Abstract
Objective
To evaluate the 12-month clinical outcome of patients with persistent non-ischaemic diffuse diabetic macular oedema (DME) treated with intravitreal bevacizumab (IVB) or with intravitreal injection of triamcinolone combined with macular laser grid (IVTA-MLG) from September 2005 to February 2008.
Methods
Retrospective interventional comparative study. Best-corrected visual acuity (BCVA, ETDRS LogMAR scale) and foveal thickness (FT) at optical coherence tomography (OCT) were obtained at baseline and during 12 months after first treatment. Re-treatment was based on clinical or OCT-based evidence of persistent macular oedema or deterioration in visual acuity.
Results
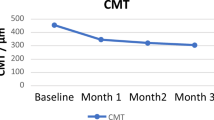
Forty-three eyes (32 patients) with DME were treated with IVB. Ninety-six eyes (52 patients) with DME were treated with combined laser grid treatment and intravitreal triamcinolone. At baseline, mean BCVA and FT were 0.92±0.34 LogMAR and 372±22 μm in the IVTA-MLG group, and 1.07±0.49 LogMAR and 423±33 μm in the IVB group, respectively. At 1- and 3-month visits, BCVA and FT had significantly improved in both groups. After 6 and 12 months, the IVB group experienced a statistically significant improvement in visual acuity (0.83±0.21 LogMAR, P<0.001 at 6 months; BCVA 0.86±0.24 LogMAR, P<0.001 at 12 months) and FT (248±18 μm, P<0.001 at 6 months; 262±28 μm, P=0.001 at 12 months) when compared with baseline, whereas the IVTA-MLG group did not show statistically significant improvement in vision and FT. An increase in intraocular pressure (IOP) was present in 10 of 96 (10.4%) eyes treated with IVTA-MLG, and in two cases it was resistant to topical treatment. No significant side effects were reported in the IVB group.
Conclusions
At 6 and 12 months after first treatment for chronic DME IVB provided significant improvement of BCVA and FT, whereas improvement after IVTA-MLG was not significant. Increased IOP occurred in 10.4% of patients who received IVTA, with two patients requiring trabeculectomy.
Similar content being viewed by others
Introduction
Diabetic macular oedema (DME) is a major cause of visual loss in patients with diabetes.1, 2 For patients presenting with DME for the first time, macular laser grid (MLG) photocoagulation is currently the standard treatment. The Early Treatment of Diabetic Retinopathy Study showed that MLG reduced moderate visual loss in eyes with clinically significant macular oedema.3 However, especially for chronic diffuse macular oedema, MLG is not always beneficial.3, 4, 5 Hypoxia-induced expression of vascular endothelial growth factor (VEGF) has been shown to have a major role in the development of retinal oedema in diabetes.6, 7 Intravitreal injection of triamcinolone acetonide (TA) has been reported to improve visual acuity and to reduce the macular thickness in eyes with diffuse DME8, 9, 10, 11, 12 by inhibition of the arachidonic acid pathway and downregulation of the production of VEGF. Nevertheless, improvement strictly depends on TA persistence in the vitreous,13 and a main limitation is the high rate of side effects such as cataract formation or increased intraocular pressure (IOP).14, 15 The off-label use of intravitreal VEGF inhibitor, bevacizumab, for the treatment of DME showed promising functional and anatomical results in short- and long-term studies.16, 17, 18
In this retrospective study, we evaluated the 12-month clinical outcome of patients with persistent non-ischaemic diffuse DME treated with intravitreal bevacizumab (IVB) alone or with intravitreal injection of triamcinolone combined with MLG.
Methods
The study design was a retrospective interventional comparative evaluation of all consecutive patients with non-tractive diffuse macular oedema treated with IVB or combined intravitreal triamcinolone acetonide-MLG (IVTA-MLG) photocoagulation at the Eye Department of the University Federico II of Naples from September 2005 to February 2008. The study followed the tenets of the Declaration of Helsinki and had Institutional Research Board approval. Unlike the ETDRS definition, diffuse macular oedema was defined as a diffuse thickening of the retina up to the vascular arcades including the fovea, and an optical coherence tomography (OCT) measured retinal thickness of ⩾250 μm in the central subfield. Exclusion criteria for treatment were the presence of dense or opaque media, ocular trauma, inflammation, or surgery in the previous 12 months; previous pan-retinal photocoagulation; glaucoma or IOP >18 mm Hg in a measurement before the study, poorly controlled (not responding to treatment) diabetes, hypertension, or nephropathy. Eyes with macular ischaemia were excluded. Macular ischaemia was defined as angiographic evidence of foveal avascular zones 1000 μm or larger, or broken perifoveal capillary rings at the borders of the foveal avascular zone, with distinct areas of capillary non-perfusion within one disk diameter of the foveal centre, as seen in the transit phase of fluorescein angiography.
