Abstract
Purpose
To study the relationship between age and response to surgery in patients with intermittent exotropia and to identify change points in response to surgery.
Methods
A retrospective analysis was conducted on 311 patients with intermittent exotropia who had bilateral lateral rectus recession using standard tables with minimum follow-up of 6 months. Data were analyzed using the change-point analysis software to identify cutoff points. A prospective pilot study was then performed on 171 consecutive patients with intermittent exotropia with the same clinical characteristics, in whom amount of recession was modified according to the identified cutoff points. In angles with two change points, 1-mm recession was reduced from patients younger than the lower change point and 1.5-mm recession was added to those older than the upper change point. In angles with one change point, 1.5-mm recession was added to those older than the change point. Satisfactory alignment was defined as esophoria/tropia ≤5Δ to exophoria/tropia ≤8Δ.
Results
There was a negative correlation (P<0.01) between response to surgery and age at surgery for all angles. In younger patients (<7 years) in whom surgical dose was reduced, there was no significant change in success rate (77%), compared with those who had surgery using standard tables (75%). In older patients (>12 years) in whom surgical dose was increased, there was a statistically significant increase in success rate (80% vs 41%).
Conclusions
Modifying the surgical dose according to age can improve the success in patients with intermittent exotropia.
Similar content being viewed by others
Introduction
Intermittent exotropia is fairly common with a prevalence ranging from 0.43–1.7%,1 but the exact cause is not yet known. Several surgical approaches have been used successfully to correct exotropia, but the most frequently used is recession of both lateral rectus muscles.2, 3, 4, 5
The amount of recession of the lateral rectus muscles varies according to the measured angle of deviation, and provided there is no incomitance in lateral gaze and visual acuity is equal in both eyes, most surgeons use amounts of recession that are similar to those used by other strabismologists.6, 7
Other than the preoperative angle of deviation and the amount of performed surgery, many factors were found to influence the response to strabismus surgery. These include patients’ age at onset of deviation, patients’ age at surgery, interval between onset and surgery, refractive error, degree of anisometropia, visual acuity, presence of amblyopia, presence of an A- or a V-pattern, type of exotropia, and existence of binocular single vision before surgery.8, 9, 10, 11, 12, 13, 14, 15, 16, 17
Studies on the relationship between age at surgery and surgical response had shown variable and contradictory results. Although some studies showed a larger response to surgery with higher incidence of overcorrection in younger age groups,8, 9, 10 other studies concluded that there is no relationship between age at surgery and response to surgery.12, 13, 14, 15, 16 Keech and Stewart17 even reported that patients with persistent overcorrection had a two-fold higher mean age at the time of surgery compared with those who did not have persistent overcorrection.
Due to this discrepancy as well as the wide variety of factors contributing to the outcome, this study was conducted to evaluate whether there is a relation between the age at the time of surgery and the response to surgery in patients who had bilateral lateral rectus recession surgery for the treatment of intermittent exotropia.
Materials and methods
The study was approved by Cairo University research ethics committee. The study and data collection conformed to all local laws and were compliant with the principles of the Declaration of Helsinki. A written informed consent for the surgery was obtained from all patients or their guardians.
Initial retrospective part
In the first part of the study, a retrospective chart review was done to identify patients who had bilateral lateral recession for intermittent exotropia during the period from January 2007 to July 2010.
Patients were included in the study if they had intermittent exotropia of basic type (defined as distance deviation within 10 prism diopter (PD) of the near deviation) or true divergence type (distance deviation is greater than the near deviation by more than 10 PD).
Patients were excluded from the study if they had paralytic or consecutive exotropia, a history of prior eye muscle surgery, oblique muscle dysfunction or significant A- or V-patterns (difference between angle of horizontal misalignment in upgaze and downgaze more than 10 PD), or a postoperative follow-up period<3 months. Because a number of variables are known to influence the outcome to surgery in patients with intermittent exotropia, patients with such variables were excluded from the study. Thus, patients with systemic or neurological disorders were excluded from the study. Patients with any degree of amblyopia (a difference of two or more lines in Snellen visual acuity charts between the best-corrected visual acuity of each eye or a best-corrected visual acuity lower than 20/30) or anisometropia (an absolute difference of the spherical equivalent of two or more diopters between the right and left eyes) were excluded from the study. Patients with significant myopia (spherical equivalent >3 D) or hypermetropia (spherical equivalent >4 D) were excluded from the study as some studies concluded that they showed a poorer response to surgery and a greater risk of consecutive esotropia.14 Patients with lateral gaze incomitance defined as reduction in the angle of exodeviation of 20% or more upon lateral gazing were excluded from the study. In addition, patients with constant exotropia, or intermittent exotropia of very poor control simulating constant exotropia (Newcastle control score=7)18 were also excluded from the study.
