Key Points
-
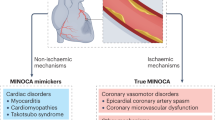
Coronary microvascular dysfunction (CMD) can present as chest pain with electrocardiographic changes and/or imaging abnormalities on stress testing, but no or nonobstructive coronary artery disease on angiography
-
CMD is an under-recognized and underdiagnosed condition that is associated with an increased incidence of adverse cardiac events
-
Risk factors for CMD seem to be similar to those for coronary artery disease, including hypertension, hyperlipidaemia, oestrogen deficiency in women, hyperglycaemia, chronic inflammation, and ageing; however, these factors do not fully account for the prevalence of CMD
-
CMD can be diagnosed using invasive angiography techniques, and novel noninvasive techniques (such as PET, transthoracic Doppler echocardiography, and cardiac MRI) are increasingly available
-
Supported by data from intermediate-outcome trials, treatment for CMD includes antiatherosclerotic and antianginal therapy, but trials to assess major adverse outcomes (such as death and myocardial infarction) are necessary
-
Most studies of CMD have focused on women; further evaluation is needed in men
Abstract
Cardiovascular disease is the leading cause of death worldwide. In the presence of signs and symptoms of myocardial ischaemia, women are more likely than men to have no obstructive coronary artery disease (CAD). Women have a greater burden of symptoms than men, and are often falsely reassured despite the presence of ischaemic heart disease because of a lack of obstructive CAD. Coronary microvascular dysfunction should be considered as an aetiology for ischaemic heart disease with signs and symptoms of myocardial ischaemia, but no obstructive CAD. Coronary microvascular dysfunction is defined as impaired coronary flow reserve owing to functional and/or structural abnormalities of the microcirculation, and is associated with an adverse cardiovascular prognosis. Therapeutic lifestyle changes as well as antiatherosclerotic and antianginal medications might be beneficial, but clinical outcome trials are needed to guide treatment. In this Review, we discuss the prevalence, presentation, diagnosis, and treatment of coronary microvascular dysfunction, with a particular emphasis on ischaemic heart disease in women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Fihn, S. D. et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 130, 1749–1767 (2014).
Montalescot, G. et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur. Heart J. 34, 2949–3003 (2013).
Banks, K., Lo, M. & Khera, A. Angina in women without obstructive coronary artery disease. Curr. Cardiol. Rev. 6, 71–81 (2010).
Sullivan, A. Chest pain in women: clinical, investigative & prognostic features. BMJ 308, 4 (1994).
Shaw, L. J. et al. Insights from the NHLBI-sponsored Women's Ischemia Syndrome Evaluation (WISE) study: part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J. Am. Coll. Cardiol. 47 (Suppl.), S4–S20 (2006).
Bairey Merz, C. N. et al. Insights from the NHLBI-sponsored Women's Ischemia Syndrome Evaluation (WISE) study: part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J. Am. Coll. Cardiol. 47 (Suppl.), S21–S29 (2006).
Bugiardini, R. & Bairey Merz, C. N. Angina with “normal” coronary arteries: a challenging philosophy. JAMA 293, 477–484 (2005).
Gulati, M. et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the Women's Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch. Intern. Med. 169, 843–850 (2009).
Eastwood, J. A. et al. Anginal symptoms, coronary artery disease, and adverse outcomes in black and white women: the NHLBI-sponsored Women's Ischemia Syndrome Evaluation study. J. Womens Health 22 724–732 (2013).
Johnson, B. D. et al. Persistent chest pain predicts cardiovascular events in women without obstructive coronary artery disease: results from the NIH-NHLBI-sponsored Women's Ischaemia Syndrome Evaluation (WISE) study. Eur. Heart J. 27, 1408–1415 (2006).
Reis, S. E. et al. Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. Am. Heart J. 141, 735–741 (2001).
Kothawade, K. & Bairey Merz, C. N. Microvascular coronary dysfunction in women: pathophysiology, diagnosis, and management. Curr. Probl. Cardiol. 36, 27 (2011).
Sharaf, B. et al. Adverse outcomes among women presenting with signs and symptoms of ischemia and no obstructive coronary artery disease: findings from the National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE) angiographic core laboratory. Am. Heart J. 166, 134–141 (2013).
Sedlak, T. L. et al. Sex differences in clinical outcomes in patients with stable angina and no obstructive coronary artery disease. Am. Heart J. 166, 38–44 (2013).
