Abstract
Methods employed for pulse wave analysis (PWA) and peripheral blood pressure (PBP) calibration vary. The purpose of this study was to evaluate the agreement of SphygmoCor PWA parameters derived from radial artery tonometry when considering (1) timing (before vs. after tonometry) and side selection (ipsilateral vs. contralateral limb) for PBP calibration and (2) side selection for tonometry (left vs. right arm). In 34 subjects (aged 21.9±2.3 years), bilateral radial artery tonometry was performed simultaneously on three instances. PBP assessment via oscillometric sphygmomanometry in the left arm only and both arms simultaneously occurred following the first and second instances of tonometry, respectively. Significant within arm differences in PWA parameters derived before and after PBP measurement were observed in the right arm only (for example, aortic systolic blood pressure, Δ=0.38±0.64 mm Hg). Simultaneously captured bilateral PWA variables demonstrated significant between arm differences in 88% (14/16) and 56% (9/16) of outcome variables when calibrated to within arm and equivalent PBP, respectively. Moreover, the right arm consistently demonstrated lower values for clinical PWA variables (for example, augmentation index, bias=−2.79%). However, 26% (n=9) of participants presented with clinically significant differences (>10 mm Hg) in bilateral PBP and their exclusion from analysis abolished most between arm differences observed. SphygmoCor PWA in the right radial artery results in greater variability independent of the timing of PBP measurement and magnitude of calibration pressures in young subjects. Moreover, bilateral PBP measurement is imperative to identify subjects in whom a significant difference in bilateral PWA outcomes may exist.
Similar content being viewed by others
Introduction
Several parameters of central arterial blood pressure and wave reflection characteristics have demonstrated value as independent predictors of future cardiovascular morbidity and mortality.1, 2, 3, 4, 5 Central blood pressures have also been shown to more strongly relate to vascular disease than peripheral blood pressures.4 However, direct measurement of central aortic pressures is invasive and expensive.6 As a result, methods for noninvasive assessment of central hemodynamic indices have been increasingly employed in clinical and research settings for evaluation and titration of treatments and/or interventions.
There are a number of methods currently available for the noninvasive assessment of aortic wave reflection characteristics.7, 8 At present, applanation tonometry in which high-fidelity radial artery pressure waveforms are recorded using a ‘pencil’ type micromanometer are most commonly performed,9 likely due in part to the strong validity and reliability of resultant measures reported in the literature.10, 11, 12 Notably, the central hemodynamic indices derived from radial artery pulse wave analysis (PWA) are dependent upon calibration to peripheral artery blood pressure (PBP) measured at the brachial artery and based on the assumption that mean blood pressure is constant throughout the arterial tree.13, 14 Further, the importance of PBP in PWA measures is emphasized by Shih et al.15 who demonstrated that errors in PWA measurements are equivalent to those associated with brachial cuff sphygmomanometry.
Methods for PBP determination and calibration vary between PWA devices and are not always standardized. In the case of the SphygmoCor system (AtCor Medical, Sydney, NSW, Australia), the operations manual recommends a rest period after brachial artery sphygmomanometry before radial pressure waveform measurement because of supra-systolic pressures followed by a period of cuff deflation which disrupts local and distal blood flow and brachial wave transmission. This would seem to suggest that PBP measurement should be performed in the same arm at which PWA will occur. However, to our knowledge, there is no data available that examines the variability in PWA at the radial artery prior to and following PBP assessment at the brachial artery via cuff sphygmomanometry.
To circumvent the disruption in arterial blood flow that may occur downstream of cuff sphygmomanometry, calibration could be performed by using measurement of PBP in the contralateral limb. However, PBP measurements made at the brachial artery have been shown to vary significantly between arms.16, 17 Given the reliance of PWA on PBP calibration, disparities in bilateral PBP could further increase variability in clinical measures derived from PWA depending on the arm selected for calibration. Indeed, calibration is based on the assumption that mean blood pressure is constant throughout the large arteries.14 Moreover, it is unknown if characteristics of the radial pulse pressure wave derived from PWA are also variable between arms of measure, independent of arm selection for calibration. Importantly, validation studies frequently use a single arm and/or exclude persons with unequal brachial pressures.11, 12, 18, 19 As PWA protocols are increasingly employed in clinical and research settings, it is imperative to explore potential differences in bilateral PWA and to standardize evaluation methods for continuity of patient monitoring and comparative value of PWA outcomes.
Therefore, the purpose of this study was to (1) evaluate the effect of PBP measurement on subsequent PWA, (2) evaluate the difference in PWA between arms when calibrated to the same PBP (for example, left brachial artery) and (3) evaluate the difference in PWA between arms when calibrated to within arm PBP in young, apparently healthy people using the SphygmoCor system.
