Abstract
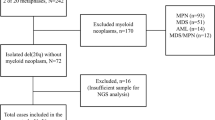
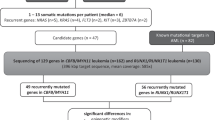
t(8;21)/RUNX1-RUNX1T1-positive acute myeloid leukemia (AML) is prognostically favorable; however, outcome is heterogeneous. We analyzed 139 patients with t(8;21)/RUNX1-RUNX1T1-positive AML (de novo: n=117; therapy-related: n=22) to determine frequency and prognostic impact of additional genetic abnormalities. All patients were investigated for mutations (mut) in ASXL1, FLT3, KIT, NPM1, MLL, IDH1, IDH2, KRAS, NRAS, CBL and JAK2. Sixty-nine of 139 cases (49.6%) had 1 mutation in addition to RUNX1-RUNX1T1, and 23/139 (16.5%) had ⩾2 additional mutations. Most common were KITmut (23/139; 16.5%), NRASmut (18/139; 12.9%) and ASXL1mut (16/139; 11.5%). FLT3-ITD, FLT3-TKDmut, CBLmut, KRASmut, IDH2mut and JAK2mut were found in 2.9–5.0%. Additional chromosomal abnormalities (ACAs) were found in 97/139 (69.8%). Two-year overall survival (OS) was 73.4% in 111 intensively treated patients. KITD816mut negatively impacted on OS in de novo AML (2-year OS: 59.1% vs 82.0%, P=0.03), ASXL1mut on EFS (de novo AML: 20% vs 59.1%, P=0.011; total cohort: 28.6% vs 56.7%, P=0.021). Sex chromosome loss was favorable (2-year EFS: 66.9% vs 43.0%, P=0.031), whereas +8 was adverse on EFS (2-year EFS: 26.7% vs 55.9%, P=0.02). In conclusion, t(8;21)/RUNX1-RUNX1T1-positive AML shows a high frequency of additional genetic alterations. Investigation for KITD816 and ASXL1mut combined with investigation of ACAs is recommended in t(8;21)/RUNX1-RUNX1T1-positive AML because of the prognostic significance of these parameters.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood 2010; 116: 354–365.
Mulloy JC, Cammenga J, MacKenzie KL, Berguido FJ, Moore MAS, Nimer SD . The AML1-ETO fusion protein promotes the expansion of human hematopoietic stem cells. Blood 2002; 99: 15–23.
Speck NA, Gilliland DG . Core-binding factors in haematopoiesis and leukaemia. Nat Rev Cancer 2002; 2: 502–513.
Kuchenbauer F, Schnittger S, Look T, Gilliland G, Tenen D, Haferlach T et al. Identification of additional cytogenetic and molecular genetic abnormalities in acute myeloid leukaemia with t(8;21)/AML1-ETO. Br J Haematol 2006; 134: 616–619.
Yuan Y, Zhou L, Miyamoto T, Iwasaki H, Harakawa N, Hetherington CJ et al. AML1-ETO expression is directly involved in the development of acute myeloid leukemia in the presence of additional mutations. Proc Natl Acad Sci USA 2001; 98: 10398–10403.
Higuchi M, O'Brien D, Kumaravelu P, Lenny N, Yeoh EJ, Downing JR . Expression of a conditional AML1-ETO oncogene bypasses embryonic lethality and establishes a murine model of human t(8;21) acute myeloid leukemia. Cancer Cell 2002; 1: 63–74.
Schnittger S, Schoch C, Dugas M, Kern W, Staib P, Wuchter C et al. Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease. Blood 2002; 100: 59–66.
Schessl C, Rawat VP, Cusan M, Deshpande A, Kohl TM, Rosten PM et al. The AML1-ETO fusion gene and the FLT3 length mutation collaborate in inducing acute leukemia in mice. J Clin Invest 2005; 115: 2159–2168.
Beghini A, Peterlongo P, Ripamonti CB, Larizza L, Cairoli R, Morra E et al. C-kit mutations in core binding factor leukemias. Blood 2000; 95: 726–727.
