Abstract
Background/objectives:
We aimed to quantify the association of sarcopenia with length of hospital stay (LOS) and to identify factors associated with sarcopenia among hospitalized patients.
Subjects/methods:
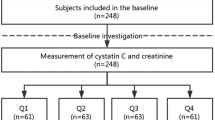
A total of 655 patients composed the study sample. A longitudinal study was conducted in a University Hospital. Sarcopenia was defined, according to European Consensus criteria, as low muscle mass (bioelectrical impedance analysis) and low muscle function (handgrip strength). Logistic regression, Kaplan–Meier and Cox adjusted proportional hazards methods were used. LOS was determined from the date of hospital admission and discharge home (event of interest).
Results:
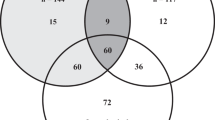
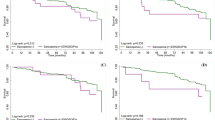
Participants were aged 18 to 90 years (24.3% sarcopenic). Factors associated with sarcopenia were male gender, age ⩾65 years, moderate or severe dependence, undernutrition and being admitted to a medical ward. Sarcopenic patients presented a lower probability of being discharged home (hazard ratio (HR), 95% confidence interval (CI)=0.71, 0.58–0.86). However, after stratifying for age groups, this effect was visible only in patients aged <65 years (HR, 95% CI= 0.66, 0.51–0.86). Moreover, sarcopenic overweight or obese patients presented a higher probability of being discharged home (HR, 95% CI=0.78, 0.61–0.99) than nonoverweight sarcopenic patients (HR, 95% CI=0.63, 0.48–0.83).
Conclusions:
Being male, age ⩾65 years, presenting dependence, being undernourished and admitted to a medical ward were factors associated with sarcopenia among hospitalized adult patients. Sarcopenia is independently associated with longer LOS, although this association is stronger for patients aged <65 years. Moreover, sarcopenic overweight was associated with a higher probability of discharge home than nonoverweight sarcopenia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Ageing 2010; 39: 412–423.
Landi F, Liperoti R, Russo A, Giovannini S, Tosato M, Capoluongo E et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr 2012; 31: 652–658.
Abellan van Kan G . Epidemiology and consequences of sarcopenia. J Nutr Health Aging 2009; 13: 708–712.
Volpato S, Bianchi L, Cherubini A, Landi F, Maggio M, Savino E et al. Prevalence and clinical correlates of sarcopenia in community-dwelling older people: application of the EWGSOP definition and diagnostic algorithm. J Gerontol A Biol Sci Med Sci 2014; 69: 438–446.
Cherin P, Voronska E, Fraoucene N, de Jaeger C . Prevalence of sarcopenia among healthy ambulatory subjects: the sarcopenia begins from 45 years. Aging Clin Exp Res 2014; 26: 137–146.
Gariballa S, Alessa A . Sarcopenia: prevalence and prognostic significance in hospitalized patients. Clin Nutr 2013; 32: 772–776.
Smoliner C, Sieber CC, Wirth R . Prevalence of sarcopenia in geriatric hospitalized patients. J Am Med Dir Assoc 2014; 15: 267–272.
Cerri AP, Bellelli G, Mazzone A, Pittella F, Landi F, Zambon A et al. Sarcopenia and malnutrition in acutely ill hospitalized elderly: prevalence and outcomes. Clin Nutr 2014; 34: 745–751.
Sousa AS, Guerra RS, Fonseca I, Pichel F, Amaral TF . Sarcopenia among hospitalized patients - a cross-sectional study. Clin Nutr 2015; 34: 1239–1244.
Rossi AP, Fantin F, Micciolo R, Bertocchi M, Bertassello P, Zanandrea V et al. Identifying sarcopenia in acute care setting patients. J Am Med Dir Assoc 2014; 15: 303 e7–303 12.
Vetrano DL, Landi F, Volpato S, Corsonello A, Meloni E, Bernabei R et al. Association of sarcopenia with short- and long-term mortality in older adults admitted to acute care wards: results from the CRIME study. J Gerontol A Biol Sci Med Sci 2014; 69: 1154–1161.
Kyle UG, Genton L, Pichard C . Hospital length of stay and nutritional status. Curr Opin Clin Nutr Metab Care 2005; 8: 397–402.
Omachonu VK, Suthummanon S, Akcin M, Asfour S . Predicting length of stay for Medicare patients at a teaching hospital. Health Serv Manage Res 2004; 17: 1–12.
ASPEN Board of Directors and the Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. J Parenter Enteral Nutr 2002; 26: 1SA–138SA.
Hodkinson HM . Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 1972; 1: 233–238.
Katz S . Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc 1983; 31: 721–727.
Charlson ME, Pompei P, Ales KL, MacKenzie CR . A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383.
Ottery F . Patient-generated subjective global assessment. In: Polisena PMC (ed). The Clinical Guide to Oncology Nutrition. The American Dietetic Association: Chicago, IL, USA, 2000, pp 11–23.
Marfell-Jones MOT, Stewart A, Carter L . International Standards for Anthropometric Assessement. ISAK: Potchefstroom, South Africa, 2006.
Pederson D, Gore C . Anthropometry Measurement Error. University of New South Wales Press: Sydney, Australia, 1996.
WHO Expert Committee on Physical Status. Physical status: the use and interpretation of anthropometry, Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995; 854: 1–452.
Janssen I, Heymsfield SB, Baumgartner RN, Ross R . Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol (1985) 2000; 89: 465–471.
Fess E . Grip Strength, 2nd edn. American Society of Hand Therapists: Chicago, 1992.
Vaz M, Thangam S, Prabhu A, Shetty PS . Maximal voluntary contraction as a functional indicator of adult chronic undernutrition. Br J Nutr 1996; 76: 9–15.
Matos L, Teixeira MA, Henriques A, Tavares MM, Alvares L, Antunes A et al. [Nutritional status recording in hospitalized patient notes]. Acta Med Port 2007; 20: 503–510.
Hillman TE, Nunes QM, Hornby ST, Stanga Z, Neal KR, Rowlands BJ et al. A practical posture for hand grip dynamometry in the clinical setting. Clin Nutr 2005; 24: 224–228.
Acknowledgements
We thank Centro Hospitalar do Porto and all ward directors for facilitating the data collection. RSG received a scholarship from Fundação para a Ciência e a Tecnologia, financing program POPH/FSE, under the project SFRH/BD/61656/2009.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sousa, A., Guerra, R., Fonseca, I. et al. Sarcopenia and length of hospital stay. Eur J Clin Nutr 70, 595–601 (2016). https://doi.org/10.1038/ejcn.2015.207
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.207
This article is cited by
-
The association between sedentary behaviour and sarcopenia in older adults: a systematic review and meta-analysis
BMC Geriatrics (2023)
-
A Critical Review of Current Worldwide Definitions of Sarcopenia
Calcified Tissue International (2023)
-
CT-derived measures of muscle quantity and quality predict poorer outcomes from elective colorectal surgery: a UK multicentre retrospective cohort study
Techniques in Coloproctology (2023)
-
Screening, Diagnosis and Management of Sarcopenia and Frailty in Hospitalized Older Adults: Recommendations from the Australian and New Zealand Society for Sarcopenia and Frailty Research (ANZSSFR) Expert Working Group
The Journal of nutrition, health and aging (2022)
-
Force-time curve features of handgrip strength in fibromyalgia syndrome
Scientific Reports (2020)