Refractive error values were obtained from cycloplegic refraction test using 1% cyclopentolate; all data were obtained in the 3 months before surgery. Patients who had hyperopia of more than +2.00 diopters, astigmatism more than 1.00 D or any degree of myopia were prescribed glasses prior to any surgical intervention and then re-evaluated 1 month later. Myopia and astigmatism were fully corrected. Hypermetropia was corrected partially after removing 1.00 D from the cycloplegic refraction.
All patients had a detailed sensorimotor examination during the initial evaluation and at each follow-up period. Angle was measured using plastic prisms held with the rear surface of the prism in the frontal plane of the patient.19, 20 Prism bars were used to measure the angle of deviation to the closest 2 PD (for angles less than or equal to 20 PD) and to the closed 5 PD (for angles more than 20 PD). The angle was then checked again using separate prisms placed in front of one or both the eyes to get the angle to the nearest 2 PD.
Angle of deviation was measured using prolonged prism and alternating cover test with the patient looking at a distance target approximately six meters from the patient, then repeated again at 33 cm with the patient looking at an accommodative target. The angle of deviation was measured with and without glasses for both distance and near.
In patients with significant distance–near discrepancy (>10 Δ) or significant angle variability during alternate cover test, one eye was patched for ∼60 min. The deviation was then measured again without letting the patient restore binocular vision, both to disrupt fusion and disclose the full latent deviation, and to differentiate true from simulated divergence excess. Accommodation was controlled with appropriate accommodative targets during the measurements of the deviation.
The angle of horizontal misalignment was also measured in side gazes and in straight up and down gazes. Measurement of the angle of deviation in up and down gazes was done by tilting the head, ∼25 degrees up and down, respectively, with the patient fixing on a distance target. The difference between the angles of horizontal misalignment in up and down gazes was used to calculate the amount of pattern strabismus, if present.
Lateral gaze incomitance was measured with the patient fixing on the distance target by rotating the head around a vertical axis until the adducting eye could no longer fixate the target. The head was then rotated back toward primary position until the eye could just fixate the target. This was generally about 30 degrees of lateral gaze. Prism and alternate cover measurements were then performed with the prism placed over the adducting eye and held with its posterior surface perpendicular to the direction of the fixation target.21, 22
For patients with basic exotropia, the preoperative and postoperative angle of deviation was calculated for each subject as angle of deviation for distance—with appropriate spectacle correction whenever needed. For patients with true divergence excess, the angle of deviation was calculated as the average of angle for distance and near—with appropriate spectacle correction whenever needed.7
Sensory evaluation was performed for all patients, using 4-PD base-out prism test to detect foveal suppression, Worth 4-dot test (for distance) to assess fusion and the Netherlands Organization for Applied Scientific Research (TNO) stereo test to assess stereopsis.
All patients had bilateral lateral rectus recession only with no other eye muscle surgery at the same time. The surgical dosage calculated for lateral rectus recession was according to the standard previously published tables.7 All surgeries were performed under general anesthesia, by one surgeon (AA) using a fornix incision. The conjunctiva was incised and the lateral rectus muscle was exposed. It was then recessed and fixed to the sclera under direct visualization, according to the deviation angle. The conjunctiva was then approximated and sutured.
For statistical analysis, the final short-term outcome was measured 6 months after surgery to estimate the effect of lateral rectus muscles recession. Satisfactory surgical alignment was defined as esophoria/tropia ≤5 Δ to exophoria/tropia ≤8 Δ in primary gaze. The response to surgery was calculated as the algebraic difference between the preoperative and postoperative angle of deviation for distance. Pearson’s Correlation coefficient was used to assess the relationship between age and response to surgery, and a P-value less than 0.05 was considered significant.
Change-point analysis
The data collected was analyzed using the change-point analysis software (Change-Point Analyzer 2.3 shareware program, Taylor Enterprises, Libertyville, IL, USA), for determining whether a change has taken place in the response to surgery with increasing age at surgery. Change-point analysis iteratively uses a combination of cumulative sum charts (CUSUM) and bootstrapping to detect changes. It is capable of detecting multiple changes and for each change it provides a detailed information, including a confidence level indicating the likelihood that a change occurred.23
Prospective part
According to the results obtained from the change-point analysis, a prospective pilot study was performed on all consecutive patients with intermittent exotropia with the same clinical characteristics, from December 2010 to July 2012, in which the surgical dosage for lateral rectus recession was adjusted and then data collected.