Wang YY, Zhou GB, Yin T, Chen B, Shi JY, Liang WX et al. AML1-ETO and C-KIT mutation/overexpression in t(8;21) leukemia: implication in stepwise leukemogenesis and response to Gleevec. Proc Natl Acad Sci USA 2005; 102: 1104–1109.
Schnittger S, Kohl TM, Haferlach T, Kern W, Hiddemann W, Spiekermann K et al. KIT-D816 mutations in AML1-ETO-positive AML are associated with impaired event-free and overall survival. Blood 2006; 107: 1791–1799.
Paschka P, Du J, Schlenk RF, Gaidzik VI, Bullinger L, Corbacioglu A et al. Secondary genetic lesions in acute myeloid leukemia with inv(16) or t(16;16): a study of the German–Austrian AML Study Group (AMLSG). Blood 2013; 121: 170–177.
Bowen DT, Frew ME, Hills R, Gale RE, Wheatley K, Groves MJ et al. RAS mutation in acute myeloid leukemia is associated with distinct cytogenetic subgroups but does not influence outcome in patients younger than 60 years. Blood 2005; 106: 2113–2119.
Kiyoi H, Naoe T, Nakano Y, Yokota S, Minami S, Miyawaki S et al. Prognostic implication of FLT3 and N-RAS gene mutations in acute myeloid leukemia. Blood 1999; 93: 3074–3080.
Boissel N, Leroy H, Brethon B, Philippe N, de Botton S, Auvrignon A et al. Incidence and prognostic impact of c-Kit, FLT3, and Ras gene mutations in core binding factor acute myeloid leukemia (CBF-AML). Leukemia 2006; 20: 965–970.
Schlenk R Dasatinib (Sprycel™) in patients with newly diagnosed core binding factor (CBF) acute myeloid leukemia (AML). ClinicalTrials gov 2013; NCT00850382.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al. Proposals for the classification of the acute leukaemias. French-American-British (FAB) co-operative group. Br J Haematol 1976; 33: 451–458.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al. Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med 1985; 103: 620–625.
Buchner T, Berdel WE, Schoch C, Haferlach T, Serve HL, Kienast J et al. Double induction containing either two courses or one course of high-dose cytarabine plus mitoxantrone and postremission therapy by either autologous stem-cell transplantation or by prolonged maintenance for acute myeloid leukemia. J Clin Oncol 2006; 24: 2480–2489.
Büchner T, Schlenk RF, Schaich M, Dohner K, Krahl R, Krauter J et al. Acute myeloid leukemia (AML): different treatment strategies versus a common standard arm—combined prospective analysis by the German AML Intergroup. J Clin Oncol 2012; 30: 3604–3610.
Arber DA, Brunning RD, Le Beau MM, Falini B, Vardiman J, Porwit A et al. Acute myeloid leukemia with recurrent genetic abnormalities. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H et al. (eds). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. International Agency for Research on Cancer (IARC): Lyon, France, 2008; pp 110–123.
Schoch C, Schnittger S, Bursch S, Gerstner D, Hochhaus A, Berger U et al. Comparison of chromosome banding analysis, interphase- and hypermetaphase-FISH, qualitative and quantitative PCR for diagnosis and for follow-up in chronic myeloid leukemia: a study on 350 cases. Leukemia 2002; 16: 53–59.
Haferlach C, Rieder H, Lillington DM, Dastugue N, Hagemeijer A, Harbott J et al. Proposals for standardized protocols for cytogenetic analyses of acute leukemias, chronic lymphocytic leukemia, chronic myeloid leukemia, chronic myeloproliferative disorders, and myelodysplastic syndromes. Genes Chromosomes Cancer 2007; 46: 494–499.
Shaffer LG, Tommerup N . ISCN 2013: An International System for Human Cytogenetic Nomenclature. Karger: Basel, Switzerland and New York, NY, USA, 2013.
Kern W, Voskova D, Schoch C, Hiddemann W, Schnittger S, Haferlach T . Determination of relapse risk based on assessment of minimal residual disease during complete remission by multiparameter flow cytometry in unselected patients with acute myeloid leukemia. Blood 2004; 104: 3078–3085.
