Abstract
Aggregatibacter (Actinobacillus) actinomycetemcomitans is a facultative anaerobic gram-negative bacterium associated with severe forms of periodontitis. A leukotoxin, which belongs to the repeats-in-toxin family, is believed to be one of its virulence factors and to have an important role in the bacterium's pathogenicity. This toxin selectively kills human leukocytes by inducing apoptosis and lysis. Here, we report that leukotoxin-induced cell death of macrophages proceeded through a process that differs from the classical characteristics of apoptosis and necrosis. A. actinomycetemcomitans leukotoxin-induced several cellular and molecular mechanisms in human macrophages that led to a specific and excessive pro-inflammatory response with particular secretion of both interleukin (IL)-1β and IL-18. In addition, this pro-inflammatory cell death was inhibited by oxidized ATP, which indicates involvement of the purinergic receptor P2X7 in this process. This novel virulence mechanism of the leukotoxin may have an important role in the pathogenic potential of this bacterium and can be a target for future therapeutic agents.
Similar content being viewed by others
Main
Aggregatibacter actinomycetemcomitans is a facultative anaerobic gram-negative bacterium that is mainly associated with severe forms of periodontitis, mankind's most common chronic inflammatory disease.1, 2, 3 There is evidence for a correlation between loss of attachment of the periodontal tissue and high proportion of A. actinomycetemcomitans.4 In addition, this bacterium has been responsible for some non-oral infections including endocarditis, bacteremia, pericarditis, septicemia, pneumonia, infectious arthritis, osteomyelitis, synovitis, skin infections, urinary tract infections and various types of abscesses.5 A link between this bacterium and cardiovascular diseases seems to exist since A. actinomycetemcomitans has been detected in atherosclerotic plaque samples.1, 6
A. actinomycetemcomitans possesses several different well-studied virulence factors, among which the leukotoxin is suggested to have an important role in the pathogenicity.6, 7 The leukotoxin of A. actinomycetemcomitans shares considerable molecular homology (35–70%) with toxins of the repeats-in-toxin (RTX) family, which are produced by other gram-negative pathogens, such as Escherichia coli, Actinobacillus pleuropneumoniae, Bordetella pertussis and Mannheimia haemolytica.8 The toxins of the RTX family selectively kill human leukocytes by inducing apoptosis and lysis.9
An intra-species diversity of A. actinomycetemcomitans exists and clones with different leukotoxin-producing abilities have been identified.6 One clone, JP2, has enhanced leukotoxin expression because of a 530-bp deletion in the leukotoxin promoter region, and it is strongly correlated to disease onset in certain populations.10, 11, 12 The leukotoxin is assumed to protect the bacterium from the local defense mechanisms through its capacity to lyse human immune cells.13, 14 However, this cytotoxic effect cannot alone explain the inflammatory responses that cause the destruction of the tooth-supporting tissues.
Macrophages have an important role in various homeostatic, immunological and inflammatory processes. These cells are organ-localized and can render an immediate nonspecific defense against foreign elements before immigration of other leukocytes. Macrophages release cytokines, are the main source of interleukin 1β (IL-1β) in the inflamed tissue, and contribute to the specific immunity through antigen presentation.15, 16 IL-1β is produced as a biologically inactive precursor, pro-IL-1β, and needs to be cleaved by a specific enzyme, caspase-1, for activation and secretion.15 This enzyme can be activated in response to various pore-forming toxins and extra cellular ATP.17 Human monocytes/macrophages are highly sensitive to the A. actinomycetemcomitans leukotoxin. In contrast to other subsets of leukocytes, the monocytes/macrophages are lysed by a mechanism that involves activation of caspase-1 and secretion of bio-active IL-1β.18, 19 This response is mediated by leukotoxin or live wild-type A. actinomycetemcomitans. As the response is completely abolished in the presence of bacteria from a leukotoxin knockout strain, the induced IL-1β secretion from these cells appears mainly to be caused by the leukotoxin.20 These findings resembles a recently discovered death mechanism termed pyroptosis, which is characterized as a caspase-1-dependent programmed cell death leading specifically to IL-1β and IL-18 secretion.21 Pyroptosis was first described for Salmonella-infected macrophages.22
In this study, we describe new features of human macrophage cell death induced by A. actinomycetemcomitans leukotoxin that that can be linked to pathogenic mechanisms of inflammatory-related diseases.
Results
Cell survival and cell death of macrophages exposed to leukotoxin
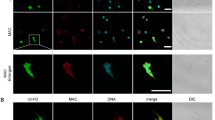
The lactate dehydrogenase (LDH) leakage from human macrophages exposed to various concentrations of A. actinomycetemcomitans leukotoxin for 60 min indicated that a dose-dependent disruption of the membrane integrity occurred when leukotoxin concentrations were ≥1 ng/ml (Figure 1a). The uptake of early apoptotic (Yo-PRO-1) and necrotic/late apoptotic (propidium iodide, PI) markers in macrophages exposed to 1 or 10 ng/ml of leukotoxin (60 min) showed a similar pattern for both markers (Figure 1b). The morphology of the macrophages exposed to these concentrations of leukotoxin for 60 min was further analyzed by transmission electron microscopy (TEM) (Figure 1c). The proportion of normal cells (Figure 1c-i) decreased, while the proportions of necrotic cells (Figures 1c-II and c-IV) and apoptotic cells (Figures 1c-III and c-V) increased. Leukotoxin caused an activation and secretion of IL-18 and IL-1β from the affected macrophages (Figures 2d and e). Taken together, these results indicated that there existed a threshold level for leukotoxin sensitivity in each cell and that each of the affected cells activated signaling pathways that eventually led to cell death.