Jespersen, L. et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur. Heart J. 33, 734–744 (2012).
Maddox, T. M. et al. Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA 312, 1754–1763 (2014).
Humphries, K. H., Pu, A., Gao, M., Carere, R. G. & Pilote, L. Angina with “normal” coronary arteries: sex differences in outcomes. Am. Heart J. 155, 375–381 (2008).
Jones, E., Eteiba, W. & Bairey Merz, N. Cardiac syndrome X and microvascular coronary dysfunction. Trends Cardiovasc. Med. 22, 161–168 (2012).
Murthy, V. L. et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation 129, 2518–2527 (2014).
Camici, P. G. & Crea, F. Coronary microvascular dysfunction. N. Engl. J. Med. 356, 830–840 (2007).
Arrebola-Moreno, A. L. et al. Coronary microvascular spasm triggers transient ischemic left ventricular diastolic abnormalities in patients with chest pain and angiographically normal coronary arteries. Atherosclerosis 236, 207–214 (2014).
Davis, K. B., Chaitman, B., Ryan, T., Bittner, V. & Kennedy, J. W. Comparison of 15-year survival for men and women after initial medical or surgical treatment for coronary artery disease: a CASS registry study. Coronary Artery Surgery Study. J. Am. Coll. Cardiol. 25, 1000–1009 (1995).
Shaw, L. J. et al. The economic burden of angina in women with suspected ischemic heart disease: results from the National Institutes of Health—National Heart, Lung, and Blood Institute—sponsored Women's Ischemia Syndrome Evaluation. Circulation 114, 894–904 (2006).
Shaw, L. J. et al. Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the American College of Cardiology-National Cardiovascular Data Registry. Circulation 117, 1787–1801 (2008).
Johnston, N., Schenck-Gustafsson, K. & Lagerqvist, B. Are we using cardiovascular medications and coronary angiography appropriately in men and women with chest pain? Eur. Heart J. 32, 1331–1336 (2011).
Pepine, C. J. et al. Some thoughts on the vasculopathy of women with ischemic heart disease. J. Am. Coll. Cardiol. 47 (Suppl.), S30–S35 (2006).
Erbel, R. et al. Value of intracoronary ultrasound and Doppler in the differentiation of angiographically normal coronary arteries: a prospective study in patients with angina pectoris. Eur. Heart J. 17, 880–889 (1996).
Mieres, J. H. et al. Signs and symptoms of suspected myocardial ischemia in women: results from the What is the Optimal Method for Ischemia Evaluation in WomeN? trial. J. Womens Health 20, 1261–1268 (2011).
Safdar, B. et al. Gender-specific research for emergency diagnosis and management of ischemic heart disease: proceedings from the 2014 Academic Emergency Medicine Consensus Conference Cardiovascular Research Workgroup. Acad. Emerg. Med. 21, 1350–1360 (2014).
Masseri, A., Crea, F., Kaski, J. C. & Crake, T. Mechanisms of angina pectoris in syndrome X. J. Am. Coll. Cardiol. 17, 499–506 (1991).
Herrmann, J., Kaski, J. C. & Lerman, A. Coronary microvascular dysfunction in the clinical setting: from mystery to reality. Eur. Heart J. 33, 2771–2783 (2012).
Eggers, K. M., Johnston, N., James, S., Lindahl, B. & Venge, P. Cardiac troponin I levels in patients with non-ST-elevation acute coronary syndrome-the importance of gender. Am. Heart J. 168, 317–324.e1 (2014).
Crea, F., Camici, P. G. & Bairey Merz, C. N. Coronary microvascular dysfunction: an update. Eur. Heart J. 1101–1111 (2013).
Wessel, T. R. et al. Coronary microvascular reactivity is only partially predicted by atherosclerosis risk factors or coronary artery disease in women evaluated for suspected ischemia: results from the NHLBI Women's Ischemia Syndrome Evaluation (WISE). Clin. Cardiol. 30, 69–74 (2007).
Suessenbacher, A. et al. Sex differences in independent factors associated with coronary artery disease. Wien. Klin. Wochenschr. 126, 718–726 (2014).
Huxley, R. R. & Woodward, M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet 378, 1297–1305 (2011).
Almdal, T., Scharling, H., Jensen, J. S. & Vestergaard, H. The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population-based study of 13,000 men and women with 20 years of follow-up. Arch. Intern. Med. 164, 1422–1426 (2004).
