Coe, F. L., Evan, A. & Worcester, E. Kidney stone disease. J. Clin. Invest. 115, 2598–2608 (2005).
Worcester, E. M. & Coe, F. L. Clinical practice: Calcium kidney stones. N. Engl. J. Med. 363, 954–963 (2010).
Scales, C. D. Jr., Smith, A. C., Hanley, J. M., Saigal, C. S., Urologic Diseases in America P. Prevalence of kidney stones in the United States. Eur. Urol. 62, 160–165 (2012).
Sakhaee, K. Nephrolithiasis as a systemic disorder. Curr. Opin. Nephrol. Hypertens. 17, 304–309 (2008).
Moe, O. W. Kidney stones: Pathophysiology and medical management. Lancet 367, 333–344 (2006).
Baker, L. R., Cattell, W. R., Fry, I. K. & Mallinson, W. J. Acute renal failure due to bacterial pyelonephritis. Q. J. Med. 48, 603–612 (1979).
Hsiao, C. Y. et al. Urolithiasis is a risk factor for uroseptic shock and acute kidney injury in patients with urinary tract infection. Front. Med. 6, 288 (2019).
Liborio, A. B., Leite, T. T., Neves, F. M., Teles, F. & Bezerra, C. T. AKI complications in critically ill patients: Association with mortality rates and RRT. Clin. J. Am. Soc. Nephrol. 10, 21–28 (2015).
Cohen, J., Cohen, S. & Grasso, M. Ureteropyeloscopic treatment of large, complex intrarenal and proximal ureteral calculi. BJU. Int. 111, 127–131 (2013).
Wagenlehner, F. M. E., Pilatz, A., Weidner, W. & Naber, K. G. Urosepsis: Overview of the diagnostic and treatment challenges. Microbiol. Spectr. 3, 0003 (2015).
Vahlensieck, W., Friess, D., Fabry, W., Waidelich, R. & Bschleipfer, T. Long-term results after acute therapy of obstructive pyelonephritis. Urol. Int. 94, 436–441 (2015).
Cox, C. E. & Hinman, F. Jr. Experiments with induced bacteriuria, vesical emptying and bacterial growth on the mechanism of bladder defense to infection. J. Urol. 86, 739–748 (1961).
Yongzhi, L. et al. Risk factors for urinary tract infection in patients with urolithiasis-primary report of a single center cohort. BMC Urol. 18, 45 (2018).
Lujan Galan, M. et al. Usefulness of ultrasonography in the assessment of acute pyelonephritis. Arch Esp. Urol. 50, 46–50 (1997).
Berger, I. et al. Emergency nephrectomy due to severe urosepsis: A retrospective, multicentre analysis of 65 cases. BJU Int. 104, 386–390 (2009).
Tambo, M., Okegawa, T., Shishido, T., Higashihara, E. & Nutahara, K. Predictors of septic shock in obstructive acute pyelonephritis. World J. Urol. 32, 803–811 (2014).
Lee, J. H., Lee, Y. M. & Cho, J. H. Risk factors of septic shock in bacteremic acute pyelonephritis patients admitted to an ER. J. Infect. Chemother. 18, 130–133 (2012).
Yamamichi, F., Shigemura, K., Kitagawa, K. & Fujisawa, M. Comparison between non-septic and septic cases in stone-related obstructive acute pyelonephritis and risk factors for septic shock: A multi-center retrospective study. J. Infect. Chemother. 24, 902–906 (2018).
Tang, X. & Lieske, J. C. Acute and chronic kidney injury in nephrolithiasis. Curr. Opin. Nephrol. Hypertens. 23, 385–390 (2014).
Rule, A. D., Krambeck, A. E. & Lieske, J. C. Chronic kidney disease in kidney stone formers. Clin. J. Am. Soc. Nephrol. 6, 2069–2075 (2011).
Bander, S. J., Buerkert, J. E., Martin, D. & Klahr, S. Long-term effects of 24-hr unilateral ureteral obstruction on renal function in the rat. Kidney Int. 28, 614–620 (1985).
Wang, S. J., Mu, X. N., Zhang, L. Y., Liu, Q. Y. & Jin, X. B. The incidence and clinical features of acute kidney injury secondary to ureteral calculi. Urol. Res. 40, 345–348 (2012).
Singh, S. M., Yadav, R., Gupta, N. P. & Wadhwa, S. N. The management of renal and ureteric calculi in renal failure. Br. J. Urol. 54, 455–457 (1982).
