Abstract
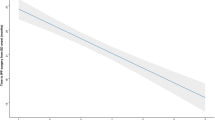
Oral PDE5 inhibitors, intracavernosal injection and penile implants are mainstay treatments for ED. Data on their utilization reflect economic aspects of ED, but are underreported. We report utilization data and user characteristics for these modalities in Taiwan between 1999 and 2011. Sales data on PDE5 inhibitors—sildenafil citrate, tadalafil and vardenafil and on alprostadil were retrieved from International Market Services Health, and on penile implants from the local importing company for them. Users’ clinical characteristics were derived from one institution. Between 1999 and 2011, sales of PDE5 inhibitors increased 5.9-fold, whereas those of alprostadil and penile implants remained stable. Over 90% of PDE5 inhibitors were purchased in pharmacies without a prescription. Between 1999 and 2011, the number of patients who received PDE5 inhibitors (n=4715) exceeded those who underwent penile injection (n=333) and penile implantation (n=108). The mean age of patients with ED who first received PDE5 inhibitors tended to decrease over consecutive years. Discontinuation of treatment with PDE5 inhibitors or intracavernosal injection reached 90% within 3 years of treatment initiation. Our data on the increasing market for PDE5 inhibitors and the trend for first use of PDE5 inhibitors at younger ages highlight the growing burden of ED and the acceptance of PDE5 inhibitors as the primary treatment for ED.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
National Institutes of Health. NIH consensus development panel on impotence. Impotence. JAMA 1993; 270: 83–90.
Lue TF, Giuliano F, Montorsi F, Rosen RC, Andersson KE, Althof S et al. Summary of the recommendations on sexual dysfunctions in men. J Sex Med 2004; 1: 6–23.
Wespes E, Amar E, Hatzichristou D, Hatzimouratidis K, Montorsi F, Pryor J et al. EAU Guidelines on erectile dysfunction: an update. Eur Urol 2006; 49: 806–815.
Moncada I, Martínez-Jabaloyas JM, Rodriguez-Vela L, Gutiérrez PR, Giuliano F, Koskimaki J et al. Emotional changes in men treated with sildenafil citrate for erectile dysfunction: a double-blind, placebo-controlled clinical trial. J Sex Med 2009; 6: 3469–3477.
Althof SE, Berner MM, Goldstein I, Claes HI, Cappelleri JC, Bushmakin AG et al. Interrelationship of sildenafil treatment effects on the physiological and psychosocial aspects of erectile dysfunction of mixed or organic etiology. J Sex Med 2010; 7: 3170–3178.
Chevret-Méasson M, Lavallée E, Troy S, Arnould B, Oudin S, Cuzin B . Improvement in quality of sexual life in female partners of men with erectile dysfunction treated with sildenafil: findings of the Index of Sexual Life (ISL) in a couple study. J Sex Med 2009; 6: 761–769.
Fisher WA, Rosen RC, Mollen M, Brock G, Karlin G, Pommerville P et al. Improving the sexual quality of life of couples affected by erectile dysfunction: a double-blind, randomized, placebo-controlled trial of vardenafil. J Sex Med 2005; 2: 699–708.
McCabe MP, O’Connor EJ, Conaglen JV, Conaglen HM . The impact of oral ED medication on female partners’ relationship satisfaction. J Sex Med 2011; 8: 479–483.
Wysowski DK, Swann J . Use of medications for erectile dysfunction in the United States, 1996 through 2001. J Urol 2003; 169: 1040–1042.
Jiann BP, Yu CC, Su CC . Impact of introduction of sildenafil on other treatment modalities for erectile dysfunction: a study of nationwide and local hospital. Int J Impot Res 2004; 16: 527–530.
Shabsigh R, Hackett G, Calomfirescu N, Kimoto Y, Meryn S, Torres LO . Economical Aspects of sexual dysfunctions. In Montorsi F, Basson R, Adaikan G, et al eds Sexual Medicine: Sexual Dysfunctions in Men and Women. Health Publication: Paris pp 205–228 2010.
Ayta IA, McKinlay JB, Krane RJ . The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int 1999; 84: 50–56.
Braun M, Wassmer G, Klotz T, Reifenrath B, Mathers M, Engelmann U . Epidemiology of erectile dysfunction: results of the ‘Cologne Male Survey’. Int J Impot Res 2000; 12: 305–311.
Kubin M, Wagner G, Fugl-Meyer AR . Epidemiology of erectile dysfunction. Int J Impot Res 2003; 15: 63–71.
Chew KK, Earle CM, Stuckey BG, Jamrozik K, Keogh EJ . Erectile dysfunction in general medicine practice: prevalence and clinical correlates. Int J Impot Res 2000; 12: 41–45.
Salonia A, Ferrari M, Saccà A, Pellucchi F, Castagna G, Clementi MC et al. Delay in seeking medical help in patients with new-onset erectile dysfunction remained high over and despite the PDE5 era-an ecological study. J Sex Med 2012; 9: 3239–3246.