Methods
Study participants.
The study population was recruited via word of mouth from the greater Hamden, CT, USA and Kingston, RI, USA areas with 34 subjects (17 male, 17 female; 21.9±2.3 years) enrolled. Apparently healthy, young (aged <30 years), nonsmokers without previously diagnosed cardiovascular disease were included in this study and all participants maintained normal sinus rhythm throughout the testing procedures. Subjects were asked to report to the laboratory in a post-absorptive state and were instructed to abstain from exercise and the consumption of alcohol and caffeine for at least 12 h prior to testing. A random number generator was used to create a list of 40, four digit codes that were assigned consecutively to each subject. All measurements were made in the Cardiovascular Laboratories at Quinnipiac University and the University of Rhode Island. This study was approved by the Institutional Review Boards at Quinnipiac University and the University of Rhode Island and written informed consent was obtained from all participants.
Subject characteristics
Height and weight were measured by using standard techniques. Body fat was assessed via bioelectrical impedance analysis (Omron HBF306C, Omron Corporation, Kyoto, Japan). Heart rate (HR) brachial systolic (PSBP), diastolic (PDBP) and pulse blood pressure (PPP) measurements were made in triplicate at the brachial artery of the right and left arms by oscillometric blood pressure sphygmomanometry by using an automated, noninvasive device (Omron BP785). The Omron BP785 (HEM-7222) has been declared as equivalent to the Omron M6 (HEM-7000) which has been previously validated according to the international protocol20 and is required by manufacturing standards to be accurate within 3 mm Hg for pressure readings. In our hands, for triplicate measurements at the same site, the overall intra-class correlation coefficient was 0.96 and 0.88 and the typical error was 3.27 and 2.54 for PSBP and PDBP, respectively. HR and PBP measurements were made on two occasions in the left arm, and on one occasion in the right arm with the second set of measures in the left arm and the singular set of measures in the right arm occurring simultaneously. Two automated oscillometric blood pressure sphygmomanometry devices (Omron BP785) were used throughout the study with the arm measured by each device randomly selected for each subject (that is, odd/even first digit of subject code). The average of three HR and BP measurements at each timepoint was used for resting values and hypertensive status was determined by the mean of all left arm PBP measurements, unless right arm PBP was found to be significantly higher (⩾10 mm Hg) than the left in which case the higher, right arm was used.21
Pulse wave analysis (PWA)
The assessment of arterial wave reflection characteristics was performed noninvasively using identical SphygmoCor CPVH Pulse Wave Velocity systems and Research Version 9.0 software (AtCor Medical, Sydney, NSW, Australia). The SphygmoCor systems utilize a Medical Electronics Module Model EM3, an AtCor Medical/Millar tipped pressure tonometer (Millar Instruments, Houston, TX, USA) and a validated generalized mathematical transfer function to synthesize a central aortic pressure waveform.13, 14 The generalized transfer function has been validated using both intra-arterially and noninvasively obtained radial pressure waves.12
Participants rested quietly in a supine position in a temperature controlled room for 15 min prior to initial radial artery pulse pressure waveform analysis. Consecutive pulse pressure waveform measurements were then performed by two highly trained and experienced technicians (JSM and DTB) simultaneously at the right and left radial artery on three occasions interspersed by PBP assessment in the left arm only and in both arms simultaneously (Supplementary Figure 1). Briefly, an initial set of pulse pressure waveform measurements was performed (PWA1), PBP was assessed in the left arm only, a second set of pulse pressure waveform measurements commenced (PWA2), PBP was assessed simultaneously in the right and left arms and, finally, a third set of pulse pressure waveform measurements was performed (PWA3). The arm evaluated for PWA by each of the two investigators was randomly selected for each subject (that is, odd/even last digit of subject code) and the average of the first three high-quality pulse pressure waveform recordings per subject and per tonometer were captured for analysis. Pulse pressure waveforms were calibrated to the ipsilateral and/or contralateral limb PSBP and PDBP as appropriate for the comparisons described below (see statistical analysis). The use of PSBP and PDBP to calibrate radial pressure waveforms omits a possible brachial-to-radial pressure amplification and may lead to underestimation of the central pressure.22, 23, 24, 25 Despite this, PSBP and PDBP were used for radial artery waveform calibration, as recommended by the manufacturer, as automated oscillometric blood pressure monitors are not required to verify and validate mean arterial pressur,26 available estimation equations will produce calibration errors,27 and the range of error in calibration was found to be less by Shih et al.15 when utilizing PSBP and PDBP rather than mean arterial pressure and PDBP.