Holm-Nielsen, A., Jorgensen, T., Mogensen, P. & Fogh, J. The prognostic value of probe renography in ureteric stone obstruction. Br. J. Urol. 53, 504–507 (1981).
Yamamoto, Y. et al. Clinical characteristics and risk factors for septic shock in patients receiving emergency drainage for acute pyelonephritis with upper urinary tract calculi. BMC Urol. 12, 4 (2012).
Badia, M. et al. Mortality predictive factors in patients with urinary sepsis associated to upper urinary tract calculi. Med. Intensiva. 39, 290–297 (2015).
Rhodes, A. et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive. Care Med. 43, 304–377 (2017).
Brown, P. D. Management of urinary tract infections associated with nephrolithiasis. Curr. Infect. Dis. Rep. 12, 450–454 (2010).
Browne, R. F., Zwirewich, C. & Torreggiani, W. C. Imaging of urinary tract infection in the adult. Eur. Radiol. 14, E168-183 (2004).
Hamasuna, R. et al. Obstructive pyelonephritis as a result of urolithiasis in Japan: Diagnosis, treatment and prognosis. Int. J. Urol. 22, 294–300 (2015).
Chevalier, R. L., Thornhill, B. A. & Chang, A. Y. Unilateral ureteral obstruction in neonatal rats leads to renal insufficiency in adulthood. Kidney Int. 58, 1987–1995 (2000).
Lucarelli, G. et al. Delayed relief of ureteral obstruction is implicated in the long-term development of renal damage and arterial hypertension in patients with unilateral ureteral injury. J. Urol. 189, 960–965 (2013).
Heyns, C. F. Urinary tract infections in obstructionof the urinary tract. In Urogenital Infections 1st edn (eds Naber, K. G. et al.) 452–480 (European Association of Urology-International Consultation on Urological Diseases, 2010).
Zanetti, G. et al. Infections and urolithiasis: Current clinical evidence in prophylaxis and antibiotic therapy. Arch. Ital. Urol. Androl. 80, 5–12 (2008).
Tavichakorntrakool, R. et al. Extensive characterizations of bacteria isolated from catheterized urine and stone matrices in patients with nephrolithiasis. Nephrol. Dial. Transplant. 27, 4125–4130 (2012).
Kakinoki, H. et al. Risk factors for uroseptic shock in patients with urolithiasis-related acute pyelonephritis. Urol. Int. 100, 37–42 (2018).
Pertel, P. E. & Haverstock, D. Risk factors for a poor outcome after therapy for acute pyelonephritis. BJU Int. 98, 141–147 (2006).
Miano, R., Germani, S. & Vespasiani, G. Stones and urinary tract infections. Urol. Int. 79, 32–36 (2007).
Sammon, J. D. et al. Temporal trends, practice patterns, and treatment outcomes for infected upper urinary tract stones in the United States. Eur. Urol. 64, 85–92 (2013).
Mori, T., Shimizu, T. & Tani, T. Septic acute renal failure. Contrib. Nephrol. 166, 40–46 (2010).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150, 604–612 (2009).
National, K. F. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. 39, S1-266 (2002).
Kellum, J. et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group: KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2, 1–138 (2012).
Dellinger, R. P. et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2012. Crit. Care Med. 41, 580–637 (2013).
Dalal, S. & Zhukovsky, D. S. Pathophysiology and management of fever. J. Support Oncol. 4, 9–16 (2006).
Magiorakos, A. P. et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 18, 268–281 (2012).
Acknowledgements
The authors would like to acknowledge the support of Cheng-Lun Chiang.
Author information
Authors and Affiliations
Contributions
All authors participated in the interpretation of the studies and analysis of the data and also reviewed and approved the final version of the manuscript. C.H. protocol/project development; C.H. data collection or management; C.H. and T.C. manuscript writing/editing; C.H., T.C. and Y.L. data analysis; M.W. manuscript review; M.W. scientific advisor.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hsiao, CY., Chen, TH., Lee, YC. et al. Ureteral stone with hydronephrosis and urolithiasis alone are risk factors for acute kidney injury in patients with urinary tract infection. Sci Rep 11, 23333 (2021). https://doi.org/10.1038/s41598-021-02647-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-02647-8
This article is cited by
-
Integrated single-nucleus sequencing and spatial architecture analysis identified distinct injured-proximal tubular types in calculi rats
Cell & Bioscience (2023)
-
Comparison of image quality of two versions of deep-learning image reconstruction algorithm on a rapid kV-switching CT: a phantom study
European Radiology Experimental (2023)
-
Knowledge-map analysis of percutaneous nephrolithotomy (PNL) for urolithiasis
Urolithiasis (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.