In the prospective part of the study, all patients had a detailed sensorimotor examination during the initial evaluation and at each follow-up period similar to that done in the retrospective part of the study. Surgical technique was also similar. However, surgical doses were adjusted according to the identified cutoff point. In angles of exotropia with two identified change points, 1-mm less recession was reduced from those below the lower change point and 1.5-mm more recession was added to those above the upper change point. Amount of recession was kept constant for those between the lower and upper change points. For angles of misalignment with one change point, the amount of recession was modified, so that 1.5-mm recession was added to those older than the change point. Patients younger than the change point had no change to standard tables. The data of all patients were also tabulated and compared with those in the retrospective part of the study who had surgery using the standard tables.
We certify that all applicable institutional and governmental ethical regulations were followed during this research.
Results
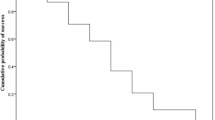
A total of 311 patients fulfilled the inclusion criteria in the retrospective study. A summary of the included patients is shown in Table 1 and Supplementary Table 1. There was a statistically significant negative correlation (P<0.01) between the response to surgery and the age of the patient for all angles of exotropia (Figure 1).
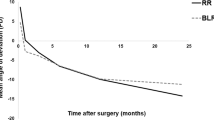
Change-point analysis was then done to identify the changes in the response to surgery for each range of angle of exotropia (Figure 2). Change-point analysis identified two change points in response to surgery at age 7 and at age 12 years for angles of exotropia 20–35 PD. For larger angles, only one change point could be identified, at age 12 years (Table 2).
Graphical representation of the results of change-point analysis showing the relationship of the response to surgery after BLR recession to age for angles of exotropia 30–34 PD. Top panel: graph depicting the mean amount of exotropia corrected in different age groups. The change points in the response to surgery are represented by the shifts in the shaded background. The shaded background represents a region expected to contain all the values based on the current model that two changes occurred. The control limits (red lines) assume the values come from the normal distribution. As some points are outside the control limits, the control chart also indicates that change occurred. Bottom panel: cumulative sums chart showing cumulative sums of differences between the values and the average amount of exotropia corrected. Using bootstrap analysis, two significant change points can be seen around the age of 7 years and around the age of 13 years.
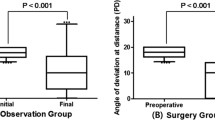
Patients were divided into three groups on the basis of the age, 4–6 years, 7–12 years, and >12 years to evaluate the success rate in each group individually. The difference in the success rate between different age groups was statistically significant for all angles (P<0.05). There was a tendency toward higher rate of undercorrection in older age and higher rate of overcorrection in younger age. The highest degree of satisfactory motor alignment was achieved in patients 7–12 years old following the standard tables (91%), whereas 71% achieved satisfactory motor alignment in the 4–6-year-old group and only 41% achieved it in the above 12-year-old group.
During the prospective part of the study, amount of muscle recession was modified according to the identified cutoff point. For lower range of angles of exotropia with two identified change points, 1-mm recession was reduced from patients below (younger than) the lower change point and 1.5-mm recession was added to those above (older than) the upper change point. Amount of recession was kept constant for those between the lower and upper change points. For higher angles of misalignment with one change point, the amount of recession was modified, so that 1.5-mm recession was added to those older than the change point. Patients younger than the change point had no change to the standard tables.
During the second part of the study, 171 patients with intermittent exotropia who fulfilled the same inclusion criteria were identified (Table 1 and Supplementary Table 2). The difference in the success rates between patients who had surgery using the standard tables and those who had surgery using the modified numbers is shown in Table 3. In younger patients (4–6 years old) in whom the surgical dose was reduced, there was no significant change in success rate for satisfactory alignment (77%), compared with those who had surgery using the standard tables (75%). However, in children who had these reduced numbers, there was a statistically significant lower rate of overcorrection, but a higher rate of undercorrection. In older patients (>12 years) in whom the surgical dose was increased, there was however a statistically significant increase in success rate (80% using the augmented number vs 41% using standard tables) with marked reduction in undercorrection rate (20% using the augmented number vs 59% using standard tables). For those in whom the surgical dose was not adjusted, there was no statistically significant difference in success rate (88% in the prospective part vs 91% in the retrospective part).
