Abstract
Restorative proctocolectomy with ileal pouch–anal anastomosis has become the procedure of choice for the majority of patients with ulcerative colitis who require surgical treatment. Pouchitis, the most common long-term complication of the procedure, involves a spectrum of disease processes with heterogeneous risk factors, clinical features, disease courses and prognoses. In addition, clinical symptoms of pouchitis are not specific and often overlap with those of other inflammatory and functional pouch disorders, such as Crohn's disease of the pouch and irritable pouch syndrome. Pouchoscopy and biopsy, along with laboratory and radiographic evaluations, are often required for accurate diagnosis in patients with symptoms indicative of pouchitis. Dysbiosis has been implicated as a triggering factor for pouchitis, and concurrent infection with pathogens, such as Clostridium difficile, might contribute to disease relapse and exacerbation. Antibiotic therapy is the main treatment modality. However, the management of antibiotic-dependent and antibiotic-refractory pouchitis remains challenging. Secondary causes of pouchitis, such as ischaemia, NSAID use, the presence of concurrent primary sclerosing cholangitis and other systemic immune-mediated disorders, should be evaluated and properly managed.
Key Points
-
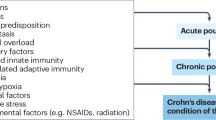
Pouchitis comprises a spectrum of disease, ranging from antibiotic-responsive forms to antibiotic-refractory entities, which involve various aetiological and pathogenetic pathways and have differing clinical presentations, disease courses and prognoses
-
Relapsing or chronic forms of pouchitis are also emerging
-
Dysbiosis (quantitative and/or qualitative alterations of the pouch microbiota) has a key role in the initiation and progression of pouchitis
-
Concurrent infections (such as Clostridium difficile) and other triggering factors (such as NSAID use) should be identified and treated or eradicated
-
Antibiotics are the mainstay of treatment for pouchitis
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Dhillon, S. et al. The natural history of surgery for ulcerative colitis in a population-based cohort from Olmsted County, Minnesota [abstract]. Am. J. Gastroenterol. 100, A819 (2005).
Melton, G. B. et al. Long-term outcomes with ileal pouch-anal anastomosis and Crohn's disease: pouch retention and implications of delayed diagnosis. Ann. Surg. 248, 608–616 (2008).
Hueting, W. E., Buskens, E., van der Tweel, I., Gooszen, H. G. & van Laarhoven, C. J. Results and complications after ileal pouch anal anastomosis: a meta-analysis of 43 observational studies comprising 9,317 patients. Dig. Surg. 22, 69–79 (2005).
Sandborn, W. J. Pouchitis following ileal pouch–anal anastomosis: definition, pathogenesis, and treatment. Gastroenterology 107, 1856–1860 (1994).
Winther, K. V., Jess T., Langholz, E., Munkholm, P. & Binder, V. Survival and cause-specific mortality in ulcerative colitis—follow-up of a population-based cohort in Copenhagen County. Gastroenterology 125, 1576–1582 (2003).
Tulchinsky, H., Hawley, P. R. & Nicholls, J. Long-term failure after restorative proctocolectomy for ulcerative colitis. Ann. Surg. 238, 229–234 (2003).
Belliveau, P., Trudel, J., Vasilevsky, C. A., Stein, B. & Gordon, P. H. Ileoanal anastomosis with reservoirs: complications and long-term results. Can. J. Surg. 42, 345–352 (1999).
Nicholls, R. J. Review article: ulcerative colitis—surgical indications and treatment. Aliment. Pharmacol. Ther. 16, 25–28 (2002).
Shen, B. et al. Comprehensive evaluation of inflammatory and non-inflammatory sequelae of ileal pouch–anal anastomosis. Am. J. Gastroenterol. 100, 93–101 (2005).
Penna, C. et al. Function of ileal J pouch–anal anastomosis in patients with familial adenomatous polyposis. Br. J. Surg. 80, 765–767 (1993).
Tjandra, J. J. et al. Similar functional results after restorative proctocolectomy in patients with familial adenomatous polyposis and mucosal ulcerative colitis. Am. J. Surg. 165, 322–325 (1993).
Penna, C. et al. Pouchitis after ileal pouch–anal anastomosis for ulcerative colitis occurs with increased frequency in patients with associated primary sclerosing cholangitis. Gut 38, 234–239 (1996).
