Abstract
To study the acute psychological effects of Coronavirus Disease 2019 (COVID-19) outbreak among healthcare workers (HCWs) in China, a cross-sectional survey was conducted among HCWs during the early period of COVID-19 outbreak. The acute psychological effects including symptoms of depression, anxiety, and post-traumatic stress disorder (PTSD) were assessed using the Patient Health Questionnaire-9 (PHQ-9), the Generalized Anxiety Disorder (GAD-7) questionnaire, and the Impact of Event Scale-Revised (IES-R). The prevalence of depression, anxiety, and PTSD was estimated at 15.0%, 27.1%, and 9.8%, respectively. Having an intermediate technical title, working at the frontline, receiving insufficient training for protection, and lacking confidence in protection measures were significantly associated with increased risk for depression and anxiety. Being a nurse, having an intermediate technical title, working at the frontline, and lacking confidence in protection measures were risk factors for PTSD. Meanwhile, not worrying about infection was a protective factor for developing depression, anxiety, and PTSD. Psychological interventions should be implemented among HCWs during the COVID-19 outbreak to reduce acute psychological effects and prevent long-term psychological comorbidities. Meanwhile, HCWs should be well trained and well protected before their frontline exposure.
Similar content being viewed by others
Introduction
Infectious diseases are one of the biggest threats to human beings. In December 2019, a novel coronavirus-infected disease1,2,3, now named as the Coronavirus Disease 2019 (COVID-19) by the World Health Organization, occurred in Wuhan, Hubei Province, China, and rapidly become a global health emergency4. Within 1 month, the number of confirmed COVID-19 cases, since it was first publicly reported5, has exceeded the total number of confirmed severe acute respiratory syndrome (SARS) cases in 2003 in China. As of April 2, 2020, 81,620 confirmed COVID-19 cases and 3322 deaths has been reported by the National Health Commission of China6. The outbreak of COVID-19 has caused public panic and triggered psychological stress7.
Healthcare workers (HCWs), the key personnel for controlling and eliminating the outbreak of a severe infectious disease, are at high risk of infection. During the outbreak of SARS, Ebola virus disease, and the Middle East respiratory syndrome (MERS), hundreds of HCWs were infected and even died8,9,10. Due to the fear of being infected or death, HCWs can experience various acute psychological effects in the early period of an outbreak11, including symptoms of depression, anxiety, and post-traumatic stress disorder (PTSD)7. Meanwhile, they can also experience isolation from their families or community because of infection transmission risk and stigmatization11.
Since the outbreak of COVID-19, a large sum of HCWs in China immediately devoted themselves to the fight against COVID-19, and more HCWs are involved or prepared, as the virus rapidly transmitted during the Chinese Spring Festival travel season. Facing an emergency, HCWs can suffer from acute psychological effects. Moreover, the unpredictable future of this epidemic, large burden in the clinical treatment and care, and shortage of medical protective resources in the initial period of the outbreak may aggravate the acute psychological effects among HCWs.
To alleviate the acute psychological effects of HCWs, a psychological intervention program has been launched in China12. However, the lack of baseline data and the unexplored risk factors for the psychological well-being of HCWs may mislead the direction and limit the effect of psychological intervention. Furthermore, previous studies mainly focused on the long-term psychological comorbidities of an outbreak, and the acute psychological effects among HCWs have been studied less. Accordingly, we performed this cross-sectional study to assess the acute psychological effects experienced by HCWs during the early period of the COVID-19 outbreak in China. We mainly assessed the symptoms of depression, anxiety, and PTSD, and explored the related risk factors among HCWs. The findings of this study may provide crucial evidence for psychological intervention, as well as possibilities for further comparisons in future studies.