Moreau, P., d'Uscio, L. & Lüscher, T. F. Structure and reactivity of small arteries in aging. Cardiovasc. Res. 37, 247–253 (1998).
Michel, J. B. et al. Effect of chronic ANG 1-coverting enzyme inhibitors on aging processes. II. Large arteries. Am. J. Physiol. 267 (Pt 2), R124–R135 (1994).
Rizzoni, D. et al. Relationships between coronary flow vasodilator capacity and small artery remodelling in hypertensive patients. J. Hypertens. 21, 625–631 (2003).
Mundhenke, M., Schwartzkopff, B. & Strauer, B. E. Structural analysis of arteriolar and myocardial remodelling in the subendocardial region of patients with hypertensive heart disease and hypertrophic cardiomyopathy. Virchows Arch. 431, 265–273 (1997).
Agabiti-Rosel, E. Structural and functional changes of the microcirculation in hypertension: influence of pharmacological therapy. Drugs 63, 19–29 (2003).
Smith, S. M. et al. Cardiovascular and mortality risk of apparent resistant hypertension in women with suspected myocardial ischemia: a report from the NHLBI-sponsored WISE study. J. Am. Heart Assoc. 3, e000660 (2014).
Sucato, V. Evola, S., Novo, G. & Novo, S. Diagnosis of coronary microvascular dysfunction in diabetic patients with cardiac syndrome X: comparison by current methods [Italian]. Recenti Prog. Med. 104, 63–68 (2013).
Girach, A. & Vignati, L. Diabetic microvascular complications—can the presence of one predict the development of another? J. Diabetes Complications 20, 228–237 (2006).
Di Carli, M. F., Janisse, J., Grunberger, G. & Ager, J. Role of chronic hyperglycemia in the pathogenesis of coronary microvascular dysfunction in diabetes. J. Am. Coll. Cardiol. 41, 2387–2393 (2003).
Galderisi, M. et al. Coronary flow reserve in hypertensive patients with hypercholesterolemia and without coronary heart disease. Am. J. Hypertens. 20, 177–183 (2007).
Duvernoy, C. S. et al. Gender differences in myocardial blood flow dynamics: lipid profile and hemodynamic effects. J. Am. Coll. Cardiol. 33, 463–470 (1999).
Bonetti, P. O., Lerman, L. O. & Lerman, A. Endothelial dysfunction: a marker of atherosclerotic risk. Arterioscler. Thromb. Vasc. Biol. 23, 168–175 (2003).
Recio-Mayoral, A., Rimoldi, O. E., Camici, P. G. & Kaski, J. C. Inflammation and microvascular dysfunction in cardiac syndrome X patients without conventional risk factors for coronary artery disease. JACC Cardiovasc. Imaging 6, 660–667 (2013).
Lanza, G. A. et al. Assessment of systemic inflammation and infective pathogen burden in patients with cardiac syndrome X. Am. J. Cardiol. 94, 40–44 (2004).
Cosín-Sales, J., Pizzi, C., Brown, S. & Kaski, J. C. C-reactive protein, clinical presentation, and ischemic activity in patients with chest pain and normal coronary angiograms. J. Am. Coll. Cardiol. 41, 1468–1474 (2003).
Ishimori, M. et al. Myocardial ischemia in the absence of obstructive coronary artery disease in systemic lupus erythematosus. JACC Cardiovasc. Imaging 4, 27–33 (2011).
Caliskan, M. et al. Impaired coronary microvascular and left ventricular diastolic functions in patients with ankylosing spondylitis. Atherosclerosis 196, 306–312 (2008).
Reriani, M. et al. Microvascular endothelial dysfunction predicts the development of erectile dysfunction in men with coronary atherosclerosis without critical stenoses. Coron. Artery Dis. 25, 552–557 (2014).
Kaski, J. C. Cardiac syndrome X in women: the role of oestrogen deficiency. Heart 92 (Suppl. 3), iii5–iii9 (2006).
Rosano, G. M. et al. 17-beta-estradiol therapy lessens angina in postmenopausal women with syndrome X. J. Am. Coll. Cardiol. 28, 1500–1505 (1996).
Albertsson, P. A., Emanuelsson, H. & Milsom, I. Beneficial effect of treatment with transdermal estradiol-17-beta on exercise-induced angina and ST segment depression in syndrome X. Int. J. Cardiol. 54, 13–20 (1996).