Optimal recording of the pressure wave was obtained when the hold-down force of the transducer on the artery was such that the resulting waveform had a stable baseline for at least 10 cardiac cycles and resulted in a quality index of ⩾90% (derived from an algorithm including average pulse height variation, diastolic variation and maximum rate of rise of the peripheral waveform). This technique has been shown to be highly reproducible28 and, in our hands, reproducibility in young, healthy men has previously been reported with a mean coefficient of variation of 6.5, 2.1, 2.4 and 2.4% for aortic augmentation inde, time to reflection of the reflected pressure wave (T1r), central systolic and diastolic blood pressure, respectively.29
A typical aortic pressure waveform synthesized from radial pulse pressure using applanation tonometry and the generalized transfer function is shown in Supplementary Figure 2. Detailed description of PWA parameters have been described previously.30
Statistical analysis
Analyses included the following: (1) To evaluate the effect of PBP measurement on subsequent PWA, comparisons of dependent variables within arm and calibrated to within arm PBP (left arm: PWA1 vs. PWA2; right arm: PWA2 vs. PWA3) were performed; (2) to evaluate the difference between arms in PWA, comparisons of dependent variables between arms, calibrated to left arm PBP (PWA1 and PWA2) were performed; (3) to evaluate the effect of calibrating to within arm PBP on between arm differences in PWA, comparisons of dependent variables between arms, calibrated to within arm PBP (PWA3) were performed; (4) to explore the impact of clinically significant differences in bilateral PBP (defined as a difference >10 mm Hg) on the observed PWA differences between arms, comparisons of dependent variables at PWA2 when calibrated to the same (left arm) PBP were made when subjects were clustered as overall (overall group; n=34), those with (clinical difference, n=9) and those without (normal, n=25) a clinically significant difference in PBP; and (5) to determine the effect of not detecting a clinically significant difference in PBP between arms with PWA, comparisons of left arm PWA2 dependent variables in the clinically different group when calibrated to the lower (left arm) and higher (right arm) PBP observed were performed.
Nine subjects presented with a clinically significant difference in bilateral PBP with eight demonstrating the higher pressure in the right arm. The subject with clinically significant higher PBP in the left arm was excluded from analyses 4 and 5, described above, to more clearly define the directional error associated with the traditional method of assessing PBP and PWA in only the left arm. Inclusion/exclusion of this subject in the analysis did not affect any of the significant outcomes.
All values are presented as mean±s.d. Kolmogorov–Smirnov tests were used to confirm normality of the distributions of the variable differences. Comparisons of PWA primary and secondary variables measured in the left and right arms via pencil-type tonometer were analyzed using Student’s paired t-tests for within and between arms differences. In the sub-analysis of subjects with and without clinically significant difference in bilateral PBP, Satterwaite corrected two sample t-tests were performed. Linear regression by the method of ordinary least squares was used to define the correlation between tonometer values, with goodness of fit expressed by Pearson’s correlation coefficient (r). Further, agreement between the left and right arm measurements were analyzed using Bland–Altman tests for agreement of clinical measurements and defined as being within 10% of the overall mean for the studied variable as the maximal tolerated difference.31 An alpha level of P<0.05 was required for statistical significance. Based on the reproducibility of augmentation index measured by PWA by Wilkinson et al.,28 we determined that ~30 subjects would be required to give at least an 80% chance of detecting a difference in AIx of 10% at an alpha level of 0.05. All statistical analyses were performed by using SPSS version 22.0 for Windows (SPSS, Chicago, IL, USA).
Results
Subject characteristics are presented in Table 1. Study participants (n=34) included 22 normotensive, 11 prehypertensive and 1 stage 1 hypertensive participants. Overall means of PSBP, PDBP and PMAP were calculated as the average of simultaneous bilateral measurements resulting in PSBP, PDBP and PMAP means of 114.7±13.7 mm Hg, 65.6±7.0 mm Hg and 81.9±7.4, respectively. PSBP and PPP were significantly different in the right and left arms when simultaneously measured (P<0.01). No significant differences in PBP were found between time points in the left arm.
Effect of peripheral blood pressure measurement on subsequent pulse wave analysis variables
Comparisons of the within arm difference before and after calibration to PBP via cuff sphygmomanometry in PWA parameters are presented in Table 2. There were no significant differences identified within the left arm. However, HR, ASBP, APP, PPA, TTI and AIx@75 were significantly different following PBP measurement in the right arm (P<0.05 for HR, PPA and AIx@75; P<0.01 for ASBP, APP and TTI).