Fazio, V. W. et al. Ileal pouch–anal anastomosis complications and function in 1005 patients. Ann. Surg. 222, 120–127 (1995).
Ferrante, M. et al. Outcome after proctocolectomy with ileal pouch–anal anastomosis for ulcerative colitis. Inflamm. Bowel Dis. 14, 20–28 (2008).
Fleshner, P. et al. Both preoperative perinuclear antineutrophil cytoplasmic antibody and anti-CBir1 expression in ulcerative colitis patients influence pouchitis development after ileal pouch–anal anastomosis. Clin. Gastroenterol. Hepatol. 6, 561–568 (2008).
Stocchi, L. & Pemberton, J. H. Pouch and pouchitis. Gastroenterol. Clin. North Am. 30, 223–241 (2001).
Gionchetti, P. et al. Prophylaxis of pouchitis onset with probiotic therapy: a double-blind placebo controlled trial. Gastroenterology 124, 1202–1209 (2003).
Abdelrazeq, A. S. et al. Predictors for acute and chronic pouchitis following restorative proctocolectomy for ulcerative colitis. Colorectal Dis. 10, 805–813 (2008).
Shen, B., Remzi, F. H., Lavery, I. C., Lashner, B. A. & Fazio, V. W. A proposed classification of ileal pouch disorders and associated complications after restorative proctocolectomy. Clin. Gastroenterol. Hepatol. 6, 145–158 (2008).
Zoetendal, E. G., Rajilic-Stojanovic, M. & De Vos, W. M. High-throughput diversity and functionality analysis of the gastrointestinal tract microbiota. Gut 57, 1605–1615 (2008).
Falk, A. et al. Ileal pelvic pouch microbiota from two former ulcerative colitis patients, analysed by DNA-based methods, were unstable over time and showed the presence of Clostridium perfringens. Scand. J. Gastroenterol. 42, 973–985 (2007).
Lim, M. et al. An assessment of bacterial dysbiosis in pouchitis using terminal restriction fragment length polymorphisms of 16S ribosomal DNA from pouch effluent microbiota. Dis. Colon Rectum 52, 1492–1500 (2009).
Atila, K. et al. Partially hydrolyzed guar gum attenuates the severity of pouchitis in a rat model of ileal J pouch–anal anastomosis. Dig. Dis. Sci. 54, 522–529 (2009).
Chen, C. N. et al. Anatomic and functional characteristics of the rat ileal pouch. Am. J. Surg. 183, 464–470 (2002).
Lim, M., Sagar, P., Finan, P., Burke, D. & Schuster, H. Dysbiosis and pouchitis. Br. J. Surg. 93, 1325–1334 (2006).
Duffy, M. et al. Sulfate-reducing bacteria colonize pouches formed for ulcerative colitis but not for familial adenomatous polyposis. Dis. Colon Rectum 45, 384–388 (2002).
Nasmyth, D. G., Godwin, P. G. R., Dixon, M. F., Williams, N. S. & Johnston, D. Ileal ecology after pouch anal anastomosis or ileostomy. Gastroenterology 96, 817–824 (1989).
Komanduri, S., Gillevet, P. M., Sikaroodi, M., Mutlu, E. & Keshavarzian, A. Dysbiosis in pouchitis: evidence of unique microfloral patterns in pouch inflammation. Clin. Gastroenterol. Hepatol. 5, 352–360 (2007).
Sokol, H., Lay, C., Seksik, P. & Tannock, G. W. Analysis of bacterial bowel communities of IBD patients: what has it revealed? Inflamm. Bowel Dis. 14, 858–867 (2008).
Ferrante, M. et al. Development of pouchitis following ileal pouch–anal anastomosis (IPAA) for ulcerative colitis: a role for serological markers and microbial pattern recognition receptor genes. J. Crohns Colitis 2, 142–151 (2008).
Gionchetti, P. et al. Oral bacteriotherapy as maintenance treatment in patients with chronic pouchitis: a double-blind, placebo-controlled trial. Gastroenterology 119, 305–309 (2000).
Mimura, T. et al. Once daily high dose probiotic therapy (VSL#3®) for maintaining remission in recurrent or refractory pouchitis. Gut 53, 108–114 (2004).