Shabsigh R, Perelman MA, Laumann EO, Lockhart DC . Drivers and barriers to seeking treatment for erectile dysfunction: a comparison of six countries. BJU Int 2004; 94: 1055–1065.
Shabsigh R, Kaufman J, Magee M, Creanga D, Russell D, Budhwani M . Lack of awareness of erectile dysfunction in many men with risk factors for erectile dysfunction. BMC Urol 2010; 10: 18.
Scranton RE, Goldstein I, Stecher VJ . Erectile dysfunction diagnosis and treatment as a means to improve medication adherence and optimize comorbidity management. J Sex Med 2013; 10: 551–561.
Dyer K, das Nair R . Why don’t healthcare professionals talk about sex? A systemic review of recent qualitative studies conducted in the United Kingdom. J Sex Med 2013; 10: 2658–2670.
Delate T, Simmons VA, Motheral BR . Patterns of use of sildenafil among commercially insured adults in the United States: 1998–2002. Int J Impot Res 2004; 16: 313–318.
Capogrosso P, Colicchia M, Ventimiglia E, Castagna G, Clementi MC, Suardi N et al. One patient out of four with newly diagnosed erectile dysfunction is a young man-worrisome picture from the everyday clinical practice. J Sex Med 2013; 10: 1833–1841.
Feldman HA, Goldstein I, Hatichristou DG . Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol 1994; 151: 54–61.
Martins FG, Abdo CH . Erectile dysfunction and correlated factors in Brazilian men aged 18–40 years. J Sex Med 2010; 7: 2166–2173.
Bechara A, Casabé A, Bonis WD, Helien A, Bertolino MV . Recreational use of phosphodiesterase type 5 inhibitors by healthy young men. J Sex Med 2010; 7: 3736–3742.
Banks I . No man’s land: men, illness, and the NHS. BMJ 2001; 323: 1058–1060.
Schnetzler G, Banks I, Kirby M, Zou KH, Symonds T . Characteristics, behaviors, and attitudes of men bypassing the health care system when obtaining phosphodiesterase type 5 inhibitors. J Sex Med 2010; 7: 1237–1246.
Billups KL . Sexual dysfunction and cardiovascular disease: integrative concepts and strategies. Am J Cardiol 2005; 96: 57M–61M.
Inman BA, Sauver JL, Jacobson DJ, McGree ME, Nehra A, Lieber MM et al. A population-based, longitudinal study of erectile dysfunction and future coronary artery disease. Mayo Clin Proc 2009; 84: 108–113.
Jackson G, Arver S, Banks I, Stecher VJ . Counterfeit phosphodiesterase type 5 inhibitors pose significant safety risks. Int J Clin Pract 2010; 64: 497–504.
Jack A . Counterfeit medicines. Bitter pills. BMJ 2007; 335: 1120–1121.
Campbell N, Clark JP, Stecher VJ, Goldstein I . Internet-ordered Viagra (sildenafil citrate) is rarely genuine. J Sex Med 2012; 9: 2943–2951.
Kao SL, Chan CL, Tan B, Lim CC, Dalan R, Gardner D et al. An unusual outbreak of hypoglycemia. N Engl J Med 2009; 360: 734–736.
Jiann BP, Yu CC, Su CC, Tsai JY . Compliance of sildenafil treatment for erectile dysfunction and factors affecting it. Int J Impot Res 2006; 18: 146–149.
Sato Y, Tanda H, Kato S, Onishi S, Nitta T, Koroku M . How long do patients with erectile dysfunction continue to use sildenafil citrate? Dropout rate from treatment course as outcome in real life. Int J Urol 2007; 14: 339–342.
Klotz T, Mathers M, Klotz R, Sommer F . Why do patients with erectile dysfunction abandon effective therapy with sildenafil (Viagra®)? Int J Impot Res 2005; 17: 2–4.
Carvalheira AA, Pereira NM, Maroco J, Forjaz V . Dropout in the treatment of erectile dysfunction with PDE5: a study on predictors and a qualitative analysis of reasons for discontinuation. J Sex Med 2012; 9: 2361–2369.
Althof SE . When an erection alone is not enough: biopsychosocial obstacles to lovemaking. Int J Impot Res 2002; 14 (Suppl 1): S99–S104.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tsai, WK., Jiann, BP. Data on the utilization of treatment modalities for ED in Taiwan in the era of PDE5 inhibitors. Int J Impot Res 26, 141–145 (2014). https://doi.org/10.1038/ijir.2013.53
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2013.53
Keywords
This article is cited by
-
Pharmacological treatment and inappropriate prescriptions for patients with erectile dysfunction
International Journal of Clinical Pharmacy (2020)
-
Sildenafil citrate use in Addis Ababa: characteristics of users and pharmacists’ dispensing practices
International Journal of Clinical Pharmacy (2018)