Subjects and methods
Study design and participants
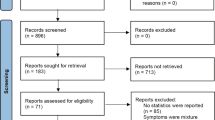
This was a survey-based cross-sectional study performed from January 29, 2020 to February 7, 2020 in China. The actual time during which we conducted this study is presented in Fig. 1. The target population was doctors or nurses working in hospitals that established fever clinics or wards for patients with COVID-19. HCWs were mainly recruited from Wuhan (the capital of Hubei Province), the epicenter city of COVID-19 in China. For comparison, HCWs were also recruited from other regions within Hubei Province (except Wuhan) and from other provinces in China. Wenjuanxing (www.wjx.cn), an anonymous online survey tool used in a previous study13, was employed to collect data. The sample size was computed via the formula14 N = Zα2P (1 − P)/d2, where α = 0.05 and Zα = 1.96. The estimated acceptable margin of error for proportion d was 0.1, and the prevalence (P) of respondents with psychological distress was estimated at 20%15. Finally, the minimum sample size was estimated at about 1600.
Data were obtained from the National Health Commission of China (Accessed on February 15, 2020, Available at: http://www.nhc.gov.cn/xcs/xxgzbd/gzbd_index.shtml).
This study was reviewed and approved by the Clinical Research Ethics Committee of Renmin Hospital of Wuhan University (WDRY2020-K004). Informed consent was obtained from all subjects prior to their enrollment by electronic way. Two options “yes/no” (whether subjects were willing to participate in the survey), were on the informed consent page, and only those who chose “yes” were taken to the questionnaire page. The anonymous survey had 74 required questions and took about 10 min. Respondents could terminate the survey at any time or during any question if they needed to. Participants or members of the public were not involved in the design, conduction, reporting, or dissemination plans of the study.
Outcome and covariates
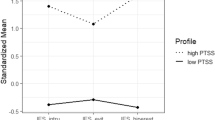
Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9)16. The instrument had been validated in the Chinese population and showed good reliability (Cronbach’s α = 0.89)17. The PHQ-9 included nine items, the total score ranged from 0 to 27, and a score of 10 or greater was defined as depression. Anxiety was measured using the seven-item Generalized Anxiety Disorder (GAD-7) questionnaire18. The GAD-7 has been found to have good reliability in the Chinese population (Cronbach’s coefficient of 0.89)19. The total score of the GAD-7 ranged from 0 to 21, and a score of greater than 6 was classified as anxiety. PTSD was assessed using the Impact of Event Scale-Revised (IES-R)20. It consisted of 22 items and included three subscales: intrusion, avoidance, and hyperarousal. The total IES-R score was calculated as the mean response across all items, while subscale scores were generated from the mean response across all items within the specific subscale. A cutoff mean score of 2 or higher indicated obvious distress for the total and subscale scores21. The IES-R had been validated in the Chinese populations; the Cronbach’s alpha coefficients for subscales were three subscales were 0.89 (Intrusion), 0.85 (Avoidance), and 0.83 (Hyperarousal), respectively22.
Occupational factors included occupation (doctor/nurse), technical title (junior, intermediate, and senior), and type of hospital (secondary/tertiary). Other occupational factors related to COVID-19 and nosocomial infection were acquired by the following questions, and the previous name (2019-nCoV) of COVID-19 was used in the survey:
-
(1)
Working position: Are you directly engaged in the diagnosis and treatment or nursing of patients with fever or 2019-nCoV pneumonia (yes/no)? Those who responded with “yes” or “no” were defined as frontline or second-line HCWs.
-
(2)
Enough training for protection: Do you think that you have received enough training on prevention of nosocomial infection for 2019-nCoV pneumonia (yes/no)?
-
(3)
Enough resources for protection: Do you have enough resources to be protected according to the latest guidelines for the prevention and control of 2019-nCoV nosocomial infection (yes, no)?
-
(4)
Confidence in protection measures: Do you think the latest guidelines for the prevention and control of 2019-nCoV nosocomial infection can protect you from infection (yes/no)?
-
(5)
Worry about infection: Do you worry about your vulnerability to infection (yes/no)?
Socioeconomic factors were: gender (male or female), age (years), marital status (unmarried, married, widowed, or devoiced), educational level (undergraduate or less, postgraduate, or more), and location (Wuhan, Hubei Province (except Wuhan), or other provinces).