Evaluation of the difference in pulse wave analysis variables between arms
Comparisons of between arms measures derived simultaneously from PWA at the respective radial artery after calibration to the same PBP (that is, left arm) demonstrated significant differences in ED, AgBP, AgBP@75, ASBP, AMAP, APP, PPA, TTI, DTI, SEVR, AIx1, AIx2, AIx@75 and wasted left ventricular energy (LVEW) (Table 3). The most striking differences between arms were observed in AgBP, AIx1, AIx@75 and LVEW at 0.8 mm Hg, 2.8%, 2.7% and 79.26 dynes s cm−1, respectively. When comparing simultaneous measurements between arms before calibration to the same PBP, the same parameters were significantly different, with the exceptions of AMP, TTI and SEVR (P=0.298, 0.570 and 0.973, respectively; data not shown).
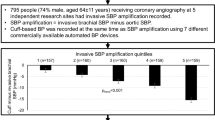
Figures 1 and 2 show Pearson correlations and Bland–Altman tests for agreement of clinical measurements. PWA measurements in the right arm produced a negative bias in SEVR, AgBP, AIx1, AIx2, AIx@75 and LVEW whereas DTI demonstrated a positive bias which was expected given its reciprocal relationship with TTI. In persons that presented with clinically different bilateral PBP, the difference between arms was significantly higher when compared with ‘normal’ subjects for AgBP, AgBP@75, TTI, DTI, SVI, AIx1, AIx2, AIx@75 and LVEW despite being calibrated to the same PBP. Moreover, in all cases except for DTI, the significant difference between arms in simultaneous PWA measurements was abolished when considering only the ‘normal’ subjects (Figure 3).
Correlation coefficients and Bland–Altman plots for right and left arm measurement agreement in PWA-derived measures of central augmented blood pressure (AgBP), the central augmentation index (AIx1) and wasted left ventricular energy (LVEw) at PWA2. Closed circles represent subjects who presented with a clinically significant difference in bilateral peripheral blood pressure (n=9), whereas open circles represent those without a clinically significant difference in peripheral blood pressure (n=25).
Correlation coefficients and Bland–Altman plots for right and left arm measurement agreement in PWA-derived measures of the tension-time index (TTI), diastolic-time index (DTI) and sub-endocardial viability ration (SEVR) at PWA2. Closed circles represent subjects who presented with a clinically significant difference in bilateral peripheral blood pressure (n=9), whereas open circles represent those without a clinically significant difference in peripheral blood pressure (n=25).
Between arm differences (right arm—left arm) in PWA-derived characteristics of central arterial blood pressure and wave reflection characteristics at PWA2. TTI, tension-time index; DTI, diastolic time index; SEVR, sub-endocardial viability ratio; AgBP, central augmented blood pressure AIx1, augmentation index 1, LVEW, wasted left ventricular energy. Data are mean±s.d. Paired t-tests were performed to determine significant differences between arms and Satterthwaite corrected two sample t-tests were performed to determine differences between groups. Clinically different bilateral blood pressure was defined as>10 mm Hg. *Significantly different between arms (P<0.05), †significantly different between groups (P<0.05).
Effect of calibration to within arm peripheral blood pressure on differences in between arm pulse wave analysis variables
Between arms measures derived simultaneously from PWA at the respective radial artery after calibration to within arm PBP are shown in Table 4. Simultaneous measurements calibrated to within arm PBP no longer demonstrated statistical differences in ASBP, AMAP, TTI, DTI and SEVR. Although the difference in ASBP increased (−0.4 vs. +1.96; PWA2 vs. PWA3) when calibrated to within arm PBP, it only approached statistical significance (P=0.065). Differences in ASBP, ED, AgBP, AgBP@75, APP, PPA, AIx1, AIx2, AIx@75 and LVEW between arms were still found to vary significantly between sides.
Effect of not detecting a clinically significant difference in bilateral peripheral blood pressure measurement on pulse wave analysis variables
Correcting for the higher PBP (recalibration) with the same radial artery pulse pressure waveform measurements in the clinically different group resulted in significant increases in TTI (182.5±73.4, P<0.01), DTI (246.0±149.5, P<0.01), CSP (10.8±3.5, P<0.01), CDP (4.1±4.3, P<0.05), CPP (6.7±4.6, P<0.01) and CMP (7.1±3.3, P<0.01).
Discussion
The present study sought to evaluate the agreement in variables derived from bilateral radial artery PWA and the effects of timing and side selection for PBP measurement using the SphygmoCor system. The principle findings are that, in young subjects (1) there was no significant effect of PBP measurement on repeated PWA in the left arm; (2) there is a significant difference in simultaneously captured bilateral PWA in which the right arm variables associated with wave reflection characteristics are lower; and (3) a significant portion of the negative bias in the right arm was associated with subjects who presented with clinically significant differences in PBP.
