Abstract
Total hip and total knee replacements (THR and TKR respectively), the definitive treatments for end-stage arthritis, are both safe and extremely successful in relieving pain and improving function. However, physicians who care for patients with chronic hip and knee arthritis are often the 'gatekeepers' to total joint replacement (TJR) procedures as they select patients for referral to an orthopaedic surgeon to be considered for arthroplasty. Currently, no evidence-based criteria exist to guide physicians in this decision-making process, and this situation raises the possibility that conscious or unconscious biases may influence referral patterns, potentially leading to systematic inequities regarding which patients are eventually offered TJR. This article reviews why TJRs are particularly important procedures, and highlights common misperceptions among physicians regarding TJR risk assessment. This article also underscores the benefits of ongoing discussion regarding TJR with all patients with moderate-to-severe chronic hip or knee pain and disability.
Key Points
-
Hip and knee replacements are the definitive treatments for end-stage arthritis, providing excellent pain relief with minimal risks
-
Physicians who care for patients with chronic hip and knee arthritis function as 'gatekeepers,' determining who is referred for surgical consultation
-
Conscious or unconscious biases could influence referral patterns, leading to systematic inequities regarding who is considered for surgery
-
Data that should be considered when physicians contemplate the referral of patients for consideration of joint replacement are discussed
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Charnley, J. Arthroplasty of the hip. A new operation. Lancet 1, 1129–1132 (1961).
Mahomed, N. et al. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J. Bone Joint Surg. Am. 85 27–32 (2003).
Hawker, G. et al. Health-related quality of life after knee replacement. J. Bone Joint Surg. Am. 80, 163–173 (1998).
Karlson, E. W., Daltroy, L. H., Liang, M. H., Eaton, H. E. & Katz, J. N. Gender differences in patient preferences may underlie differential utilization of elective surgery. Am. J. Med. 102, 524–530 (1997).
Kurtz, S., Ong, K., Lau, E., Mowat, F. & Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Joint Surg. Am. 89, 780–785 (2007).
Kurtz, S. M. et al. Future clinical and economic impact of revision total hip and knee arthroplasty. J. Bone Joint Surg. Am. 89 (Suppl. 3), 144–151 (2007).
Wilson, N. A., Schneller, E. S., Montgomery, K. & Bozic, K. J. Hip and knee implants: current trends and policy considerations. Health Aff. (Millwood) 27, 1587–1598 (2008).
Hawker, G. A. et al. A population-based nested case–control study of the costs of hip and knee replacement surgery. Med. Care 47, 732–741 (2009).
Reichmann, W. M., Katz, J. N., Kessler, C. L., Jordan, J. M. & Losina, E. Determinants of self-reported health status in a population-based sample of persons with radiographic knee osteoarthritis. Arthritis Rheum. 61, 1046–1053 (2009).
Chang, R., Pellisier, J., Hazen, G. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA 275, 858–865 (1996).
HCUP interactive Database. Agency for Health Care Quality and Research. [online], (2009)
Lohmander, L. S., Englund, P. M., Dahl, L. L. & Roos, E. M. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am. J. Sports Med. 35, 1756–1769 (2007).
Marx, R. G., Jones, E. C., Angel, M., Wickiewicz, T. L. & Warren, R. F. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy 19, 762–770 (2003).
Felson, D. T Anderson, J. J., Naimark, A., Walker, A. M. & Meenan, R. F. Obesity and knee osteoarthritis The Framingham Study. Ann. Intern. Med. 109, 18–24 (1988).
Reijman, M. et al. Body mass index associated with onset and progression of osteoarthritis of the knee but not of the hip: the Rotterdam Study. Ann. Rheum. Dis. 66, 158–162 (2007).
Karlson, E. W. et al. Total hip replacement due to osteoarthritis: the importance of age, obesity, and other modifiable risk factors. Am. J. Med. 114, 93–98 (2003).