Statistical analysis
Initially, 2367 completed questionnaires were received, with a response rate of 73.6%. The duration (seconds) to complete the questionnaire was recorded by Wenjuanxing. We excluded 346 questionnaires with a completion duration of less than 5 min (300 s) and more than 20 min (1200 s), to ensure that all questions had been well understood and completed consecutively by respondents. We further excluded 124 questionnaires from provinces that had recruited less than 20 participants. Totally, 470 questionnaires were excluded, leaving 1897 questionnaires for analysis. Respondents completing the included questionnaires and excluded questionnaires were comparable in age and sex.
Categorical data were presented as numbers (n)/percentage (%). The Chi-square test was used to compare the prevalence of depression, anxiety and PTSD between groups. Univariate regression analysis was conducted to determine whether any socioeconomic and occupational factors were associated with depression, anxiety, and PTSD. Binary logistic regression analysis was performed to examine the effects of occupational factors on depression, anxiety, and PTSD. The associations between potential risk factors and outcomes were presented as odds ratios (ORs) and 95% confidence intervals (CIs). Data analysis was conducted using SPSS version 20.0 (IBM Corp., Armonk, New York, United States). The significance level was set at α = 0.05.
Results
The 1897 HCWs consisted of 332 males (17.5%) and 1 565 females (82.5%). Most of the HCWs were aged 25–40 years (61.7%), married (67.5%), and had an educational level of undergraduate or less (84.8%). Nearly half of the HCWs (49.5%) were recruited from hospitals in Wuhan, 29.7% were doctors, 70.3% were nurses, 76.3% worked in tertiary hospitals, and 39.1% worked at the frontline against COVID-19. The majority of the HCWs had received sufficient training (71.0%) or had enough resources (78.8%) for protection, had confidence in the protection measure (68.4%), and worried about being infected (82.8%) (Table 1).
Overall, the prevalence of depression, anxiety, and PTSD was assessed at 15.0%, 27.1%, and 9.8%, respectively. The prevalence of depression, anxiety, and PTSD among HCWs working at the frontline was assessed at 21.7%, 38.5%, and 15.4%, respectively. A significantly higher prevalence of depression, anxiety, and PTSD was observed in HCWs that were females, working in Wuhan, working at the frontline, received insufficient training and recourses for protection, lack of confidence in protection measures, and worried about being infected (all p < 0.05). Nurses and those with an intermediate technical title had high prevalence of anxiety and PTSD (all p < 0.05). No statistical differences were detected among HCWs in different age groups, marital status, education level, and type of hospital (all p > 0.05) (Table 2).
Results of univariate logistic regression are presented in Table 3. Females, frontline HCWs, those who worked in Wuhan, had insufficient training and resources for protection, lacked confidence in protection measures, and worried about being infected were more likely to be afflicted with depression, anxiety, and PTSD. Nurses (vs. doctors) or those with an intermediate technical title (vs. junior technical title) were at higher risk of anxiety and PTSD.
The results of the binary logistic regression analysis are listed in Table 4. Controlling for potential confounding variables, intermediate technical title, working at the frontline, insufficient training for protection, and a lack of confidence in protection measures were significantly associated with an increased risk of depression and anxiety. Being a nurse, having an intermediate technical title, working at the frontline, and a lack of confidence in protection measures were risk factors for PTSD. Worry about infection was a risk factor for developing depression, anxiety, and PTSD. HCWs working in Hubei Province (except Wuhan) had a lower risk for anxiety than those who worked in Wuhan.
Discussion
Main findings
This cross-sectional study, based on 1897 participants assessed the acute psychological effects of the COVID-19 outbreak among HCWs in China. The prevalence of depression, anxiety, and PTSD in HCWs in the first month of COVID-19 outbreak was 15.0%, 27.1%, and 9.8%, respectively. Overall, females, and those who worked in Wuhan, worked at the frontline, had insufficient training and recourses for protection, lacked confidence in protection measures, and worried about being infected had a significantly higher prevalence of psychological effects. Generally, having an intermediate technical title, working at the frontline, insufficient training for protection, a lack of confidence in protection measures, and worry about infection were risk factors for depression, anxiety, and PTSD. In comparison with a recent study involving 1257 HCWs in China that identified factors associated with mental health outcomes among HCWs exposed to the COIVD-1923, our study firstly explored the association of several occupational factors with risk of acute psychological effects of the COVID-19 outbreak among HCWs with a larger sample size.