Kern W, Bacher U, Haferlach C, Schnittger S, Haferlach T . The role of multiparameter flow cytometry for disease monitoring in AML. Best Pract Res Clin Haematol 2010; 23: 379–390.
Schnittger S, Weisser M, Schoch C, Hiddemann W, Haferlach T, Kern W . New score predicting for prognosis in PML-RARA+, AML1-ETO+, or CBFBMYH11+ acute myeloid leukemia based on quantification of fusion transcripts. Blood 2003; 102: 2746–2755.
Schnittger S, Eder C, Jeromin S, Alpermann T, Fasan A, Grossmann V et al. ASXL1 exon 12 mutations are frequent in AML with intermediate risk karyotype and are independently associated with an adverse outcome. Leukemia 2013; 27: 82–91.
Bacher U, Haferlach C, Kern W, Haferlach T, Schnittger S . Prognostic relevance of FLT3-TKD mutations in AML: the combination matters—an analysis of 3082 patients. Blood 2008; 111: 2527–2537.
Kohl TM, Schnittger S, Ellwart JW, Hiddemann W, Spiekermann K . KIT exon 8 mutations associated with core-binding factor (CBF)-acute myeloid leukemia (AML) cause hyperactivation of the receptor in response to stem cell factor. Blood 2005; 105: 3319–3321.
Schnittger S, Kern W, Tschulik C, Weiss T, Dicker F, Falini B et al. Minimal residual disease levels assessed by NPM1 mutation-specific RQ-PCR provide important prognostic information in AML. Blood 2009; 114: 2220–2231.
Schnittger S, Schoch C, Kern W, Mecucci C, Tschulik C, Martelli MF et al. Nucleophosmin gene mutations are predictors of favorable prognosis in acute myelogenous leukemia with a normal karyotype. Blood 2005; 106: 3733–3739.
Weisser M, Kern W, Schoch C, Hiddemann W, Haferlach T, Schnittger S . Risk assessment by monitoring expression levels of partial tandem duplications in the MLL gene in acute myeloid leukemia during therapy. Haematologica 2005; 90: 881–889.
Schnittger S, Haferlach C, Ulke M, Alpermann T, Kern W, Haferlach T . IDH1 mutations are detected in 6.6% of 1414 AML patients and are associated with intermediate risk karyotype and unfavorable prognosis in adults younger than 60 years and unmutated NPM1 status. Blood 2010; 116: 5486–5496.
Bacher U, Haferlach T, Schoch C, Kern W, Schnittger S . Implications of NRAS mutations in AML: a study of 2502 patients. Blood 2006; 107: 3847–3853.
Schnittger S, Bacher U, Alpermann T, Reiter A, Ulke M, Dicker F et al. Use of CBL exon 8 and 9 mutations in diagnosis of myeloproliferative neoplasms and myelodysplastic/myeloproliferative disorders: an analysis of 636 cases. Haematologica 2012; 97: 1890–1894.
Schnittger S, Bacher U, Kern W, Schroder M, Haferlach T, Schoch C . Report on two novel nucleotide exchanges in the JAK2 pseudokinase domain: D620E and E627E. Leukemia 2006; 20: 2195–2197.
Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH et al. Revised recommendations of the international working group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol 2003; 21: 4642–4649.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues 4th edn. International Agency for Research on Cancer (IARC): Lyon, France, 2008.
Wang YY, Zhao LJ, Wu CF, Liu P, Shi L, Liang Y et al. C-KIT mutation cooperates with full-length AML1-ETO to induce acute myeloid leukemia in mice. Proc Natl Acad Sci USA 2011; 108: 2450–2455.
Paschka P, Marcucci G, Ruppert AS, Mrozek K, Chen H, Kittles RA et al. Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B Study. J Clin Oncol 2006; 24: 3904–3911.
Kim HJ, Ahn HK, Jung CW, Moon JH, Park CH, Lee KO et al. KIT D816 mutation associates with adverse outcomes in core binding factor acute myeloid leukemia, especially in the subgroup with RUNX1/RUNX1T1 rearrangement. Ann Hematol 2013; 92: 163–171.