Gionchetti, P. et al. High-dose probiotics for the treatment of active pouchitis. Dis. Colon Rectum 50, 2075–2084 (2007).
Elahi, B., Nikfar, S., Derakhshani, S., Vafaie, M. & Abdollahi, M. On the benefit of probiotics in the management of pouchitis in patients underwent ileal pouch anal anastomosis: a meta-analysis of controlled clinical trials. Dig. Dis. Sci. 53, 1278–1284 (2008).
Kühbacher, T. et al. Bacterial and fungal microbiota in relation to probiotic therapy (VSL#3) in pouchitis. Gut 55, 833–841 (2006).
Madden, M. V., McIntyre, A. S. & Nicholls, R. J. Double-blind crossover trial of metronidazole versus placebo in chronic unremitting pouchitis. Dig. Dis. Sci. 39, 1193–1196 (1994).
Shen, B. et al. A randomized trial of ciprofloxacin and metronidazole in treating acute pouchitis. Inflamm. Bowel Dis. 7, 301–305 (2001).
Andersone, A. F. et al. Comparative analysis of human gut microbiota by barcoded pyrosequencing. PLoS ONE 3, e2836 (2008).
McLaughlin, S. D. et al. The bacteriology of pouchitis: a molecular phylogenetic analysis using 16S rRNA gene cloning and sequencing. Ann. Surg. 252, 90–98 (2010).
Ohge, H. et al. Association between fecal hydrogen sulfide production and pouchitis. Dis. Colon Rectum 48, 469–475 (2005).
Gosselink, M. P. et al. Eradication of pathogenic bacteria and restoration of normal pouch flora: comparison of metronidazole and ciprofloxacin in the treatment of pouchitis. Dis. Colon Rectum 47, 1519–1525 (2004).
Kohyama, A. et al. Bacterial population moves toward a colon-like community in the pouch after total proctocolectomy. Surgery 145, 435–447 (2009).
Almeida, M. G. et al. Intestinal mucosa-associated microflora in ulcerative colitis patients before and after restorative proctocolectomy with an ileoanal pouch. Dis. Colon Rectum 51, 1113–1119 (2008).
Shen, B. et al. Clostridium difficile infection in patients with ileal pouch–anal anastomosis. Clin. Gastroenterol. Hepatol. 6, 782–788 (2008).
Kyne, L., Warny, M., Qamar, A. & Kelly, C. P. Association between antibody response to toxin A and protection against recurrent Clostridium difficile diarrhea. Lancet 357, 189–193 (2001).
Kelly, C. P., Pothoulakis, C., Orellana, J. & LaMont, J. T. Human colonic aspirates containing immunoglobulin A antibody to Clostridium difficile toxin A inhibit toxin A–receptor binding. Gastroenterology 102, 35–40 (1992).
Leung, D. Y. et al. Treatment with intravenously administered gamma globulin of chronic relapsing colitis induced by Clostridium difficile toxin. J. Pediatr. 118, 633–637 (1997).
Warny, M., Vaerman, J. P., Avesani, V. & Delmee, M. Human antibody response to Clostridium difficile toxin A in relation to clinical course of infection. Infect. Immun. 62, 384–389 (1994).
Aronsson, B., Granstrom, M., Mollby, R. & Nord, C. E. Serum antibody response to Clostridium difficile toxins in patients with Clostridium difficile diarrhoea. Infection 13, 97–101 (1985).
Shen, B. Campylobacter infection in patients with ileal pouches. Am. J. Gastroenterol. 105, 472–473 (2010).
Ingram, S., McKinley, J. M., Vasey, F., Carter, J. D. & Brady, P. G. Are inflammatory bowel disease (IBD) and pouchitis a reactive enteropathy to group D streptococci (enterococci)? Inflamm. Bowel Dis. 15, 1609–1610 (2009).
DeSilva, H. J. et al. Lymphocyte and macrophage subpopulations in pelvic ileal reservoirs. Gut 32, 1160–1165 (1991).
Muñoz-Juarez, M., Pemberton, J. H., Sandborn, W. J., Tremaine, W. J. & Dozois, R. R. Misdiagnosis of specific cytomegalovirus infection of ileoanal pouch as a refractory idiopathic chronic pouchitis. Report of two cases. Dis. Colon Rectum 42, 117–120 (1999).