HCWs were at high risk of exposure to COVID-19, and were faced with increased levels of stress. In response to actual or possible threat, stress enhance the possibility of forming trauma-related memories24, and is a defining feature of PTSD25. Moreover, stress plays a critical role in the development and expression of many other psychiatric disorders25. Several pathways exist to establish the link between stress and psychiatric disorders, for instance, inflammation. There is evidence that psychological stress can trigger significant increases in inflammatory activity26. Notably, elevated concentrations of inflammatory signals, including cytokines and C-reactive protein, have been reported in patients with PTSD, generalized anxiety disorder, and depression27,28. However, because the pathophysiological mechanism is very complex, it is likely that many pathways act simultaneously to contribute to the psychiatric disorders.
Comparison with other studies
In our study, the prevalence of depression, anxiety, and PTSD was estimated at 15.0%, 27.1%, and 9.8%, respectively. The psychological effects of the COVID-19 outbreak seem to be less severe among HCWs than those of the SARS outbreak. According to a systematic review based on thirty-two studies involving 26,869 participants15, the estimated average rate of depression, anxiety, and PTSD during outbreaks of infectious disease (mainly SARS) was ~46% (ranging from 2329 to 74%30), 45% (ranging from 1931 to 77%30), and 21% (ranging from 1032 to 33%33), respectively. This difference between our study and previous ones may be attributed to the variations in measurement tools. For example, the Center for Epidemiologic Studies Depression Scale (CES-D) was used by Liu et al.29 while the Chinese Health Questionnaire (CHQ) was chose by Chong et al.30 for the assessment of depression, both of which differed from this study. Another possible explanation is that our study was conducted at the early stage of the outbreak, while studies regarding SARS were generally conducted at the late stage30 of the outbreak or after the outbreak had discharged31. The differences might reflect variations between the acute and long-term psychological effects triggered by an outbreak, and the prevalence of psychological stress among HCWs may increase after the initial period of an outbreak.
We found that HCWs with an intermediate technical title were at higher risk of anxiety and PTSD. One possible explanation was that HCWs with an intermediate technical title may be burdened with more work responsibility than those with a junior technical title, as well as longer work time in the wards than HCWs with a senior technical title. As a result, they may be associated with higher risk of psychological distress. In a previous study30, being both male and female gender were associated with being at risk for PTSD and anxiety, respectively. However, being female was associated with an increased risk for depression, anxiety, and PTSD only in our initial analysis. After controlling for confounders, the association was dismissed.
Another finding in our study was that working at the frontline was an independent risk factor for depression, anxiety, and PTSD, which has also been demonstrated by previous studies during the outbreak of severe acute respiratory syndrome (SARS) in 200329,30,34,35,36. It was indicated that HCWs working at the frontline should be the priority to receive psychological assistance. We also found that factors related to nosocomial infection, including insufficient training and recourses for protection, lack of confidence in protection measures, and worried about being infected, were generally found to be associated with psychological stress. Among these factors, previous studies indicated that lack of confidence in protection measures was a risk factor for anxiety37 while sufficient training protected against the development of anxiety31. This highlights the importance of essential training and good protection for preventing nosocomial infection in HCWs before they are faced with COVID-19 directly, to reduce the acute psychological effects.
Strengths and limitations
The primary strength of this study is the timing. We initiated this study when the confirmed cases of COVID-19 were increased rapidly and the narrow time period during which all of the participants completed the survey, with 98.8% of them completing it within 7 days (from January 29 to February 4, 2020) reflected the psychological effects of the COVID-19 outbreak among HCWs could be well. Second, we used THE PHQ-9, GAD-7, and IES-R to assess depression, anxiety, and PTSD, which have been validated in the Chinese population and show good reliability17,19,22. The three brief tools together consist of only 38 single-choice questions. The timesaving advantage makes them more acceptable for respondents to complete thoroughly, especially for the frontline HCWs. Another strength is that we had a larger sample size compared with previous studies that focused on the SARS outbreak 15. Thus, the results of the present study are robust and reliable.