Data collection included the evaluation of best-corrected visual acuity (BCVA) according to the Early Treatment Diabetic Retinopathy Study (ETDRS) LogMAR scale, clinical examination, mean thickness in the central 1000-μm diameter area (foveal thickness, FT) at OCT (Stratus OCT, software version 4.0.1, Carl Zeiss, Dublin, CA, USA). To obtain FT a high-resolution Radial Line scan protocol (6 diagonal 6-mm scans, 1.0 B scans per second, 512 axial measurements with a resolution of around 10 microns) was used. Patients were observed according to the physician's discretion, at 1- to 2-month intervals. At baseline, between 2 and 3 months, and between 8 and 12 months from first treatment colour fundus photographs and fluorescein angiography were performed.
On each follow-up visit, possible side effects of the treatment (IOP ⩾23 mm Hg, anterior chamber reaction, severe lens opacity, vitreous haemorrhage, endophthalmitis, retinal detachment, significant blood pressure increase, thromboembolic events) were ruled out.
Surgical procedure
All injections were administered in the operating room through the pars plana with topical anaesthesia (Tetracaine, Novartis, Basel, Switzerland) according to standard procedures.19 Patients were treated with IVB (0.05 ml solution prepared from Avastin 100 mg per 4 ml vial; Roche, Basel, Switzerland). Each patient was informed of the off-label status of bevacizumab and informed consent was obtained. Patients treated with combined IVTA-MLG received an intravitreal injection of TA (4 mg, 0.1 ml; Kenacort-A; Bristol-Myers Squibb, Sermoneta, Latina, Italy) and MLG according to ETDRS guidelines3 after a time ranging from 2 to 3 weeks from IVTA. Photocoagulation in spots of 100–200 μm diameter in the macular area, at a distance of one to two spots from one to another, in concentric lines, with an exposure time of 0.2–0.5 s, was performed, with sparing of the central area.
Re-treatment was based on clinical or OCT-based evidence of persistent macular oedema or deterioration in visual acuity. As this was a retrospective study, the choice of re-treatment was at the discretion of the physician. Re-treatment in the IVB group was performed with IVB after a minimum interval of 6 weeks. Re-treatment with IVTA-MLG was performed with IVTA alone after a minimum interval of 4 months.
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (version 13.0, SPSS Inc, Chicago, IL, USA). Baseline demographic and clinical parameters were compared between treatment groups using Student's t-tests for continuous variables and χ2-tests for the categorical variables. Between-group comparisons at each time point were performed using Student's t-test. Repeated-measures ANOVA with Dunnett correction for multiple comparisons was used to compare follow-up to baseline data within a treatment group. The level of statistical significance was set at P<0.05.
Results
All treated patients suffered from type II diabetes. Data about demographic characteristics of the two groups at baseline are resumed in Table 1.
Forty-three eyes (32 patients) with DME were treated with IVB. Ninety-six eyes (52 patients) with DME were treated with combined laser grid treatment and intravitreal triamcinolone. No significant differences were present between the two groups with regard to sex ratio, age, duration of diabetes and DME, BCVA, and FT. Duration of macular oedema was 12.6±2.3 months in the IVB group and 14.3±3.7 months in the IVTA+MLG group. Leakage at fluorescein angiography was diffuse in all cases.
During 12 months, patients in the IVB group were given a mean number of 4.4±0.4 injections. A mean number of 2.5±0.5 injections was administered in the IVTA-MLG group.
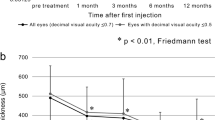
After 1 and 3 months, significant improvement of BCVA was present in both groups (Table 2, Figure 1). Improvement of BCVA was greater in IVB group, but the difference was not significant. A significant improvement of FT was present in both groups at both 1 and 3 months, but the difference between the two groups was not significant. At 6- and 12-month visits, the IVB group experienced a statistically greater improvement of BCVA (P=0.02 and P=0.03, respectively) and FT (P<0.001 and P=0.02, respectively). Between the 3- and 12-month visits, the IVTA-MLG group showed an increase in FT, although it did not reach baseline values.
Correlation (Pearson's ρ) between BCVA and FT changes was 0.42, P=0.03 in the IVB group and 0.32 P=0.02 in the IVTA-MLG group.