It has been suggested that peripheral vasodilation caused by arterial obstruction alters brachial wave transmission,32 and this may need to be considered in the assessment of PBP prior to PWA. Indeed, the SphygmoCor operator’s manual suggests that a period of at least 2 min elapse following cuff sphygmomanometry before radial pressure waveform recordings. However, to our knowledge, no data are available that documents the magnitude or time course of the effect(s) of PBP assessment via cuff sphygmomanometer on indices derived from PWA. Here we employed radial artery PWA before and two minutes after PBP measurement in the left arm and found no significant effect of standard brachial artery sphygmomanometry on any variables (P>0.10 for all dependent variables). Interestingly, significant differences were observed in ASBP, APP, PPA, TTI and AIx@75 measurements prior to and following PBP assessment in the right arm (Table 2). Although the absolute difference between measurements is modest, it does suggest a greater variability in the right arm with consecutive PWA measurements surrounding PBP assessment may exist. Indeed, greater variability in right arm PBP has been reported previously33 and may extend to differences in radial pressure waveforms.
Several investigations have reported differences in PBP between arms with ~20% exhibiting clinically significant bilateral differences (defined as a >10 mm Hg difference).17, 34 In the present study, we observed a significant difference in PSBP and PPP between arms (Table 1) and nine subjects (26.5%) presented with clinically significant differences between arms. Current recommendations for the assessment of PBP include measurement in both arms at first examination,21, 35, 36 and when a consistent inter-arm difference is observed that the higher pressure should be used to determine hypertensive status.21 Strict adherence to these guidelines is not routinely reported in PWA studies and clinical adherence is sub-optimal.37 Frequently, PWA and PBP are measured in the same arm (for example, left arm), and may not detect a difference in bilateral PBP. Of the 9 subjects in our study that presented with clinically significant differences in PBP, comparative analysis of the effect of calibration to each limb for the same radial artery PWA measurements demonstrated markedly lower values for clinically relevant variables, TTI (10%), DTI (8%), ASBP (11%), ADBP (6%), APP (24%) and AMAP (9%), when calibrated to the lower pressure. Given the clinical implications of these markers, this discrepancy cannot be ignored. For example, it has been reported that there is a 7 and 15% increase in cardiovascular risk for every 10 mm Hg increase in ASBP and APP, respectively.38 Importantly, 8 of 9 participants exhibited significantly higher PBP in the right arm.
Comparisons of simultaneous bilateral PWA parameters revealed significant differences between sides whether calibrated to the ipsilateral or contralateral limb. Nearly all (HR, T1r and ADBP being the exceptions) PWA variables were significantly different between arms when measured simultaneously and calibrated to the same (left arm) PBP with the right arm consistently indicating lesser results of wave reflection and central pressure augmentation (Table 3). Moreover, independent of PBP calibration, ED and PPA were consistently higher in the right arm while AgBP, AgBP@75, AIx1, AIx2, AIx@75 and LVEW were consistently lower in the right arm at all time points (Table 4). To further explore these differences, Pearson correlations and Bland–Altman agreement analyses were evaluated to demonstrate the bias between arms. Selected variables presented in Figures 1 and 2 illustrate the negative bias in parameters of wave reflection and central pressure augmentation. Despite modest bias in measures known to have a considerable variability (TTI, DTI and SEVR; Figure 2),39 underestimation in clinical populations (for example, coronary artery disease) is less than desirable. The present study included young, apparently healthy male and female participants representing a relatively homogenous population. Therefore, further studies should be conducted to evaluate the bilateral PWA relationship in aged and clinical populations as age associated increases in vascular resistance and/or asymmetrical vascular disease may contribute to disparities in PWA characteristics.17, 40 Nevertheless, as can be appreciated from Figure 1, there was a moderate negative bias associated with central pressure augmentation (that is, AgBP, AIx1) and resultant LVEW, an index of myocardial oxygen demand and LV work.41 In our study, six (18%) of the participants demonstrated absolute differences of greater than 10% for AIx and, on average, the bias for AIx was 3% lower in the right arm. The clinical significance of the observed difference is demonstrated by reports that the relative risk of LV hypertrophy, and independent predictor of cardiovascular events,42 has been reported as 1.99 for each 10% increase in AIx.43
Upon review of our data, we hypothesized that the bias in bilateral PWA assessment may be driven by those that presented with clinically significant differences in bilateral PBP. Identification of those subjects on the Pearson correlation and Bland–Altman agreement analyses plots (represented by closed circles, Figures 1 and 2) demonstrated a clear pattern of greater variability in those subjects. When grouped separately, the difference in bilateral PWA measures is amplified in those with a clinically significant difference in bilateral PBP and abolished in those without for all variables except DTI (Figure 3).