Moonka, D., Furth, E. E., MacDermott, R. P. & Lichtenstein, G. R. Pouchitis associated with primary cytomegalovirus infection. Am. J. Gastroenterol. 93, 264–266 (1998).
Kroesen, A. J. et al. Increased bacterial permeation in long-lasting ileoanal pouches. Inflamm. Bowel Dis. 12, 736–744 (2006).
Hirata, I., Berrebi, G., Austin, L. L., Keren, D. F. & Dobbins, W. O. 3rd. Immunohistological characterization of intraepithelial and lamina propria lymphocytes in control ileum and colon and inflammatory bowel disease. Dig. Dis. Sci. 31, 593–603 (1986).
Stallmach, A. et al. Increased state of activation of CD4 positive T cells and elevated interferon gamma production in pouchitis. Gut 43, 499–505 (1998).
Thomas, P. D., Forbes, A., Nicholls, R. J. & Ciclitira, P. Altered expression of the lymphocyte activation markers CD30 and CD27 in patients with pouchitis. Scand. J. Gastroenterol. 36, 258–264 (2001).
Goldberg, P. A. et al. Leukocyte typing, cytokine expression and epithelial turn over in the ileal pouch in patients with ulcerative colitis and familial adenomatous polyposis. Gut 38, 549–553 (1996).
Toiyama, T. et al. The expression patterns of Toll-like receptors in the ileal pouch mucosa of postoperative ulcerative colitis patients. Surg. Today 36, 287–290 (2006).
Heuschen, G. et al. Differential expression of Toll-like receptor 3 and 5 in ileal pouch mucosa of ulcerative colitis patients. Int. J. Colorectal Dis. 22, 293–301 (2007).
Salzman, N. H., Ghosh, D., Huttner, K. M., Paterson, Y. & Bevins, C. L. Protection against enteric salmonellosis in transgenic mice expressing a human intestinal defensin. Nature 422, 522–526 (2003).
Scarpa, M. et al. TLR2 and TLR4 up-regulation and colonization of the ileal mucosa by Clostridiaceae spp. in chronic/relapsing pouchitis. J. Surg. Res. 169, e145–e154 (2011).
Porter, E., van Dam, E., Valore, E. & Ganz, T. Broad spectrum antimicrobial activity of human intestinal defensin 5. Infect. Immun. 65, 2396–2401 (1997).
Ayabe, T. et al. Secretion of microbicidal α-defensins by intestinal Paneth cells in response to bacteria. Nat. Immunol. 1, 113–118 (2000).
Wehkamp, J. et al. Decreased Paneth cell defensins and antimicrobial activity in ileal Crohn's disease. Proc. Natl Acad. Sci. USA 102, 18129–18134 (2005).
Hirata, N. et al. Proliferation of immature plasma cells in pouchitis mucosa in patients with ulcerative colitis. Inflamm. Bowel Dis. 14, 1084–1090 (2008).
Patel, R. T., Bain, I., Youngs, D. & Keighley, M. R. B. Cytokine production in pouchitis is similar to that in ulcerative colitis. Dis. Colon Rectum 38, 831–837 (1995).
Schmidt, C. et al. Increased cytokine transcripts in pouchitis reflect the degree of inflammation but not the underlying entity. Int. J. Colorectal Dis. 21, 419–426 (2006).
Gionchetti, P. et al. Mucosal concentrations of interleukin-1β, interleukin-6, interleukin-8, and tumor necrosis factor-α in pelvic ileal pouches. Dig. Dis. Sci. 39, 1525–1531 (1994).
Bulois, P. et al. Pouchitis is associated with mucosal imbalance between interleukin-8 and interleukin-10. Inflamm. Bowel Dis. 6, 157–164 (2000).
Patel, R. T., Pall, A. A., Adu, D. & Keighley M. R. B. Circulating soluble adhesion molecules in inflammatory bowel disease. Eur. J. Gastroenterol. Hepatol. 7, 1037–1041 (1995).
Chaussade S. et al. Presence of PAF-acether in stool of patients with pouch ileoanal anastomosis and pouchitis. Gastroenterology 100, 1509–1514 (1991).