During follow-up IOP increased in 10 of 96 (10.4%) eyes treated with IVTA-MLG, and decreased to normal values in eight of them after topical anti-glaucomatous treatment and a period ranging from 3 to 7 months. In two cases, IOP elevation was intractable and was normalised after trabeculectomy. No side effects were reported in the IVB group.
Discussion
To our knowledge, this is the first reported comparison of combined IVTA-MLG treatment and IVB alone for persistent non-ischaemic diffuse DME. Previous studies have compared IVTA and IVB and combined IVB-IVTA and MLG.17, 20, 21, 22, 23, 24, 25
BCVA and FT improved in both groups during the first 3 months of follow-up, whereas at 6 and 12 months, the improvement was significant in the IVB group only. A low correlation was found between BCVA and FT, as already reported.26 In a recent paper by Kook et al17 and in the Pan-American Collaborative Retina Study Group,18 IVB for DME improved central retinal thickness and visual function during 6 months of follow-up. In a phase II randomised clinical trial IVB monotherapy did not differ from combined IVB-MLG, as no apparent differences were present with regard to short-term benefit or adverse outcomes.27 No significant differences have been reported in DME between one IVTA injection and two IVB injections during 6 months of follow-up,22 whereas IVTA has shown to be more effective than IVB after a single injection in severe DME.23, 24 Our patients underwent more IVB re-injections because significant levels of triamcinolone are likely to persist inside the eye for at least 4 months,28 whereas the duration of the effect of bevacizumab is presumed to be shorter.29 Therefore, the different minimum interval before re-injections is not likely related to the better results obtained in the IVB group.
Functional and anatomical improvement after IVTA-MLG was significant during the first 3 months only. IVTA was re-injected after at least 4 months, according to reported suggestions.29 Grid photocoagulation was performed 3 weeks after IVTA because this is when IVTA likely exerts the greatest therapeutic effects8, 9, 10, 11, 12 Initial improvement and following recurrence of macular oedema after 6 months from intravitreal triamcinolone have often been described6, 7, 8, 9, 10 and are related to the disappearance of TA from the vitreous. Intravitreal high-dose injection of TA has been suggested to maintain improved VA, reduce the risk of recurrent macular oedema, and prevent retinal damage in eyes with diffuse DME.30 The synergistic effects of MLG after TA injection have been examined by several recent studies, with conflicting results.31, 32, 33 Our results agree with Avitabile et al31 and with Lam et al,32 and do not show long-term improvement despite the adjunct of MLG to IVTA. This could be due to the several factors that may influence the visual outcome, such as the different durations of macular oedema, previous macular laser photocoagulation, patient age, the presence of cataract, glycaemic control, and the presence of hard exudates.
No side effects were present in the IVB group, whereas 10.4% of the eyes treated with IVTA-MLG developed IOP ⩾23 mm Hg during follow-up, and in two cases IOP elevation was resistant to anti-glaucomatous treatment. Several retrospective studies support the local and systemic safety of intravitreal anti-VEGF19, 34 whereas the most frequent adverse effects with corticosteroids are cataract formation and elevation of IOP.35, 36 Notwithstanding the positive effects of triamcinolone on the reduction of macular oedema and improvement of visual function, recurrence of macular oedema and occasional IOP increase have been reported within 24 weeks after IVTA treatment.10 In our study a 4-mg dose of intravitreal triamcinolone was used. According to the recently reported results of the SCORE study37 and DRCR.net study,38 the 1-mg dose of intravitreal triamcinolone for the treatment of central retinal vein occlusions and DME had similar effectiveness and a superior safety profile to that of the 4-mg dose, with regard to the incidence of IOP elevation and cataract formation beyond a period ranging from 12 to 36 months. In our series IVB resulted in a lower incidence of increased IOP when compared with 4-mg IVTA. A prospective study is planned to compare IVB and 1-mg IVTA for the treatment of persistent DME.
The limitation of our study is the retrospective design. However, the long-term effectiveness of both IVB and triamcinolone in diffuse macular oedema has been suggested by several prospective studies.17, 23 A prospective study is planned to confirm our results.
In conclusion, combined IVTA-MLG and IVB showed similar effectiveness in improving visual acuity and reducing macular thickness in diffuse non-ischaemic DME during the first 3 months, whereas at 6 and 12 months, a visual and anatomical improvement was observed in the IVB group only. Intravitreal injection of TA may be associated with IOP elevation, not always responding to anti-glaucomatous treatment.
Summary

References
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL . The Wisconsin epidemiologic study of diabetic retinopathy. IV. Diabetic macular edema. Ophthalmology 1984; 91 (12): 1464–1474.