Wang, Y. C., McPherson, K., Marsh, T., Gortmaker, S. L. & Brown, M. Health and economic burden of the projected obesity trends in the USA and the, UK. Lancet 378, 815–825 (2011).
OECD. Obesity and the Economics of Prevention: Fit not Fat (OECD Publishing, Paris, 2010).
Ogden, C. L., Lamb, M. M., Carroll, M. D., Flegal, K. M. Obesity and socioeconomic status in children and adolescents: United States, 2005–2008. NCHS data brief 51, (2010).
Christensen, R., Astrup, A. & Bliddal, H. Weight loss: the treatment of choice for knee osteoarthritis? A randomized trial. Osteoarthritis Cartilage 13, 20–27 (2005).
Rehabilitation Institute of Chicago. Baby Boomers Expect to Beat the Odds with More Active, Longer Lives. Business Wire [online] (2003)
Losina, E., Thornhill, T. S., Rome, B. N., Wright, J. & Katz, J. N. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J. Bone Joint Surg. Am. 94, 201–207 (2012).
Lee, T. H. et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 100, 1043–1049 (1999).
Barrett, J. et al. Survival following total hip replacement. J. Bone Joint Surg. Am. 87, 1965–1971 (2005).
Basilico, F. C. et al. Risk factors for cardiovascular complications following total joint replacement surgery. Arthritis Rheum. 58, 1915–1920 (2008).
Hamel, M. B., Toth, M., Legedza, A. & Rosen, M. P. Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee: decision making, postoperative recovery, and clinical outcomes. Arch. Intern. Med. 168, 1430–1440 (2008).
Coyte, P. C., Hawker, G. & Wright, J. G. Variations in knee replacement utilization rates and the supply of health professionals in Ontario, Canada. J. Rheumatol. 23, 1214–1220 (1996).
Ang, D. C., Thomas, K. & Kroenke, K. An exploratory study of primary care physician decision making regarding total joint arthroplasty. J. Gen. Intern. Med. 22, 74–79 (2007).
Sturmer, T. et al. Differences in the views of orthopaedic surgeons and referring practitioners on the determinants of outcome after total hip replacement. J. Bone Joint Surg. Br. 87, 1416–1419 (2005).
Singh, J. A., Gabriel, S. E., Lewallen, D. G. Higher body mass index is not associated with worse pain outcomes after primary or revision total knee arthroplasty. J. Arthroplasty 26, 366–374 (2011).
Busato, A., Roder, C., Herren, S. & Eggli, S. Influence of high BMI on functional outcome after total hip arthroplasty. Obes. Surg. 18, 595–600 (2008).
Yeung, E. et al. The effect of obesity on the outcome of hip and knee arthroplasty. Int. Orthop. 35, 929–934 (2011).
Rajgopal, V. et al. The impact of morbid obesity on patient outcomes after total knee arthroplasty. J. Arthroplasty 23, 795–800 (2008).
Samson, A. J., Mercer, G. E. & Campbell, D. G. Total knee replacement in the morbidly obese: a literature review. ANZ J. Surg. 80, 595–599 (2010).
Chee, Y. H., Teoh, K. H., Sabnis, B. M., Ballantyne, J. A. & Brenkel, I. J. Total hip replacement in morbidly obese patients with osteoarthritis: results of a prospectively matched study. J. Bone Joint Surg. Br. 92, 1066–1071 (2010).
Lubbeke, A., Moons, K. G., Garavaglia, G., Hoffmeyer, P. Outcomes of obese and nonobese patients undergoing revision total hip arthroplasty. Arthritis Rheum. 59, 738–745 (2008).
Restrepo, C., Lettich, T., Roberts, N., Parvizi, J. & Hozack, W. J. Uncemented total hip arthroplasty in patients less than twenty-years. Acta Orthop. Belg. 74, 615–622 (2008).
Callaghan, J. J., Forest E. E., Olejniczak, J. P., Goetz, D. D. & Johnston, R. C. Charnley total hip arthroplasty in patients less than fifty years old. A twenty to twenty-five-year follow-up note. J. Bone Joint Surg. Am. 80, 704–714 (1998).