Limitations
The prevalence of clinically significant differences in bilateral blood pressure among young, apparently healthy, non-obese subjects in the present study was unexpected. Although inter-arm differences in PBP can suggest underlying pathophysiology (for example, vascular disease), Grossman et al.44 recently reported a prevalence of 13 and 9% for inter-arm systolic and diastolic blood pressures, respectively, in a large cohort of young, healthy subjects. Importantly, the prevalence was not related to age, body mass index or heart rate. In addition, the automated oscillometric blood pressure devices employed in the present study feature a calibration check system which runs immediately prior to each measurement, were used within 3 months of initial manufacturer calibration, and are similar to those commonly used in clinical and research settings. Ideally, aortic pressure waveforms should be measured directly via arterial angiography as a gold standard for reference. However, the purpose of the present study was to evaluate bilateral differences in variables derived from unilateral radial artery PWA methods that have previously been validated invasively. Regardless, further studies should be conducted to further explore the differences in bilateral PWA in a larger, more heterogeneous population (for example, disease, aging, so on) as considerable variability in wave reflection characteristics can be attributed to age and sex.45, 46 In the present study, we did not observe significant sex differences in the bilateral PWA discrepancies, but our study was not sufficiently powered to appropriately evaluate this point and should be further characterized. Finally, we used the SphygmoCor system and the findings may not be applicable to different devices and transfer functions. Although methods should be optimized for each PWA system, consideration of the findings herein and intersystem variability should be given for evaluation and titration of treatments and/or interventions.
Conclusion
With respect to the aforementioned variability in bilateral radial artery PWA measures using the SphygmoCor system and the prevalence of clinically different PBP, standard recommendations for PWA are needed for longitudinal clinical monitoring and research comparisons. Here we present novel evidence that SphygmoCor PWA in the right radial artery results in significantly more variability than the left radial artery independent of the order of PWA and PBP measurement and calibration pressures. Moreover, our data suggest that bilateral PBP should be evaluated prior to tonometry measurements and PWA in order to identify subjects in whom (1) there may be a significant difference in bilateral PWA outcomes and (2) markedly different reports of aortic blood pressure estimates would be generated depending on the limb selected for PBP calibration if a clinically significant difference in PBP exists. Therefore, when possible, we suggest simultaneous assessment of PBP prior to radial artery tonometry and that the left arm be utilized for SphygmoCor tonometry measurements. Moreover, when a clinically significant difference in bilateral PBP is observed several things should be considered, including, but not limited to, exclusion from research studies or bilateral assessment of PWA with careful analytical consideration of treatment effects. As our findings highlight, future studies should invasively determine the most accurate method for assessing radial artery PWA in these persons. In the interim, when noninvasive estimates of central pressure are primary outcomes of interest in persons with a clinically significant difference in bilateral PBP, the higher PBP observed should be used for calibration as this is more consistent with guidelines for determination of hypertensive status using brachial artery PBP.21
References
Agabiti-Rosei E, Mancia G, O’Rourke MF, Roman MJ, Safar ME, Smulyan H, Wang J-G, Wilkinson IB, Williams B, Vlachopoulos C . Central blood pressure measurements and antihypertensive therapy: a consensus document. Hypertension 2007; 50: 154–160.
Nichols WW, Singh BM . Augmentation index as a measure of peripheral vascular disease state. Curr Opin Cardiol 2002; 17: 543–551.
Sabovic M, Safar ME, Blacher J . Is there any additional prognostic value of central blood pressure wave forms beyond peripheral blood pressure? Curr Pharm Des 2009; 15: 254–266.
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J 2010; 31: 1865–1871.
Otsuka T, Munakata R, Kato K, Kodani E, Ibuki C, Kusama Y, Seino Y, Kawada T . Oscillometric measurement of brachial artery cross-sectional area and its relationship with cardiovascular risk factors and arterial stiffness in a middle-aged male population. Hypertens Res 2013; 36: 910–915.
Beck DT, Martin JS, Nichols WW, Gurovich AN, Braith RW . Validity of a Novel Wristband Tonometer for Measuring Central Hemodynamics and Augmentation Index. Am J Hypertens 2014; 27: 926–931.