Adamson, D. L., Webb, C. M. & Collins, P. Esterified estrogens combined with methyltestosterone improve emotional well-being in postmenopausal women with chest pain and normal coronary angiograms. Menopause 8, 233–238 (2001).
Mosca, L. et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation 123, 1243–1262 (2011).
Merz, C. N. et al. A randomized controlled trial of low-dose hormone therapy on myocardial ischemia in postmenopausal women with no obstructive coronary artery disease: results from the National Institutes of Health/National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE). Am. Heart J. 159, 987.e1–e7 (2010).
Lanza, G. A. & Crea, F. Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation 121, 2317–2325 (2010).
Mehta, P. K. et al. Ranolazine improves angina in women with evidence of myocardial ischemia but no obstructive coronary artery disease. JACC Cardiovasc. Imaging 4, 514–522 (2011).
Camici, P. G., d'Amati, G. & Rimoldi, O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat. Rev. Cardiol. 12, 48–62 (2015).
McArdle, B. et al. Cardiac PET: metabolic and functional imaging of the myocardium. Semin. Nucl. Med. 43, 434–448 (2013).
Gould, K. L. et al. Anatomic versus physiologic assessment of coronary artery disease: role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J. Am. Coll. Cardiol. 62, 1639–1653 (2013).
Valenta, I., Dilsizian, V., Quercioli, A., Ruddy, T. D. & Schindler, T. H. Quantitative PET/CT measures of myocardial flow reserve and atherosclerosis for cardiac risk assessment and predicting adverse patient outcomes. Curr. Cardiol. Rep. 15, 344 (2013).
Plank, F. et al. The diagnostic and prognostic value of coronary CT angiography in asymptomatic high-risk patients: a cohort study. Open Heart 1, e000096 (2014).
Hou, Z. H. et al. Prognostic value of coronary CT angiography and calcium score for major adverse cardiac events in outpatients. JACC Cardiovasc. Imaging 5, 990–999 (2012).
[No authors listed] Italian Society of Cardiovascular Echography (SIEC) Consensus Conference on the state of the art of contrast echocardiography. Ital. Heart J. 5, 309–334 (2004).
Pathan, F. & Marwick, T. H. Myocardial perfusion imaging using contrast echocardiography. Prog. Cardiovasc. Dis. http://dx.doi.org/10.1016/j.pcad.2015.03.005.
Bartel, T. et al. Noninvasive assessment of microvascular function in arterial hypertension by transthoracic Doppler harmonic echocardiography. J. Am. Coll. Cardiol. 39, 2012–2018 (2002).
Prescott, E. et al. Improving diagnosis and treatment of women with angina pectoris and microvascular disease: the iPOWER study design and rationale. Am. Heart J. 167, 452–458 (2014).
Caiati, C. et al. Validation of a new noninvasive method (contrast-enhanced transthoracic second harmonic echo Doppler) for the evaluation of coronary flow reserve: comparison with intracoronary Doppler flow wire. J. Am. Coll. Cardiol. 34, 1193–1200 (1999).
Meimoun, P. et al. Transthoracic coronary flow velocity reserve assessment: comparison between adenosine and dobutamine. J. Am. Soc. Echocardiogr. 19, 1220–1228 (2006).
Dimitrow, P. P. Transthoracic Doppler echocardiography—noninvasive diagnostic window for coronary flow reserve assessment. Cardiovasc. Ultrasound 1, 4 (2003).
Okayama, H. et al. Usefulness of an echo-contrast agent for assessment of coronary flow velocity and coronary flow velocity reserve in the left anterior descending coronary artery with transthoracic Doppler scan echocardiography. Am. Heart J. 143, 668–675 (2002).
Pizzuto, F. et al. Assessment of flow velocity reserve by transthoracic Doppler echocardiography and venous adenosine infusion before and after left anterior descending coronary artery stenting. J. Am. Coll. Cardiol. 38, 155–162 (2001).
Ueno, Y., Nakamura, Y., Takashima, H., Kinoshita, M. & Soma, A. Noninvasive assessment of coronary flow velocity and coronary flow velocity reserve in the right coronary artery by transthoracic Doppler echocardiography: comparison with intracoronary Doppler guidewire. J. Am. Soc. Echocardiogr. 15, 1074–1079 (2002).
Panting, J. R. et al. Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N. Engl. J. Med. 346, 1948–1953 (2002).
Shufelt, C. L. et al. Cardiac magnetic resonance imaging myocardial perfusion reserve index assessment in women with microvascular coronary dysfunction and reference controls. Cardiovasc. Diagn. Ther. 3, 153–160 (2013).