Joshi, A. B. et al. Long-term results of Charnley low-friction arthroplasty in young patients. J. Bone Joint Surg. Br. 75, 616–623 (1993).
Ritter, M. A., Lutgring, J. D., Davis, K. E., Faris, P. M. & Berend, M. E. Total knee arthroplasty effectiveness in patients 55 years old and younger: osteoarthritis vs. rheumatoid arthritis. The Knee 14, 9–11 (2007).
Dorr, L. D., Luckett, M. & Conaty, J. P. Total hip arthroplasties in patients younger than 45 years. A nine- to ten-year follow-up study. Clin. Orthop. Relat. Res. 260, 215–219 (1990).
Rolfson, O., Karrholm, J., Dahlberg, L. E. & Garellick, G. Patient-reported outcomes in the Swedish Hip Arthroplasty Register: results of a nationwide prospective observational study. J. Bone Joint Surg. Br. 93, 867–875 (2011).
Kurtz, S. M. et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin. Orthop. Relat. Res. 467, 2606–2612 (2009).
Nestle, M. Food marketing and childhood obesity—a matter of policy. N. Engl. J. Med. 354, 2527–2529 (2006).
Apold, H. et al. Weight gain and the risk of total hip replacement a population-based prospective cohort study of 265,725 individuals. Osteoarthritis Cartilage 19, 809–815 (2011).
Boettcher, W. G. Total hip arthroplasties in the elderly. Morbidity, mortality, and cost effectiveness. Clin. Orthop. Relat. Res. 274, 30–34 (1992).
Berend, M. E. et al. Total joint arthroplasty in the extremely elderly: hip and knee arthroplasty after entering the 89th year of life. J. Arthroplasty 18, 817–821 (2003).
Ogino, D. et al. Total hip replacement in patients eighty years of age and older. J. Bone Joint Surg. Am. 90, 1884–1890 (2008).
Karuppiah, S. V., Banaszkiewicz, P. A. & Ledingham, W. M. The mortality, morbidity and cost benefits of elective total knee arthroplasty in the nonagenarian population. Int. Orthop. 32, 339–343 (2008).
Singh, J. A. & Lewallen, D. Predictors of pain and use of pain medications following primary Total Hip Arthroplasty (THA): 5,707 THAs at 2-years and 3,289 THAs at 5-years. BMC Musculoskelet. Disord. 11, 90 (2010).
Birdsall, P. D. et al. Health outcome after total knee replacement in the very elderly. J. Bone Joint Surg. Br. 81, 660–662 (1999).
Anderson, J. G., Wixson, R. L., Tsai, D., Stulberg, S. D. & Chang, R. W. Functional outcome and patient satisfaction in total knee patients over the age of 75. J. Arthroplasty 11, 831–840 (1996).
Bischoff-Ferrari, H. A. et al. Psychosocial and geriatric correlates of functional status after total hip replacement. Arthritis Rheum. 51, 829–835 (2004).
Newington, D. P., Bannister, G. C. & Fordyce, M. Primary total hip replacement in patients over 80 years of age. J. Bone Joint Surg. Br. 72, 450–452 (1990).
Adam, R. F. & Noble, J. Primary total knee arthroplasty in the elderly. J. Arthroplasty 9, 495–497 (1994).
Jones, C. A., Voaklander, D. C., Johnston, D. W. & Suarez-Almazor, M. E. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch. Intern. Med. 161, 454–460 (2001).
SooHoo, N. F., Lieberman, J. R., Ko, C. Y. & Zingmond, D. S. Factors predicting complication rates following total knee replacement. J. Bone Joint Surg. Am. 88, 480–485 (2006).
Dieppe, P. Who should have a joint replacement? A plea for more 'phronesis'. Osteoarthritis Cartilage 19, 145–146 (2011).