Jatoi NA, Mahmud A, Bennett K, Feely J . Assessment of arterial stiffness in hypertension: comparison of oscillometric (Arteriograph), piezoelectronic (Complior) and tonometric (SphygmoCor) techniques. J Hypertens 2009; 27: 2186–2191.
Wassertheurer S, Kropf J, Weber T, van der Giet M, Baulmann J, Ammer M, Hametner B, Mayer CC, Eber B, Magometschnigg D . A new oscillometric method for pulse wave analysis: comparison with a common tonometric method. J Hum Hypertens 2010; 24: 498–504.
Narayan O, Casan J, Szarski M, Dart AM, Meredith IT, Cameron JD . Estimation of central aortic blood pressure: a systematic meta-analysis of available techniques. J Hypertens 2014; 32: 1727–1740.
O’Rourke MF, Pauca A, Jiang XJ . Pulse wave analysis. Br J Clin Pharmacol 2001; 51: 507–522.
Chen CH, Nevo E, Fetics B, Pak PH, Yin FC, Maughan WL, Kass DA . Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure. Validation of generalized transfer function. Circulation 1997; 95: 1827–1836.
Pauca AL, O’Rourke MF, Kon ND . Prospective Evaluation of a Method for Estimating Ascending Aortic Pressure From the Radial Artery Pressure Waveform. Hypertension 2001; 38: 932–937.
Sharman JE, Lim R, Qasem AM, Coombes JS, Burgess MI, Franco J, Garrahy P, Wilkinson IB, Marwick TH . Validation of a generalized transfer function to noninvasively derive central blood pressure during exercise. Hypertension 2006; 47: 1203–1208.
Nichols W, O’Rourke M, Vlachopoulos C . McDonald’s Blood Flow in Arteries, Sixth Edition: Theoretical, Experimental and Clinical Principles. CRC Press: Boca Raton, FL, USA, 2011.
Shih Y-T, Cheng H-M, Sung S-H, Hu W-C, Chen C-H . Quantification of the calibration error in the transfer function-derived central aortic blood pressures. Am J Hypertens 2011; 24: 1312–1317.
Singer AJ, Hollander JE . Blood pressure. Assessment of interarm differences. Arch Intern Med 1996; 156: 2005–2008.
Lane D, Beevers M, Barnes N, Bourne J, John A, Malins S, Beevers DG . Inter-arm differences in blood pressure: when are they clinically significant? J Hypertens 2002; 20: 1089–1095.
Pauca AL, Wallenhaupt SL, Kon ND, Tucker WY . Does radial artery pressure accurately reflect aortic pressure? CHEST J 1992; 102: 1193–1198.
Sato T, Nishinaga M, Kawamoto A, Ozawa T, Takatsuji H . Accuracy of a continuous blood pressure monitor based on arterial tonometry. Hypertension 1993; 21: 866–874.
Belghazi J, El Feghali RN, Moussalem T, Rejdych M, Asmar RG . Validation of four automatic devices for self-measurement of blood pressure according to the International Protocol of the European Society of Hypertension. Vasc Health Risk Manag 2007; 3: 389–400.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ . Recommendations for blood pressure measurement in humans and experimental animals part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111: 697–716.
Verbeke F, Segers P, Heireman S, Vanholder R, Verdonck P, Bortel LMV . Noninvasive assessment of local pulse pressure importance of brachial-to-radial pressure amplification. Hypertension 2005; 46: 244–248.
Bazaral MG, Welch M, Golding LA, Badhwar K . Comparison of brachial and radial arterial pressure monitoring in patients undergoing coronary artery bypass surgery. Anesthesiology 1990; 73: 38–45.
Mahieu D, Kips J, Rietzschel ER, De Buyzere ML, Verbeke F, Gillebert TC, De Backer GG, De Bacquer D, Verdonck P, Van Bortel LM, Segers P . Noninvasive assessment of central and peripheral arterial pressure (waveforms): implications of calibration methods. J Hypertens 2010; 28: 300–305.
Picone D, Climie R, Keske M, Sharman J . Non-invasive estimation of exercise central blood pressure by radial tonometry may be underestimated due to brachial-to-radial-systolic-blood-pressure-amplification and is related to upper limb blood flow velocity. Artery Res 2014; 8: 124–125.
White WB, Berson AS, Robbins C, Jamieson MJ, Prisant LM, Roccella E, Sheps SG . National standard for measurement of resting and ambulatory blood pressures with automated sphygmomanometers. Hypertension 1993; 21: 504–509.
Smulyan H, Safar ME . Blood pressure measurement: retrospective and prospective views. Am J Hypertens 2011; 24: 628–634.