Doyle, M. et al. Prognostic value of global MR myocardial perfusion imaging in women with suspected myocardial ischemia and no obstructive coronary disease: results from the NHLBI-sponsored WISE (Women's Ischemia Syndrome Evaluation) study. JACC Cardiovasc. Imaging 3, 1030–1036 (2010).
Freed, B. H. et al. Prognostic value of normal regadenoson stress perfusion cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 15, 108 (2013).
Dez Prez, R. D. et al. Cost-effectiveness of myocardial perfusion imaging: a summary of the currently available literature. J. Nucl. Cardiol. 12, 750–759 (2005).
Mishra, J. P., Acio, E., Heo, J., Narula, J. & Iskandrian, A. E. Impact of stress single-photon emission computed tomography perfusion imaging on downstream resource utilization. Am. J. Cardiol. 83, 1401–1403 (1999).
McCrohon, J. A. et al. Adjunctive role of cardiovascular magnetic resonance in the assessment of patients with inferior attenuation on myocardial perfusion SPECT. J. Cardiovasc. Magn. Reson. 7, 377–382 (2005).
Wei, J. et al. Safety of coronary reactivity testing in women with no obstructive coronary artery disease: results from the NHLBI-sponsored WISE (Women's Ischemia Syndrome Evaluation) study. JACC Cardiovasc. Interv. 5, 646–653 (2012).
Prasad, A. et al. Abnormal coronary microvascular endothelial function in humans with asymptomatic left ventricular dysfunction. Am. Heart J. 146, 549–554 (2003).
Pepine, C. J. et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women's Ischemia Syndrome Evaluation) study. J. Am. Coll. Cardiol. 55, 2825–2832 (2010).
Suwaidi, J. A. et al. Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation 101, 948–954 (2000).
Kuruvilla, S. & Kramer, C. M. Coronary microvascular dysfunction in women: on overview of diagnostic strategies. Expert Rev. Cardiovasc. Ther. 11, 1515–1525 (2013).
Gibson, C. M. et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation 93, 879–888 (1996).
Manginas, A. et al. Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method. Am. J. Cardiol. 83, 1562–1565 (1999).
Petersen, J. W. et al. TIMI frame count and adverse events in women with no obstructive coronary disease: a pilot study from the NHLBI-sponsored Women's Ischemia Syndrome Evaluation (WISE). PLoS ONE 9, e96630 (2014).
Luo, C. et al. Thermodilution-derived coronary microvascular resistance and flow reserve in patients with cardiac syndrome X. Circ. Cardiovasc. Interv. 7, 43–48 (2014).
Fearon, W. F. et al. Comparison of coronary thermodilution and Doppler velocity for assessing coronary flow reserve. Circulation 108, 2198–2200 (2003).
von Mering, G. O. et al. Abnormal coronary vasomotion as a prognostic indicator of cardiovascular events in women: results from the National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE). Circulation 109, 722–725 (2004).
Schlächinger, V., Britten, M. B., Zeiher, A. M. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation 101, 1899–1906 (2000).
Taqueti, V. R. et al. Interaction of impaired coronary flow reserve and cardiomyocyte injury on adverse cardiovascular outcomes in patients without overt coronary artery disease. Circulation 131, 528–535 (2015).
Taqueti, V. R. et al. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 131, 19–27 (2015).
Demirkol, S. et al. Association between microvascular angina and erectile dysfunction. Int. J. Impot. Res. 26, 124–127 (2014).
Strain, W. D. et al. Attenuated systemic microvascular function in men with coronary artery disease is associated with angina but not explained by atherosclerosis. Microcirculation 20, 670–677 (2013).
Murthy, V. L. et al. Coronary vascular dysfunction and prognosis in patients with chronic kidney disease. JACC Cardiovasc. Imaging 5, 1025–1034 (2012).
Nakanishi, K. et al. Prognostic values of coronary flow reserve in long-term cardiovascular outcomes in patients with chronic kidney disease. Am. J. Cardiol. 112, 928–932 (2013).
Shaw, L. J., Bugiardini, R. & Merz, C. N. Women and ischemic heart disease: evolving knowledge. J. Am. Coll. Cardiol. 54, 1561–1575 (2009).
Khuddus, M. A. et al. An intravascular ultrasound analysis in women experiencing chest pain in the absence of obstructive coronary artery disease: a substudy from the National Heart, Lung and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation (WISE). J. Interv. Cardiol. 23, 511–519 (2010).