Gertner, D. J. et al. Increased leukotriene B4 release from ileal pouch mucosa in ulcerative colitis compared with familial adenomatous polyposis. Gut 35, 1429–1432 (1994).
Romano, M. et al. Vascular endothelial growth factor and cyclooxygenase-2 are overexpressed in ileal pouch–anal anastomosis. Dis. Colon Rectum 50, 650–659 (2007).
Leal, R. F. et al. Differential expression of pro-inflammatory cytokines and a pro-apoptotic protein in pelvic ileal pouches for ulcerative colitis and familial adenomatous polyposis. Tech. Coloproctol. 12, 33–38 (2008).
Stucchi, A. F. et al. A neurokinin 1 receptor antagonist reduces an ongoing ileal pouch inflammation and the response to a subsequent inflammatory stimulus. Am. J. Physiol. Gastrointest. Liver Physiol. 285, G1259–G1267 (2003).
Stallmach, A. et al. Comparable expression of matrix metalloproteinases 1 and 2 in pouchitis and ulcerative colitis. Gut 47, 415–422 (2000).
Ulisse, S. et al. Expression of cytokine, inducible nitric oxide synthase, matrix metalloproteinases in pouchitis: effects of probiotic therapy. Am. J. Gastroenterol. 96, 2691–2699 (2001).
Leal, R. F. et al. Activation of signal transducer and activator of transcription-1 (STAT-1) and differential expression of interferon-γ and anti-inflammatory proteins in pelvic ileal pouches for ulcerative colitis and familial adenomatous polyposis. Clin. Exp. Immunol. 160, 380–385 (2010).
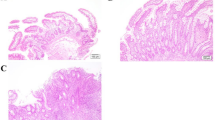
Shepherd, N. A. et al. Distribution of mucosal morphology and an assessment of colonic phenotype change in the pelvic ileal reservoir. Gut 34, 101–105 (1993).
Biancone, L. et al. Tropomyosin expression in the ileal pouch: a relationship with the development of pouchitis in ulcerative colitis. Am. J. Gastroenterol. 98, 2719–2726 (2003).
Coffey, J. C. et al. Pathogenesis of and unifying hypothesis for idiopathic pouchitis. Am. J. Gastroenterol. 104, 1013–1023 (2009).
De Preter, V. et al. Pouchitis, similar to active ulcerative colitis, is associated with impaired butyrate oxidation by intestinal mucosa. Inflamm. Bowel Dis. 15, 335–340 (2009).
Tysk, C. et al. Colonic glycoproteins in monozygote twins with inflammatory bowel disease. Gastroenterology 100, 419–423 (1991).
Merrett, M. N., Soper, N., Mortensen, N. & Jewell, D. P. Intestinal permeability in the ileal pouch. Gut 39, 226–230 (1996).
Sandborn, W. J. Pouchitis: risk factors, frequency, natural history, classification and public health prospective. In Trends in inflammatory bowel disease therapy, 1996 (eds McLeod R. S. et al.) 51–63 (Kluwer Academic Publishers, Lancaster, UK, 1997).
Shen, B. Diagnosis and management of patients with pouchitis. Drugs 63, 453–461 (2003).
Lammers, K. M. et al. Combined carriership of TLR9–1237C and CD14–260T alleles enhances the risk for developing chronic relapsing pouchitis. World J. Gastroenterol. 11, 7323–7329 (2005).
Lohmuller, J. L., Pemberton, H. J., Dozois, R. R., Ilstrup, D. & van Heerden, J. Pouchitis and extraintestinal manifestations of inflammatory bowel disease after ileal pouch–anal anastomosis. Ann. Surg. 211, 622–629 (1990).
Mowschenson, P. M., Critchlow, J. F. & Peppercorn, M. A. Ileoanal pouch operation: long-term outcome with or without diverting ileostomy. Arch. Surg. 135, 463–465 (2000).
Hurst, R. D., Chung, T. P., Rubin, M. & Michelassi, F. Implications of acute pouchitis on the long-term functional results after restorative proctocolectomy. Inflamm. Bowel Dis. 4, 280–284 (1998).
Madiba, T. E. & Bartolo, D. C. Pouchitis following restorative proctocolectomy for ulcerative colitis: incidence and therapeutic outcome. J. R. Coll. Surg. Edinb. 46, 334–337 (2001).