The limitations of this study should also be acknowledged. First, the present study could not establish a causal relationship between potential risk factors and the acute psychological effects among HWCs because of the cross-sectional study design. Second, there is the possibility of selection bias, as the second-line HCWs tended to have more time and interest in participation, and thus the prevalence of acute psychological effects could be underestimated. However, because the study was conducted anonymously through an online tool with a response rate of 73.6%, information of those who declined to respond could not be collected, we therefore failed to assess the extent of potential selection bias. Third, HCWs may experience more psychological distress compared with the general population even without an outbreak of an infectious disease, and the status of psychological distress may vary overtime, whether HCWs suffered from more severe psychological burden during early exposure to COVID-19 than that before or after the COVID-19 epidemic remained unknown because of the lack of baseline and follow-up data.
Conclusions and policy implications
A proportion of HCWs suffer from acute psychological effects caused by the COVID-19 outbreak. High-risk HCWs for acute psychological effects were those with an intermediate technical title, working at the frontline, lacking training for protection, lacking confidence in protection measures, and worrying about being infected. Psychological interventions should be implemented among HCWs during the COVID-19 outbreak to reduce acute psychological effects and prevent long-term psychological comorbidities. Meanwhile, HCWs should be well trained and well protected before their frontline exposure.
References
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. https://doi.org/10.1016/s0140-6736(20)30183-5 (2020).
Li, Q. et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2001316 (2020).
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2001017 (2020).
Eurosurveillance Editorial, T. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro. Surveill. https://doi.org/10.2807/1560-7917.ES.2020.25.5.200131e (2020).
Wuhan Municipal Health Commission. Report of novel coronavirus-infected pneumonia in Wuhan. http://wjw.wuhan.gov.cn/front/web/showDetail/2020011209037 (2020).
National Health Commission of the People’s Republic of China. Report of the novel coronavirus-infected pneumonia in China up to April 2, 2020. http://www.nhc.gov.cn/xcs/yqfkdt/202004/4786774c1fd84e16b29d872f95241561.shtml (2020).
Bao, Y., Sun, Y., Meng, S., Shi, J. & Lu, L. 2019-nCoV epidemic: address mental health care to empower society. Lancet https://doi.org/10.1016/s0140-6736(20)30309-3 (2020).
World Health Organization. Ebola Situation Report WHO 30 September 2015. http://apps.who.int/ebola/ebola-situation-reports (2015).
Elkholy, A. A. et al. MERS-CoV infection among healthcare workers and risk factors for death: Retrospective analysis of all laboratory-confirmed cases reported to WHO from 2012 to 2 June 2018. J. Infect. Public Health https://doi.org/10.1016/j.jiph.2019.04.011 (2019).
Sepkowitz, K. A. & Eisenberg, L. Occupational deaths among healthcare workers. Emerg. Infect. Dis. 11, 1003–1008, https://doi.org/10.3201/eid1107.401038 (2005).
Van Bortel, T. et al. Psychosocial effects of an Ebola outbreak at individual, community and international levels. Bull. World Health Organ 94, 210–214 (2016).
Kang, L. et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. https://doi.org/10.1016/s2215-0366(20)30047-x (2020).
Wang, X. et al. Massive misuse of antibiotics by university students in all regions of China: implications for national policy. Int. J. Antimicrob. Agents 50, 441–446 (2017).
Huang, Y. et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 6, 211–224 (2019).
Vyas, K. J., Delaney, E. M., Webb-Murphy, J. A. & Johnston, S. L. Psychological impact of deploying in support of the US response to Ebola: a systematic review and meta-analysis of past outbreaks. Mil. Med. 181, E1515–E1531 (2016).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613 (2001).
Chen, S. et al. Validation of the nine-item Patient Health Questionnaire to screen for major depression in a Chinese primary care population. Asia Pac. Psychiatry 5, 61–68 (2013).