Martino, S., Disch, D., Dowsett, S. A., Keech, C. A. & Mershon, J. L. Safety assessment of raloxifene over eight years in a clinical trial setting. Curr. Med. Res. Opin. 21, 1441–1452 (2005).
Barrett-Connor, E. et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N. Engl. J. Med. 355, 125–137 (2006).
Anand, S. S. et al. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. Eur. Heart J. 29, 932–940 (2008).
Stampfer, M. J., Hu, F. B., Manson, J. E., Rimm, E. B. & Willett, W. C. Primary prevention of coronary heart disease in women through diet and lifestyle. N. Engl. J. Med. 343, 16–22 (2000).
Samin, A., Nugent, L., Mehta, P. K., Shufelt, C. & Bairey Merz, C. N. Treatment of angina and coronary microvascular dysfunction. Curr. Treat. Options in Cardiovasc. Med. 12, 355–364 (2010).
Stone, N. J. et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129 (Suppl. 2), S1–S45 (2014).
Reriani, M. K. et al. Effects of statins on coronary and peripheral endothelial function in humans: a systematic review and meta-analysis of randomized controlled trials. Eur. J. Cardiovasc. Prev. Rehabil. 18, 704–716 (2011).
Treasure, C. B. et al. Beneficial effects of cholesterol-lowering therapy on the coronary endothelium in patients with coronary artery disease. N. Engl. J. Med. 332, 481–487 (1995).
Ridker, P. M., MacFadyen, J., Libby, P. & Glynn, R. J. Relation of baseline high-sensitivity C-reactive protein level to cardiovascular outcomes with rosuvastatin in the Justification for Use of statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER). Am. J. Cardiol. 106, 204–209 (2010).
Shahin, Y., Khan, J. A., Samuel, N. & Chetter, I. Angiotensin converting enzyme inhibitors effect on endothelial dysfunction: a meta-analysis of randomised controlled trials. Atherosclerosis 216, 7–16 (2011).
Pauly, D. F. et al. In women with symptoms of cardiac ischemia, nonobstructive coronary arteries, and microvascular dysfunction, angiotensin-converting enzyme inhibition is associated with improved microvascular function: a double-blind randomized study from the National Heart, Lung and Blood Institute Women's Ischemia Syndrome Evaluation (WISE). Am. Heart J. 162, 678–684 (2011).
Bavry, A. A. et al. Aldosterone inhibition and coronary endothelial function in women without obstructive coronary artery disease: an ancillary study of the NHLBI-sponsored Women's Ischemia Syndrome Evaluation (WISE). Am. Heart J. 167, 826–832 (2014).
Garg, R. et al. Mineralocorticoid receptor blockade improves coronary microvascular function in individuals with type 2 diabetes. Diabetes 64, 236–242 (2015).
Fraker, T. D. Jr et al. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. J. Am. Coll. Cardiol. 50, 2264–2274 (2007).
Heidenreich, P. A. et al. Meta-analysis of trials comparing beta-blockers, calcium antagonists, and nitrates for stable angina. JAMA 281, 1927–1936 (1999).
Bugiardini, R., Borghi, A., Biagetti, L. & Puddu, P. Comparison of verapamil versus propranolol therapy in syndrome X. Am. J. Cardiol. 63, 286–290 (1989).
Lanza, G. A., Colonna, G., Pasceri, V. & Maseri, A. Atenolol versus amlodipine versus isosorbide-5-mononitrate on anginal symptoms in syndrome X. Am. J. Cardiol. 84, 854–856 (1999).
Kayaalti, F. et al. Effects of nebivolol therapy on endothelial functions in cardiac syndrome X. Heart Vessels 25, 92–96 (2010).
Togni, M. et al. Does the beta-blocker nebivolol increase coronary flow reserve? Cardiovasc. Drugs Ther. 21, 99–108 (2007).
Cannon, R. O. 3rd, Watson, R. M., Rosing, D. R. & Epstein, S. E. Efficacy of calcium channel blocker therapy for angina pectoris resulting from small-vessel coronary artery disease and abnormal vasodilator reserve. Am. J. Cardiol. 56, 242–246 (1985).
Thadani, U. Current medical management of chronic stable angina. J. Cardiovasc. Pharmacol. Ther. 9 (Suppl. 1), S11–S29 (2004).