Moss SE, Klein R, Klein BE . The incidence of vision loss in a diabetic population. Ophthalmology 1988; 95 (10): 1340–1348.
Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol 1985; 103 (12): 1796–1806.
Early Treatment Diabetic Retinopathy Study Research Group. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Ophthalmology 1987; 94 (7): 761–774.
Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol 1995; 113 (9): 1144–1155.
Ishida S, Usui T, Yamashiro K, Kaji Y, Ahmed E, Carrasquillo KG et al. VEGF164 is proinflammatory in the diabetic retina. Invest Ophthalmol Vis Sci 2003; 44 (5): 2155–2162.
Funatsu H, Yamashita H, Nakamura S, Mimura T, Eguchi S, Noma H et al. Vitreous levels of pigment epithelium-derived factor and vascular endothelial growth factor are related to diabetic macular edema. Ophthalmology 2006; 113 (2): 294–301.
Jonas JB, Sofker A . Intraocular injection of crystalline cortisone as adjunctive treatment of diabetic macular edema. Am J Ophthalmol 2001; 132 (3): 425–427.
Martidis A, Duker JS, Greenberg PB, Rogers AH, Puliafito CA, Reichel E et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology 2002; 109 (5): 920–927.
Jonas JB, Kreissig I, Sofker A, Degenring RF . Intravitreal injection of triamcinolone for diffuse diabetic macular edema. Arch Ophthalmol 2003; 121 (1): 57–61.
Ciardella AP, Klancnik J, Schiff W, Barile G, Langton K, Chang S . Intravitreal triamcinolone for the treatment of refractory diabetic macular oedema with hard exudates: an optical coherence tomography study. Br J Ophthalmol 2004; 88 (9): 1131–1136.
Massin P, Audren F, Haouchine B, Erginay A, Bergmann JF, Benosman R et al. Intravitreal triamcinolone acetonide for diabetic diffuse macular edema: preliminary results of a prospective controlled trial. Ophthalmology 2004; 111 (2): 218–224; discussion 224–215.
Beer PM, Bakri SJ, Singh RJ, Liu W, Peters 3rd GB, Miller M . Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology 2003; 110 (4): 681–686.
Karacorlu M, Karacorlu SA, Ozdemir H, Senturk F . Intravitreal triamcinolone acetonide for treatment of serous macular detachment in central retinal vein occlusion. Retina 2007; 27 (8): 1026–1030.
Gregori NZ, Rosenfeld PJ, Puliafito CA, Flynn Jr HW, Lee JE, Mavrofrides EC et al. One-year safety and efficacy of intravitreal triamcinolone acetonide for the management of macular edema secondary to central retinal vein occlusion. Retina 2006; 26 (8): 889–895.
Haritoglou C, Kook D, Neubauer A, Wolf A, Priglinger S, Strauss R et al. Intravitreal bevacizumab (Avastin) therapy for persistent diffuse diabetic macular edema. Retina 2006; 26 (9): 999–1005.
Kook D, Wolf A, Kreutzer T, Neubauer A, Strauss R, Ulbig M et al. Long-term effect of intravitreal bevacizumab (avastin) in patients with chronic diffuse diabetic macular edema. Retina 2008; 28 (8): 1053–1060.
Arevalo JF, Fromow-Guerra J, Quiroz-Mercado H, Sanchez JG, Wu L, Maia M et al. Primary intravitreal bevacizumab (Avastin) for diabetic macular edema: results from the Pan-American Collaborative Retina Study Group at 6-month follow-up. Ophthalmology 2007; 114 (4): 743–750.
Aiello LP, Brucker AJ, Chang S, Cunningham Jr ET, D’Amico DJ, Flynn Jr HW et al. Evolving guidelines for intravitreous injections. Retina 2004; 24 (5 Suppl): S3–19.
Soheilian M, Ramezani A, Bijanzadeh B, Yaseri M, Ahmadieh H, Dehghan MH et al. Intravitreal bevacizumab (avastin) injection alone or combined with triamcinolone versus macular photocoagulation as primary treatment of diabetic macular edema. Retina 2007; 27 (9): 1187–1195.
Soheilian M, Ramezani A, Obudi A, Bijanzadeh B, Salehipour M, Yaseri M et al. Randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus macular photocoagulation in diabetic macular edema. Ophthalmology 2009; 116 (6): 1142–1150.
Rensch F, Spandau UH, Wickenhauser A, Jonas JB . Diffuse diabetic macular oedema treated with intravitreal bevacizumab or triamcinolone acetonide. Acta Ophthalmol 2009. [Epub ahead of print 6 February 2009].