Wilkinson IB, Fuchs SA, Jansen IM, Spratt JC, Murray GD, Cockcroft JR, Webb DJ . Reproducibility of pulse wave velocity and augmentation index measured by pulse wave analysis. J Hypertens 1998; 16: 2079–2084.
Martin JS, Casey DP, Gurovich AN, Beck DT, Braith RW . Association of age with timing and amplitude of reflected pressure waves during exercise in men. Am J Hypertens 2011; 24: 415–420.
Martin JS, Beck DT, Gurovich AN, Braith RW . The acute effects of smokeless tobacco on central aortic blood pressure and wave reflection characteristics. Exp Biol Med Maywood NJ 2010; 235: 1263–1268.
Martin Bland J, Altman D . Statisical methods for assessing agreement between two methods of clinical measurement. The Lancet 1986; 327: 307–310.
Shimizu M . Blood flow in a brachial artery compressed externally by a pneumatic cuff. J Biomech Eng 1992; 114: 78–83.
Pesola GR, Pesola HR, Lin M, Nelson MJ, Westfal RE . The normal difference in bilateral indirect blood pressure recordings in hypertensive individuals. Acad Emerg Med 2002; 9: 342–345.
Clark CE, Campbell JL, Evans PH, Millward A . Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic review. J Hum Hypertens 2006; 20: 923–931.
Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, Sever PS, McG Thom S . British Hypertension Society. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens 2004; 18: 139–185.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ . National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA J Am Med Assoc 2003; 289: 2560–2572.
Wingfield D, Pierce M, Feher M . Blood pressure measurement in the community: do guidelines help? J Hum Hypertens 1996; 10: 805–809.
Roman MJ, Devereux RB, Kizer JR, Lee ET, Galloway JM, Ali T, Umans JG, Howard BV . Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the Strong Heart Study. Hypertension 2007; 50: 197–203.
Baller DD, Bretschneider HJ, Hellige G . A critical look at currently used indirect indices of myocardial oxygen consumption. Basic Res Cardiol 1981; 76: 163–181.
Harrison EG Jr, Roth GM, Hines EA Jr . Bilateral indirect and direct arterial pressures. Circulation 1960; 22: 419–436.
Hashimoto J, Nichols WW, O’Rourke MF, Imai Y . Association between wasted pressure effort and left ventricular hypertrophy in hypertension: influence of arterial wave reflection. Am J Hypertens 2008; 21: 329–333.
Brown DW, Giles WH, Croft JB . Left ventricular hypertrophy as a predictor of coronary heart disease mortality and the effect of hypertension. Am Heart J 2000; 140: 848–856.
Hashimoto J, Watabe D, Hatanaka R, Hanasawa T, Metoki H, Asayama K, Ohkubo T, Totsune K, Imai Y . Enhanced radial late systolic pressure augmentation in hypertensive patients with left ventricular hypertrophy. Am J Hypertens 2006; 19: 27–32.
Grossman A, Prokupetz A, Gordon B, Morag-Koren N, Grossman E . Inter-Arm Blood Pressure Differences in Young, Healthy Patients. J Clin Hypertens 2013; 15: 575–578.
Ring M, Eriksson MJ, Zierath JR, Caidahl K . Arterial stiffness estimation in healthy subjects: a validation of oscillometric (Arteriograph) and tonometric (SphygmoCor) techniques. Hypertens Res 2014; 37: 999–1007.
Doonan RJ, Mutter A, Egiziano G, Gomez Y-H, Daskalopoulou SS . Differences in arterial stiffness at rest and after acute exercise between young men and women. Hypertens Res 2013; 36: 226–231.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Rights and permissions
About this article
Cite this article
Martin, J., Borges, A., Christy IV, J. et al. Considerations for SphygmoCor radial artery pulse wave analysis: side selection and peripheral arterial blood pressure calibration. Hypertens Res 38, 675–683 (2015). https://doi.org/10.1038/hr.2015.36
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.36
Keywords
This article is cited by
-
Ischemic preconditioning has no effect on maximal arm cycling exercise in women
European Journal of Applied Physiology (2020)
-
Validity of the augmentation index and pulse pressure amplification as determined by the SphygmoCor XCEL device: a comparison with invasive measurements
Hypertension Research (2018)
-
Comparison of invasive and brachial cuff-based noninvasive measurements for the assessment of blood pressure amplification
Hypertension Research (2017)
-
Mean arterial pressure values calculated using seven different methods and their associations with target organ deterioration in a single-center study of 1878 individuals
Hypertension Research (2016)
-
Influence of the central-to-peripheral arterial stiffness gradient on the timing and amplitude of wave reflections
Hypertension Research (2016)