Discussion
Age at the time of surgery has been studied as a factor that can predict the outcome of postoperative alignment, with different results. Park and his colleagues24 showed that patients older than 15 years tend to show better postoperative alignment with no tendency for overcorrection when compared with those younger than 15 years old, although the difference was not significant. Studies by Richard and Parks,15 showed no difference in surgical outcome in children in age groups; younger than 3, between 3–6, and older than 6 years.
In our study, we demonstrated that age at the time of surgery was negatively associated with the response to surgery as noted by postoperative alignment for all angles studied, showing the highest undercorrection for patients older than 12 years (59%), and no overcorrection in this group.
Moreover, in this study, change-point analysis was able to identify change points in the response to surgery with increasing age at surgery. Change-point analysis identified two change-point ages for angles of exotropia 20–35 PD. The two change points were around the age of 7 years and age of 12 years. This accounts for the higher incidence of overcorrection in children below 7 years in the study when surgery was done using standard tables. However, for larger angles, only one change point could be identified around the age of 12 years. This suggests that for larger angles of exotropia, there was no identifiable change point below 12 years. Jang and his associates14 reported similar findings with a higher incidence of overcorrection with standard tables for lower preoperative angles of deviation (25–40 PD) compared with those with larger angles of deviation.
Reducing the amount of lateral rectus recession by 1 mm in children younger than the lower change point (4–6 years old) in patients with exotropia 20–35 PD did not significantly change the success rate. However, the number of patients with overcorrection was statistically significantly lower using these modified numbers. This was balanced by a higher rate of undercorrection using these reduced numbers.
On the other hand, increasing the amount of lateral rectus recession by 1.5 mm in adults older than the upper change point (around 12 years) have both improved the success rate and reduced the incidence of undercorrection in a statistically significant way. Lee and his associates25 have suggested increasing the amount of lateral rectus recession by 1.5–2.5 mm for each eye in patients with intermittent exotropia and they reported an increase in success rate from 43.9% to 68.2% with a drop of undercorrection from 53.7% to 30.3% in the augmented formula group. In our study, increasing the amount of recession by 1.5 mm has significantly improved the success rate similarly from 41% to 80% in patients older than 12 years old. We have chosen to increase the amount of recession by 1.5 mm only as it was felt from the results of initial retrospective part that the amount of recession needed to be increased only slightly, and to minimize variables in interpreting the outcome. We are not aware of a study that defines the age limit for using a modified formula for recession in patients with intermittent XT, and correlates it to the angle of deviation. This improvement in the results cannot be attributed to historical bias as evident by the similarity of outcome in the patients 7–12 years old where the surgical tables were not modified in both the retrospective and prospective pilot groups.
The relation between the effect of recession and age may be explained by the width of the lateral rectus tendon. In a study by Yun and Kim26, they found tendon widths for patients under 5 years were narrower than older patients and they suggested modifying the degree of surgery according to the tendon width. Another factor that may justify the difference in the response with increasing age are the changes that may occur in the muscles and periocular tissue with increasing duration of strabismus that may mandate to augment the surgical dose to get the same response.
As there are other variables that may affect the outcome of surgery such as the type of surgery (bilateral lateral rectus recession vs unilateral recession–resection), neurological disorders, amblyopia, high refractive errors, oblique muscle dysfunction or pattern strabismus,8, 9, 10, 11, 12, 13, 14, 15, 16, 17 we excluded all these patients from both the retrospective and prospective part of the study in an attempt to make the study population more homogenous.
A limitation of this study design is that we used the retrospective data to evaluate the response to surgery and to calculate the change points. We however, tried to compensate for that by testing the validity of the results in the prospective part of the study. Nevertheless, further evidence is needed by comparing the results of lateral rectus recession using standard tables to those with the modified numbers using a prospective randomized controlled study design.
In conclusion, modifying the standard strabismus tables according to age can improve the surgical outcome in patients with intermittent exotropia. For patients 4–7 years old, the standard tables work well; whereas for patients 12 years or older, increasing the amount of recession by 1.5 mm significantly increased the success rate from 41% to 80%.
References
Govindan M, Mohney BG, Diehl NN, Burke JP . Incidence and types of childhood exotropia: a population-based study. Ophthalmology 2005; 112: 104–108.
Knapp PK . Treatment of divergent deviations. In: Allen JH, (ed.) Strabismus Symposium II. C.V. Mosby Co: St Louis, 1958; 364.
Burian HM . Exodeviations: their classification, diagnosis and treatment. AmJOphthalmol 1966; 62: 1161.