Opie, L. H. Calcium channel antagonists in the management of anginal syndromes: changing concepts in relation to the role of coronary vasospasm. Prog. Cardiovasc. Dis. 38, 291–314 (1996).
Timmis, A. D., Chaitman, B. R. & Crager, M. Effects of ranolazine on exercise tolerance and HbA1c in patients with chronic angina and diabetes. Eur. Heart J. 27, 42–48 (2006).
Chaitman, B. R. et al. Effects of ranolazine with atenolol, amlodipine, or diltiazem on exercise tolerance and angina frequency in patients with severe chronic angina: a randomized controlled trial. JAMA 291, 309–316 (2004).
Chaitman, B. R. et al. Anti-ischemic effects and long-term survival during ranolazine monotherapy in patients with chronic severe angina. J. Am. Coll. Cardiol. 43, 1375–1382 (2004).
Belardinelli, L., Shryock, J. C. & Fraser, H. Inhibition of the late sodium current as a potential cardioprotective principle: effects of the late sodium current inhibitor ranolazine. Heart 92 (Suppl. 4), iv6–iv14 (2006).
Hemingway, H. et al. Incidence and prognostic implications of stable angina pectoris among women and men. JAMA 295, 1404–1411 (2006).
Holubkoy, R. et al. Angina 1 year after percutaneous coronary intervention: a report from the NHLBI Dynamic Registry. Am. Heart J. 144, 826–833 (2002).
Johnson, B. D. et al. Prognosis in women with myocardial ischemia in the absence of obstructive coronary artery disease: results from the National Institutes of Health-National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE). Circulation 109, 2993–2999 (2004).
Pepine, C. J. Ischemic heart disease in women: facts and wishful thinking. J. Am. Coll. Cardiol. 43, 1727–1730 (2004).
Pepine, C. J. Ischemic heart disease in women. J. Am. Coll. Cardiol. 47 (Suppl.), S1–S3 (2006).
Wenger, N. K., Chaitman, B. & Vetrovec, G. W. Gender comparison of efficacy and safety of ranolazine for chronic angina pectoris in four randomized clinical trials. Am. J. Cardiol. 99, 11–18 (2007).
Skalidis, E. I., Hamilos, M. I., Chlouverakis, G., Zacharis, E. A. & Vardas, P. E. Ivabradine improves coronary flow reserve in patients with stable coronary artery disease. Atherosclerosis 215, 160–165 (2011).
Villano, A. et al. Effects of ivabradine and ranolazine in patients with microvascular angina pectoris. Am. J. Cardiol. 112, 8–13 (2013).
Emdin, M, Picano, E., Lattanzi, F. & L'Abbate, A. Improved exercise capacity with acute aminophylline administration in patients with syndrome X. J. Am. Coll. Cardiol. 14, 1450–1453 (1989).
Chen, J. W., Hsu, N. W., Wu, T. C., Lin, S. J. & Chang, M. S. Long-term angiotensin-converting enzyme inhibition reduces plasma asymmetric dimethylarginine and improves endothelial nitric oxide bioavailability and coronary microvascular function in patients with syndrome X. Am. J. Cardiol. 90, 974–982 (2002).
Bøtker, H. E., Sonne, H. S., Schmitz, O. & Nielsen, T. T. Effects of doxazosin on exercise-induced angina pectoris, ST-segment depression, and insulin sensitivity in patients with syndrome X. Am. J. Cardiol. 82, 1352–1356 (1998).
Chen, J. W. et al. Effects of short-term treatment of nicorandil on exercise-induced myocardial ischemia and abnormal cardiac autonomic activity in microvascular angina. Am. J. Cardiol. 80, 32–38 (1997).
Vicari, R. M. et al. Efficacy and safety of fasudil in patients with stable angina: a double-blind, placebo-controlled, phase 2 trial. J. Am. Coll. Cardiol. 46, 1803–1811 (2005).
Denardo, S. J. et al. Effect of phosphodiesterase type 5 inhibition on microvascular coronary dysfunction in women: a Women's Ischemia Syndrome Evaluation (WISE) ancillary study. Clin. Cardiol. 34, 483–487 (2011).
Maddox, T. M. et al. Utilization of secondary prevention therapies in patients with nonobstructive coronary artery disease identified during cardiac catheterization: insights from the National Cardiovascular Data Registry Cath-PCI Registry. Circ. Cardiovasc. Qual. Outcomes 3, 632–641 (2010).