Carter, M. J. et al. The interleukin 1 receptor antagonist gene allele 2 as a predictor of pouchitis following colectomy and IPAA in ulcerative colitis. Gastroenterology 121, 805–811 (2001).
Meier, C. B. et al. Innate immune receptor genetic polymorphisms in pouchitis: is NOD2/CARD15 a susceptibility factor? Inflamm. Bowel Dis. 11, 965–971 (2005).
Fleshner, P. R. et al. High level perinuclear antineutrophil cytoplasmic antibody (pANCA) in ulcerative colitis patients before colectomy predicts the development of chronic pouchitis after ileal pouch–anal anastomosis. Gut 49, 671–677 (2001).
Shen, B. et al. Risk factors for diseases of ileal pouch-anal anastomosis in patients with ulcerative colitis. Clin. Gastroenterol. Hepatol. 4, 81–89 (2006).
Hoda, K. M., Collins, J. F., Knigge, K. L. & Deveney, K. E. Predictors of pouchitis after ileal pouch–anal anastomosis: a retrospective review. Dis. Colon Rectum 51, 554–560 (2008).
Schmidt, C. M., Lazenby, A. J., Hendrickson, R. J. & Sitzmann, J. V. Pre-operative terminal ileal and colonic resection histopathology predicts risk of pouchitis in patients after ileoanal pull-through procedure. Ann. Surg. 227, 654–662 (1998).
Achkar, J. P. et al. Differentiating risk factors for acute and chronic pouchitis. Clin. Gastroenterol. Hepatol. 3, 60–66 (2005).
Shen, B. et al. Association between immune-associated disorders and adverse outcomes of ileal pouch–anal anastomosis. Am. J. Gastroenterol. 104, 655–664 (2009).
Okon, A. et al. Elevated platelet count before ileal pouch–anal anastomosis for ulcerative colitis is associated with the development of chronic pouchitis. Am. Surg. 71, 821–826 (2005).
Hata, K., Watanabe, T., Shinozaki, M. & Nagawa, H. Patients with extraintestinal manifestations have a higher risk of developing pouchitis in ulcerative colitis: multivariate analysis. Scand. J. Gastroenterol. 38, 1055–1058 (2003).
Lepistö, A., Kärkkäinen, P. & Järvinen, H. J. Prevalence of primary sclerosing cholangitis in ulcerative colitis patients undergoing proctocolectomy and ileal pouch–anal anastomosis. Inflamm. Bowel Dis. 14, 775–779 (2008).
Kuisma, J., Järvinen, H., Kahri, A. & Färkkillä, M. Factors associated with disease activity of pouchitis after surgery for ulcerative colitis. Scand. J. Gastroenterol. 39, 544–548 (2004).
Fleshner, P. et al. A prospective multivariate analysis of clinical factors associated with pouchitis after ileal pouch–anal anastomosis. Clin. Gastroenterol. Hepatol. 5, 952–958 (2007).
Boyko, E. J., Koepsell, T. D., Perera, D. R. & Inui, T. S. Risk of ulcerative colitis among former and current cigarette smokers. N. Engl. J. Med. 316, 707–710 (1987).
Mathis, K. L. et al. Ileal pouch–anal anastomosis and liver transplantation for ulcerative colitis complicated by primary sclerosing cholangitis. Br. J. Surg. 95, 882–886 (2008).
Cho, C. S. et al. Proctocolectomy–ileal pouch–anal anastomosis for ulcerative colitis after liver transplantation for primary sclerosing cholangitis: a multi-institutional analysis. J. Gastrointest. Surg. 12, 1221–1226 (2008).
Shen, B. et al. Primary sclerosing cholangitis is associated with endoscopic and histologic inflammation of the distal afferent limb in patients with ileal pouch–anal anastomosis. Inflamm. Bowel Dis. 17, 1890–1900 (2011).
Zins, B. J. et al. Pouchitis disease course after orthotopic liver transplantation in patients with primary sclerosing cholangitis and an ileal pouch–anal anastomosis. Am. J. Gastroenterol. 90, 2177–2181 (1995).
Freeman, K. et al. Orthotopic liver transplantation for primary sclerosing cholangitis in patients with ulcerative colitis: impact on occurrence of chronic pouchitis. Clin. Gastroenterol. Hepatol. 6, 62–68 (2008).