Spitzer, R. L., Kroenke, K., Williams, J. B. & Lowe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097 (2006).
Tong, X., An, D., McGonigal, A., Park, S. P. & Zhou, D. Validation of the generalized anxiety disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. 120, 31–36 (2016).
Weiss, D. S. In Cross-cultural Assessment of Psychological Trauma and PTSD pp. 219–238 (Springer, 2007).
Guo, J. et al. Suicidality associated with PTSD, depression, and disaster recovery status among adult survivors 8 years after the 2008 Wenchuan earthquake in China. Psychiatry Res. 253, 383–390 (2017).
Wu, K. K. & Chan, K. S. The development of the Chinese version of Impact of Event Scale-Revised (CIES-R). Soc. Psychiatry Psychiatr. Epidemiol. 38, 94–98 (2003).
Lai, J. et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 3, e203976–e203976 (2020).
Gonzalez, P. & Martinez, K. G. The role of stress and fear in the development of mental disorders. Psychiatr. Clin. North Am. 37, 535–546 (2014).
Maren, S. & Holmes, A. Stress and fear extinction. Neuropsychopharmacology 41, 58–79 (2016).
Glaser, R. & Kiecolt-Glaser, J. K. Stress-induced immune dysfunction: implications for health. Nat. Rev. Immunol. 5, 243–251 (2005).
Michopoulos, V., Powers, A., Gillespie, C. F., Ressler, K. J. & Jovanovic, T. Inflammation in fear- and anxiety-based disorders: PTSD, GAD, and beyond. Neuropsychopharmacology 42, 254–270 (2017).
Slavich, G. M. & Irwin, M. R. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol. Bull. 140, 774–815 (2014).
Liu, X. et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 53, 15–23 (2012).
Chong, M. Y. et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry 185, 127–133 (2004).
Lancee, W. J., Maunder, R. G. & Goldbloom, D. S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 59, 91–95 (2008).
Wu, P. et al. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol Alcohol 43, 706–712 (2008).
Su, T. P. et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 41, 119–130 (2007).
Maunder, R. G. et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom. Med. 66, 938–942 (2004).
McAlonan, G. M. et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatry 52, 241–247 (2007).
Poon, E. et al. Impact of severe respiratory syndrome on anxiety levels of front-line health care workers. Hong Kong Med. J. 10, 325–330 (2004).
Vinck, L. et al. Impact of the 2009 influenza A(H1N1) pandemic on public health workers in the Netherlands. Euro. Surveill. 16, 19793 (2011).
Acknowledgements
This work was supported by the National Key R&D Program of China (2018YFC1314600) as a grant for Z.L., from the Ministry of Science and Technology of People’s Republic of China (URL: http://www.most.gov.cn/). The funder played no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. We wish to express their gratitude to all investigators and participants of the studies included in this analysis.
Author information
Authors and Affiliations
Contributions
Z.L., Y.W., and S.M. designed the study and interpreted the results. C.Y., Z.C., S.H., and B.Z. conducted the primary analysis. S.T., H.B., X.G., J.W., H.D., L.K., H.T., R.L., L.Y., and G.W. contributed to literature search and assistance in analysis. Z.L., Y.W., and S.M. drafted the manuscript, and all authors contributed to the final version of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Ma, S., Yang, C. et al. Acute psychological effects of Coronavirus Disease 2019 outbreak among healthcare workers in China: a cross-sectional study. Transl Psychiatry 10, 348 (2020). https://doi.org/10.1038/s41398-020-01031-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-020-01031-w
This article is cited by
-
Work–family interference in urban China: gender discrimination and the effects of work–family balance policies
npj Urban Sustainability (2024)
-
Prevalence of post-traumatic stress disorder symptoms among patients with mental disorder during the COVID-19 pandemic
BMC Psychiatry (2022)
-
Mental health consequences during alerting situations and recovering to a new normal of coronavirus epidemic in 2019: a cross-sectional study based on the affected population
BMC Public Health (2021)