Borkhoff, C. M. et al. The effect of patients' sex on physicians' recommendations for total knee arthroplasty. CMAJ 178, 681–687 (2008).
Hawker, G. A. et al. Differences between men and women in the rate of use of hip and knee arthroplasty. N. Engl. J. Med. 342, 1016–1022 (2000).
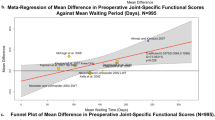
Fortin, P. R. et al. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis Rheum. 46, 3327–3330 (2002).
Gossec, L. et al. The role of pain and functional impairment in the decision to recommend total joint replacement in hip and knee osteoarthritis: an international cross-sectional study of 1909 patients. Report of the OARSI-OMERACT Task Force on total joint replacement. Osteoarthritis Cartilage 19, 147–154 (2011).
Dieppe, P. et al. Variations in the pre-operative status of patients coming to primary hip replacement for osteoarthritis in European orthopaedic centres. BMC Musculoskelet. Disord. 10, 19 (2009).
Hawker, G. The quest for explanations for race/ethnic disparity in rates of use of total joint arthroplasty. J. Rheumatol. 31, 1683–1685 (2004).
Hawker, G. A. et al. Determining the need for hip and knee arthroplasty: the role of clinical severity and patients' preferences. Med. Care 39, 206–216 (2001).
Skinner, J., Weinstein, J., Sporer, S. & Wennberg, J. Racial, ethnic, and geographic disparities in rates of knee arthroscopy among Medicare patients. N. Engl. J. Med. 349, 1350–1359 (2003).
Skinner, J., Weinstein, J. N., Sporer, S. M. & Wennberg, J. E. Racial, Ethnic, and geographic disparities in rates of knee arthroplasty among medicare patients. N. Engl. J. Med. 349, 1350–1359 (2003).
Ballantyne, P. J., Gignac, M. A. & Hawker, G. A. A patient-centered perspective on surgery avoidance for hip or knee arthritis: lessons for the future. Arthritis Rheum. 57, 27–34 (2007).
Clark, J. P. et al. The moving target: a qualitative study of elderly patients' decision-making regarding total joint replacement surgery. J. Bone Joint Surg. Am. 86, 1366–1374 (2004).
Brennan, S. et al. Cross-sectional analysis of association between socioeconomic status and utilization of primary total hip joint replacements 2006–2007: Australian Orthopaedic Association National Joint Replacement Registry. BMC Musculoskel. Dis. 13, 63 (2012).
Mancuso, C. A. et al. Patients' expectations of knee surgery. J. Bone Joint Surg. Am. 83, 1005–1012 (2001).
Acknowledgements
Thanks to Stuart Davidson for his help with graphics.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares no competing financial interests.
Rights and permissions
About this article
Cite this article
Mandl, L. Determining who should be referred for total hip and knee replacements. Nat Rev Rheumatol 9, 351–357 (2013). https://doi.org/10.1038/nrrheum.2013.27
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrrheum.2013.27
This article is cited by
-
Implementation of robotic-assisted total knee arthroplasty in the public health system: a comparative cost analysis
International Orthopaedics (2022)
-
The impact of surgical trainee involvement in total knee arthroplasty: a systematic review of surgical efficacy, patient safety, and outcomes
European Journal of Orthopaedic Surgery & Traumatology (2022)
-
Analgesic Impact of Single-Shot Versus Continuous Femoral Nerve Block After Total Knee Arthroplasty: A Systematic Review and Meta-Analysis
Advances in Therapy (2020)
-
Efficacy and safety of gyejigachulbutang (Gui-Zhi-Jia-Shu-Fu-Tang, Keishikajutsubuto, TJ-18) for knee pain in patients with degenerative knee osteoarthritis: a randomized, placebo-controlled, patient and assessor blinded clinical trial
Trials (2019)
-
Indication criteria for total hip or knee arthroplasty in osteoarthritis: a state-of-the-science overview
BMC Musculoskeletal Disorders (2016)