Shimura M, Nakazawa T, Yasuda K, Shiono T, Iida T, Sakamoto T et al. Comparative therapy evaluation of intravitreal bevacizumab and triamcinolone acetonide on persistent diffuse diabetic macular edema. Am J Ophthalmol 2008; 145 (5): 854–861.
Paccola L, Costa RA, Folgosa MS, Barbosa JC, Scott IU, Jorge R . Intravitreal triamcinolone versus bevacizumab for treatment of refractory diabetic macular oedema (IBEME study). Br J Ophthalmol 2008; 92 (1): 76–80.
Ahmadieh H, Ramezani A, Shoeibi N, Bijanzadeh B, Tabatabaei A, Azarmina M et al. Intravitreal bevacizumab with or without triamcinolone for refractory diabetic macular edema; a placebo-controlled, randomized clinical trial. Graefes Arch Clin Exp Ophthalmol 2008; 246 (4): 483–489.
Browning DJ, Glassman AR, Aiello LP, Beck RW, Brown DM, Fong DS et al. Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology 2007; 114 (3): 525–536.
Scott IU, Edwards AR, Beck RW, Bressler NM, Chan CK, Elman MJ et al. A phase II randomized clinical trial of intravitreal bevacizumab for diabetic macular edema. Ophthalmology 2007; 114 (10): 1860–1867.
Gillies MC, Simpson JM, Luo W, Penfold P, Hunyor AB, Chua W et al. A randomized clinical trial of a single dose of intravitreal triamcinolone acetonide for neovascular age-related macular degeneration: one-year results. Arch Ophthalmol 2003; 121 (5): 667–673.
Jonas JB, Degenring RF, Kamppeter BA, Kreissig I, Akkoyun I . Duration of the effect of intravitreal triamcinolone acetonide as treatment for diffuse diabetic macular edema. Am J Ophthalmol 2004; 138 (1): 158–160.
Jonas JB, Spandau UH, Kamppeter BA, Vossmerbaeumer U, Harder B, Sauder G . Repeated intravitreal high-dosage injections of triamcinolone acetonide for diffuse diabetic macular edema. Ophthalmology 2006; 113 (5): 800–804.
Avitabile T, Longo A, Reibaldi A . Intravitreal triamcinolone compared with macular laser grid photocoagulation for the treatment of cystoid macular edema. Am J Ophthalmol 2005; 140 (4): 695–702.
Lam DS, Chan CK, Mohamed S, Lai TY, Lee VY, Liu DT et al. Intravitreal triamcinolone plus sequential grid laser versus triamcinolone or laser alone for treating diabetic macular edema: six-month outcomes. Ophthalmology 2007; 114 (12): 2162–2167.
Kang SW, Sa HS, Cho HY, Kim JI . Macular grid photocoagulation after intravitreal triamcinolone acetonide for diffuse diabetic macular edema. Arch Ophthalmol 2006; 124 (5): 653–658.
Noma H, Funatsu H, Yamasaki M, Tsukamo H, Mimura T, Sone T et al. Aqueous humour levels of cytokines are correlated to vitreous levels and severity of macular oedema in branch retinal vein occlusion. Eye 2008; 22 (1): 42–48.
Butcher JM, Austin M, McGalliard J, Bourke RD . Bilateral cataracts and glaucoma induced by long term use of steroid eye drops. BMJ 1994; 309 (6946): 43.
Armaly MF . Statistical Attributes of the Steroid Hypertensive Response in the Clinically Normal Eye. I. The Demonstration of Three Levels of Response. Invest Ophthalmol 1965; 4: 187–197.
Ip MS, Scott IU, VanVeldhuisen PC, Oden NL, Blodi BA, Fisher M et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with observation to treat vision loss associated with macular edema secondary to central retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 5. Arch Ophthalmol 2009; 1279: 1101–1114.
Beck RW, Edwards AR, Aiello LP, Bressler NM, Ferris F, Glassman AR et al. Diabetic Retinopathy Clinical Research Network (DRC.Rnet). Three-year follow-up of a randomized trial comparing focal/grid photocoagulation and intravitreal triamcinolone for diabetic macular edema. Arch Ophthalmol 2009; 127: 245–251.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Forte, R., Cennamo, G., Finelli, M. et al. Intravitreal bevacizumab vs intravitreal triamcinolone combined with macular laser grid for diffuse diabetic macular oedema. Eye 24, 1325–1330 (2010). https://doi.org/10.1038/eye.2010.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.23