Shen, B. et al. Endoscopic and histologic evaluations together with symptom assessment are required to diagnose pouchitis. Gastroenterology 121, 261–267 (2001).
Moskowitz, R. L., Shepherd, N. A. & Nicholls, R. J. An assessment of inflammation in the reservoir after restorative proctocolectomy with ileoanal ileal reservoir. Int. J. Colorectal Dis. 1, 167–174 (1986).
Mowat, C. et al. Guidelines for the management of inflammatory bowel disease in adults. Gut 60, 571–607 (2011).
Sandborn, W. J., Tremaine, W. J., Batts, K. P., Pemberton, J. H. & Phillips, S. F. Pouchitis after ileal pouch–anal anastomosis: a pouchitis disease activity index. Mayo Clin. Proc. 69, 409–415 (1994).
McLaughlin, S. D. et al. Guide to endoscopy of the ileo-anal pouch following restorative proctocolectomy with ileal pouch–anal anastomosis; indications, technique, and management of common findings. Inflamm. Bowel Dis. 15, 1256–1263 (2009).
Kariv, R. et al. Preoperative colorectal neoplasia increases the risk for pouch neoplasia in patients with restorative proctocolectomy. Gastroenterology 139, 806–812 (2010).
Shen, B. et al. Efficacy and safety of endoscopic treatment of ileal pouch strictures. Inflamm. Bowel Dis. 17, 2527–2535 (2011).
Shen, B. et al. Endoscopic and histologic evaluations together with symptom assessment are required for the diagnosis of pouchitis. Gastroenterology 121, 261–267 (2001).
Kariv, R. et al. Pyloric gland metaplasia and pouchitis in patients with ileal pouch–anal anastomosis. Aliment. Pharmacol. Ther. 31, 862–873 (2010).
Shen, B. et al. Asymmetric inflammation of ileal pouch: a sign of ischemic pouchitis? Inflamm. Bowel Dis. 16, 836–846 (2010).
Joyce, M. R. et al. Ileal pouch prolapse: prevalence, management, and outcomes. J. Gastrointest. Surg. 14, 993–997 (2010).
Navaneethan, U. et al. Infiltration of IgG4+ plasma cells in symptomatic patients with ileal pouch–anal anastomosis. J. Crohns Colitis 5, 570–576 (2011).
Navaneethanm, U. et al. Risk factors for abnormal liver function tests in patients with ileal pouch-anal anastomosis for underlying inflammatory bowel disease. Am. J. Gastroenterol. 104, 2467–2475 (2009).
Shen, B. et al. Effect of withdrawal of non-steroidal anti-inflammatory drug use in patients with the ileal pouch. Dig. Dis. Sci. 52, 3321–3328 (2007).
Parsi, M. A. et al. Fecal lactoferrin for diagnosis of symptomatic patients with ileal pouch–anal anastomosis. Gastroenterology 126, 1280–1286 (2004).
Lim, M. et al. The assessment of a rapid noninvasive immunochromatographic assay test for fecal lactoferrin in patients with suspected inflammation of the ileal pouch. Dis. Colon Rectum 51, 96–99 (2008).
Johnson, M. W. et al. Faecal calprotectin: a noninvasive diagnostic tool and marker of severity in pouchitis. Eur. J. Gastroenterol. Hepatol. 20, 174–179 (2008).
Lian, L., Remzi, F. H., Fazio, V. W. & Shen, B. False positive celiac serology is associated with chronic pouchitis in patients with ulcerative colitis. Dis. Colon Rectum 53, 1446–1451 (2010).
Navaneethan, U. et al. Elevated serum IgG4 is associated with chronic antibiotic-refractory pouchitis. J. Gastrointest. Surg. 15, 1556–1561 (2011).
Navaneethan, U. et al. Prevalence and clinical implications of positive anti-microsomal antibodies in patients with symptomatic ileal pouches. J. Gastrointest. Surg. 15, 1577–1582 (2011).
Gosselink, M. P. et al. Delay of the first onset of pouchitis by oral intake of the probiotic strain Lactobacillus rhamnosus GG. Dis. Colon Rectum 47, 876–884 (2004).