Kronhaus, K. D. & Lawson, W. E. Enhanced external counterpulsation is an effective treatment for syndrome X. Int. J. Cardiol. 135, 256–257 (2009).
Di Pede, F. et al. Immediate and long-term clinical outcome after spinal cord stimulation for refractory stable angina pectoris. Am. J. Cardiol. 91, 951–955 (2003).
van Peski-Oosterbaan, A. S. et al. Cognitive-behavioral therapy for noncardiac chest pain: a randomized trial. Am. J. Med. 106, 424–429 (1999).
Chauhan, A. et al. Effect of transcutaneous electrical nerve stimulation on coronary blood flow. Circulation 89, 694–702 (1994).
Lanza, G. A. et al. Effect of spinal cord stimulation on spontaneous and stress-induced angina and 'ischemic-like' ST-segment depression in patients with cardiac syndrome X. Eur. Heart J. 26, 983–989 (2005).
Anderson, J. L. et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 2002 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation 116, 148–304 (2007).
Asbury, E. A., Kanji, N., Ernst, E, Barbir, M. & Collins, P. Autogenic training to manage symptomology in women with chest pain and normal coronary arteries. Menopause 16, 60–65 (2009).
Acknowledgements
The authors were supported by funding from the National Heart, Lung, and Blood Institute, numbers N01-HV-68161, N01-HV-68162, N01-HV-68163, and N01-HV-68164; grants K23HL105787, U0164829, U01 HL649141, U01 HL649241, T32HL69751, R01 HL090957, and 1R03AG032631 from the National Institute on Aging; GCRC grant MO1-RR00425 from the National Center for Research Resources; and grants from the Gustavus and Louis Pfeiffer Research Foundation, Danville, NJ, USA; The Women's Guild of Cedars-Sinai Medical Center, Los Angeles, CA, USA; The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, PA, USA; QMED, Inc., Laurence Harbor, NJ, USA; the Edythe L. Broad Women's Heart Research Fellowship; the Barbra Streisand Women's Cardiovascular Research and Education Program; and the Linda Joy Pollin Women's Heart Health Program, Cedars-Sinai Medical Center, Los Angeles, CA, USA.
Author information
Authors and Affiliations
Contributions
All the authors researched data for the article, discussed its content, wrote the manuscript, and reviewed/edited it before submission.
Corresponding author
Ethics declarations
Competing interests
P.K.M. has received research support from General Electric and Gilead, and has given lectures for the Medical Education Speakers Network (paid to Cedars-Sinai Medical Center). C.N.B.M. has given Continuing Medical Education lectures for Allegheny General Hospital, AHA, Bryn Mawr, Duke University, Emory University, Garden State, Gilead (Grant Review Committee), Japanese Circulation Society, Kaiser Permanente, Mayo Foundation, Preventive Cardiovascular Nurses Association, Practice Point Communications, University of California San Francisco, and Vox Media (paid to Cedars-Sinai Medical Center). C.N.B.M. has also received honoraria and consulting fees from NIH-SEP (Grant Review Study Section), Research Triangle Institute International, University of New Mexico, and Victor Chang Cardiac Research Institute; and has received research support from the Clinical Translational Science Institute, Flight Attendant Medical Research Institute, Gilead, and NIH. J.D. and S.D.C. declare no competing interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Dean, J., Cruz, S., Mehta, P. et al. Coronary microvascular dysfunction: sex-specific risk, diagnosis, and therapy. Nat Rev Cardiol 12, 406–414 (2015). https://doi.org/10.1038/nrcardio.2015.72
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2015.72
This article is cited by
-
Ascending Aorta 4D Time to Peak Distention Sexual Dimorphism and Association with Coronary Plaque Burden Severity in Women
Journal of Cardiovascular Translational Research (2024)
-
The Importance of Integrated Regulation Mechanism of Coronary Microvascular Function for Maintaining the Stability of Coronary Microcirculation: An Easily Overlooked Perspective
Advances in Therapy (2023)
-
The impact of sex on blood pressure and anthropometry trajectories from early adulthood in a Nigerian population: insights into women’s cardiovascular disease risk across the lifespan
BMC Women's Health (2022)
-
CHA2DS2 VASc score and brachial artery flow-mediated dilation as predictors for no-reflow phenomenon in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention
The Egyptian Heart Journal (2022)
-
Global trends and frontiers in research on coronary microvascular dysfunction: a bibliometric analysis from 2002 to 2022
European Journal of Medical Research (2022)