Harley RD . Pediatric Ophthalmology 2nd edition W.B. Saunders Co.: Philadelphia, 1983; 238–239.
Peyman GA . Principles and Practice of Ophthalmology 1st ed. W.B. Saunders Co.: Philadelphia, 1980; 1846–1849.
Berland JE, Wilson ME, Saunders RA . Results of large (8–9 mm) bilateral lateral rectus muscle recession for exotropia. Binocul Vis. Strabismus Q 1998; 13: 97.
Parks MM, Mitchell P . Concomitant exodeviations. In: Duane TD, (ed.) Clinical Ophthalmology. JB Lippincott: Philadelphia, 1988; 1–10.
Scott AB, Mash AJ, Jampolsky A . Quantitative guidelines for exotropia surgery. Invest Ophthalmol 1975; 14: 428–436.
Edelman PM, Brown MH, Murphee AL, Wright KW . Consecutive esodeviation, then what? Am Orthopt J 1988; 38: 111–116.
Clacke WN, Noel LP . Surgical results in intermittent exotropia. Can J Ophthalmol 1981; 16: 66–69.
Gordon YJ, Bachar E . Multiple regression analysis predictor models in exotropia surgery. Am J Ophthalmol 1980; 90: 687–691.
Kushner BJ, Fisher MR, Lucchese NJ, Morton GV . Factors influencing response to strabismus surgery. Arch Ophthalmol 1993; 111: 75–78.
Abbasoglu OE, Sener EC, Sanac AS . Factors influencing the successful outcome and response in strabismus surgery. Eye 1996; 10: 315–320.
Jang JH, Park JM, Lee SJ . Factors predisposing to consecutive esotropia after surgery to correct intermittent exotropia. Graefes Arch Clin Exp Ophthalmol 2012; 250: 1485–1490.
Richard JM, Parks MM . Intermittent exotropia surgical results in different age groups. Ophthalmology 1983; 90: 1172–1177.
Dunlap EA . Overcorrections in exotropia surgery. In: Manley DR, (ed.) Symposium On Horizontal Ocular Deviations. Mosby: St Louis, 1971; 183.
Keech RV, Stewart SA . The surgical overcorrection of intermittent exotropia. J Pediatr Ophthalmol Strabismus 1990; 27: 218–220.
Haggerty H, Richardson S, Hrisos S, Strong NP, Clarke MP . The Newcastle Control Score: a new method of grading the severity of intermittent distance exotropia. Br J Ophthalmol 2004; 88: 233–235.
Thompson JT, Guyton DL . Ophthalmic prisms. Measurement errors and how to minimize them. Ophthalmology 1983; 90: 204–210.
Thompson JT, Guyton DL . Ophthalmic prisms. Deviant behavior at near. Ophthalmology 1985; 92: 684–690.
Lennarson LW . Basic experimentation: B detection and measurement of strabismus. In: Scott WE, D’Agostino DD, Lennarson LW, (eds.) Orthotics and Ocular Examination Techniques. Williams & Wilkins: Baltimore, 1983; 233.
Repka MX, Arnoldi KA . Lateral incomitance in exotropia: fact or artifact? J Pediatr Ophthalmol Strabismus 1991; 28: 125–128.
Taylor Wayne A. 2000 ‘Change-Point Analysis: A Powerful New Tool For Detecting Changes,’ WEB: http://www.variation.com/cpa/tech/changepoint.html.
Park HJ, Kong SM, Baek SH . Consecutive esodeviation after exotropia surgery in patients older than 15 Years: comparison with younger patients. Korean J Ophthalmol 2008; 22: 178–182.
Lee SY, Kim JH, Thacker NM . Augmented bilateral lateral rectus recessions in basic intermittent exotropia. J AAPOS 2007; 11: 266–268.
Yun CM, Kim SH . The tendon width of lateral rectus muscle in predicting the effect of recession: is it just age related artifact? Eye 2011; 25: 1356–1359.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Awadein, A., Eltanamly, R. & Elshazly, M. Intermittent exotropia: relation between age and surgical outcome: a change-point analysis. Eye 28, 587–593 (2014). https://doi.org/10.1038/eye.2014.29
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.29
This article is cited by
-
Postoperative outcome and influencing factors of strabismus surgery in infants aged 1–6 years
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Comitant strabismus etiology: extraocular muscle integrity and central nervous system involvement—a narrative review
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Intermediate filaments in the medial rectus muscles in patients with concomitant exotropia
International Ophthalmology (2020)