Schlenk RF, Benner A, Krauter J, Buchner T, Sauerland C, Ehninger G et al. Individual patient data-based meta-analysis of patients aged 16 to 60 years with core binding factor acute myeloid leukemia: a survey of the German Acute Myeloid Leukemia Intergroup. J Clin Oncol 2004; 22: 3741–3750.
Gustafson SA, Lin P, Chen SS, Chen L, Abruzzo LV, Luthra R et al. Therapy-related acute myeloid leukemia with t(8;21) (q22;q22) shares many features with de novo acute myeloid leukemia with t(8;21)(q22;q22) but does not have a favorable outcome. Am J Clin Pathol 2009; 131: 647–655.
Kayser S, Dohner K, Krauter J, Kohne CH, Horst HA, Held G et al. The impact of therapy-related acute myeloid leukemia (AML) on outcome in 2853 adult patients with newly diagnosed AML. Blood 2011; 117: 2137–2145.
Burnett AK, Wheatley K, Goldstone AH, Stevens RF, Hann IM, Rees JH et al. The value of allogeneic bone marrow transplant in patients with acute myeloid leukaemia at differing risk of relapse: results of the UK MRC AML 10 trial. Br J Haematol 2002; 118: 385–400.
Suciu S, Mandelli F, de Witte T, Zittoun R, Gallo E, Labar B et al. Allogeneic compared with autologous stem cell transplantation in the treatment of patients younger than 46 years with acute myeloid leukemia (AML) in first complete remission (CR1): an intention-to-treat analysis of the EORTC/GIMEMAAML-10 trial. Blood 2003; 102: 1232–1240.
Nguyen S, Leblanc T, Fenaux P, Witz F, Blaise D, Pigneux A et al. A white blood cell index as the main prognostic factor in t(8;21) acute myeloid leukemia (AML): a survey of 161 cases from the French AML Intergroup. Blood 2002; 99: 3517–3523.
Delaunay J, Vey N, Leblanc T, Fenaux P, Rigal-Huguet F, Witz F et al. Prognosis of inv(16)/t(16;16) acute myeloid leukemia (AML): a survey of 110 cases from the French AML Intergroup. Blood 2003; 102: 462–469.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
SS, WK, CH and TH are part owners of the MLL Munich Leukemia Laboratory GmbH. MTK, CE, TA, UB and NN are employed by the MLL Munich Leukemia Laboratory GmbH.
Additional information
Author contributions
SS and MTK were the principal investigators of this study, analyzed the data and wrote the manuscript. CE did analysis of molecular mutations. CH was responsible for chromosome banding analysis. WK was responsible for immunophenotyping and was involved in the statistical analysis. TH was responsible for cytomorphologic analysis, and MTK and UB contributed to cytomorphologic analysis. TA collected and analyzed clinical data. UB contributed writing of the manuscript. NN contributed to statistics and graphics. All authors read and contributed to the final version of the manuscript.
Rights and permissions
About this article
Cite this article
Krauth, MT., Eder, C., Alpermann, T. et al. High number of additional genetic lesions in acute myeloid leukemia with t(8;21)/RUNX1-RUNX1T1: frequency and impact on clinical outcome. Leukemia 28, 1449–1458 (2014). https://doi.org/10.1038/leu.2014.4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2014.4
Keywords
This article is cited by
-
Risk-directed therapy based on genetics and MRD improves the outcomes of AML1-ETO-positive AML patients, a multi-center prospective cohort study
Blood Cancer Journal (2023)
-
Cytogenetic evolution predicts a poor prognosis in acute myeloid leukemia patients who relapse after allogeneic hematopoietic stem cell transplantation
Annals of Hematology (2023)
-
ASXL1/2 mutations and myeloid malignancies
Journal of Hematology & Oncology (2022)
-
Non-age-related neoplastic loss of sex chromosome correlated with prolonged survival in real-world CBF-AML patients
International Journal of Hematology (2022)
-
Inhibition of CDK4/6 and autophagy synergistically induces apoptosis in t(8;21) acute myeloid leukemia cells
International Journal of Hematology (2021)