Ha, C. Y. et al. Early institution of tinidazole may prevent pouchitis following ileal pouch anal anastomosis (IPAA) surgery in ulcerative colitis (UC) patients [abstract 488]. Gastroenterology 138 (Suppl. 1), S-69 (2010).
McLaughlin, S. D. et al. An open study of antibiotics for the treatment of pre-pouch ileitis following restorative proctocolectomy with ileal pouch–anal anastomosis. Aliment. Pharmacol. Ther. 29, 69–74 (2009).
McLaughlin, S. D. et al. Fecal coliform testing to identify effective antibiotic therapies for patients with antibiotic-resistant pouchitis. Clin. Gastroenterol. Hepatol. 7, 545–548 (2009).
Shen, B. et al.The efficacy and tolerability of AST-120 (spherical carbon adsorbent) in active pouchitis. Am. J. Gastroenterol. 104, 1468–1474 (2009).
Navaneethan, U. et al. Impact of budesonide on liver function tests and gut inflammation in patients with primary sclerosing cholangitis and ileal pouch–anal anastomosis. J. Crohns Colitis http://dx.doi.org/10.1016/j.crohns.2011.10.011.
McLaughlin, S. D. et al. Extended spectrum β-lactamase-producing bacteria and Clostridium difficile in patients with pouchitis. Aliment. Pharmacol. Ther. 32, 664–669 (2010).
Shen, B. et al. Maintenance therapy with a probiotic in antibiotic-dependent pouchitis: experience in clinical practice. Aliment. Pharmacol. Ther. 22, 721–728 (2005).
McLaughlin, S. D. et al. VSL#3 for chronic pouchitis: experience in UK clinical practice [abstract W1767]. Gastroenterology 134 (Suppl. 1), A711 (2008).
Gionchetti, P. et al. Antibiotic combination therapy in patients with chronic treatment-resistant pouchitis. Aliment. Pharmacol. Ther. 13, 713–718 (1999).
Abdelrazeq, A. S., Kelly, S. M., Lund, J. N. & Leveson, S. H. Rifaximin–ciprofloxacin combination therapy is effective in chronic active refractory pouchitis. Colorectal Dis. 7, 182–186 (2005).
Mimura, T. et al. Four-week open-label trial of metronidazole and ciprofloxacin for the treatment of recurrent or refractory pouchitis. Aliment. Pharmacol. Ther. 16, 909–917 (2002).
Shen, B. et al. Combined ciprofloxacin and tinidazole in the treatment of chronic refractory pouchitis. Dis. Colon Rectum 50, 498–508 (2007).
Acosta, M. B. et al. Efficacy of infliximab rescue therapy in patients with chronic refractory pouchitis: a multicenter study. Inflamm. Bowel Dis. http://dx.doi.org/10.1002/ibd.21821.
Shen, B., Remzi, F. H., Lopez, A. R. & Queener, E. Rifaximin for maintenance therapy in antibiotic-dependent pouchitis. BMC Gastroenterol. 8, 26 (2008).
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author has acted as a consultant for Gi Health Education Foundation, Optimer and Prometheus Laboratories, and has received honoraria from Abbott, Axcan and UCB.
Rights and permissions
About this article
Cite this article
Shen, B. Acute and chronic pouchitis—pathogenesis, diagnosis and treatment. Nat Rev Gastroenterol Hepatol 9, 323–333 (2012). https://doi.org/10.1038/nrgastro.2012.58
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2012.58
This article is cited by
-
Dynamic ileal pouch emptying studies
Abdominal Radiology (2023)
-
Colectomy risk score predicts pouchitis in patients with ulcerative colitis
Updates in Surgery (2022)
-
Prediction of pouchitis after ileal pouch–anal anastomosis in patients with ulcerative colitis using artificial intelligence and deep learning
Techniques in Coloproctology (2022)
-
A New Rat Model of Pouchitis After Proctocolectomy and Ileal Pouch-Anal Anastomosis Using 2,4,6-Trinitrobenzene Sulfonic Acid
Journal of Gastrointestinal Surgery (2021)
-
Clinical Discrimination of Chronic Pouchitis After Ileal Pouch-Anal Anastomosis in Patients with Ulcerative Colitis
Journal of Gastrointestinal Surgery (2021)