Analysis of cell survival, cell death, IL-18 and IL-1β secretion from human macrophages exposed to A. actinomycetemcomitans leukotoxin (Ltx) for 0–60 min. (a) Extracellular release of LDH, indicative of cell lysis, from human macrophages exposed to various concentrations of Ltx for 60 min. Mean values±S.D. of three experiments with different macrophage donors. (b) Flow cytometric analyses of uptake of YO-PRO-1 (early apoptosis marker) and PI (late apoptosis/early necrosis marker) in macrophages after Ltx exposure. Mean values±S.D. of macrophages from three experiments with MNLs obtained from different donors. (c) TEM analyses of macrophages exposed to various concentrations of Ltx (magnification of × 3700). Mean values±S.D. of cells with typically normal, necrotic or apoptotic morphology from measurements of four equally large fields on every grid with the following total number of cells in each group: 0 (n=122 cells), 1 (n=82 cells) and 10 (n=79 cells). A representative cell from each of these morphological categories is shown: normal (c-I), necrotic (c-II and c-IV) and apoptotic (c-III and c-V). ELISA quantification of the secreted and cell-associated IL-18 from human macrophages exposed to 10 ng/ml Ltx for 0–60 min. Mean values from three experiments with one macrophage donor. ELISA quantification of secreted IL-18 (d) and IL-1β (e) from human macrophages exposed to 10 ng/ml Ltx for 60 min. Mean values±S.D. from eight experiments with different macrophage donors. P-values: 0.03 (*) and 0.0003 (**) (two-tailed t-test, SPSS software) are indicated
Effects of A. actinomycetemcomitans leukotoxin (Ltx) on human macrophage IL-1β production and secretion. (a) ELISA quantification of the cell-associated and secreted IL-1β from macrophages exposed to 10 ng/ml A. actinomycetemcomitans Ltx or 100 ng/ml E. coli LPS (LPS) for 180 min. Mean values±S.D. of seven experiments with macrophages obtained from different donors. (b) Real-time RT-PCR quantification of mRNA of IL-1β in macrophages exposed to Ltx (10 ng/ml) or LPS (100 ng/ml) for 60 min in relation to the endogenous control GAPDH. Mean values±S.D. of three experiments from one macrophage donor. (c) Levels of mRNA for IL-1β in relation to the endogenous control GAPDH quantified by real time RT-PCR in macrophages exposed to Ltx (0–60 min) or LPS (60 min). Mean values±S.D. from three experiments from one macrophage donor. (d) ELISA quantification of IL-1β secreted from macrophages exposed to Ltx (0–60 min) or LPS (60 min). Mean values±S.D. from three experiments from one macrophage donor. (e) ELISA quantification of the cell-associated and secreted amounts of pro-IL-1β and IL-1β of macrophages exposed for 60 min to 10 ng/ml Ltx or 10 ng/ml heat-inactivated (HI) Ltx (pretreated at 70 °C for 30 min). Mean values±S.D. from three experiments from one macrophage donor. (f) Western blot analyses of cell lysates (Pellet) and supernatants (Sup) of macrophages exposed to 10 ng/ml Ltx or 100 ng/ml LPS for 60 min. GAPDH was used as endogenous control. Recombinant human IL-1β (rh IL1β, left lower band) was used for verification of the position of the 17 kDa IL-1β (active form). Representative results from two experiments with different macrophage donors are shown
Effects of leukotoxin on macrophage IL-1β production and secretion
The amounts of total active IL-1β (cell associated and secreted), detectable by enzyme-linked immunosorbent assay (ELISA), from macrophages exposed to 10 ng/ml of A. actinomycetemcomitans leukotoxin or to 100 ng/ml of E. coli lipopolysaccharide (LPS) for 180 min are shown (Figure 2a). Cultures of macrophages exposed for 60 min to A. actinomycetemcomitans leukotoxin (10 ng/ml) showed a 10-fold increase in total IL-1β protein as compared with cultures without stimulus and a 6-fold increase as compared with cultures exposed to E. coli LPS (100 ng/ml) (Figure 2a). To study whether this excessive secretion could be due to higher production of IL-1β, the mRNA level for this cytokine in macrophages was studied by quantitative real-time RT-PCR. The IL-1β mRNA level in the macrophages exposed to leukotoxin for 60 min was negligibly increased as compared with the control cells, while exposure to LPS (100 ng/ml) led to approximately 30 times higher levels of IL-1β mRNA (Figure 2b). Time-course experiments aimed to study the mRNA levels of IL-1β showed no sign of any marked increase because of the leukotoxin exposure (Figure 2c). On the other hand, the time course of the secreted active protein showed that already after 20 min of leukotoxin exposure (10 ng/ml) a substantial amount of IL-1β was secreted and reached its maximum after 40 min (Figure 2d). The enhancement caused by the LPS (100 ng/ml) after 60-min exposure was negligible as compared with that caused by the leukotoxin (Figure 2d). All the mRNA levels for IL-1β were calculated in relation to the mRNA levels of an endogenous control, glyceraldehyde-3-phosphate dehydrogenase (GAPDH). To verify the stability of GAPDH mRNA in the leukotoxin-exposed macrophages, the mRNA levels of another endogenous control, ribosomal protein L13A (RPL13A), were also quantified. The resulting changes in the IL-1β mRNA levels because of exposure to leukotoxin or LPS were similar regardless of the selection of the endogenous controls tested (data not shown).
Leukotoxin exposure (10 ng/ml) of macrophages for 60 min decreased the cell-associated pro-IL-1β and increased the secretion of pro-IL-1β (Figure 2e). In addition, the secreted IL-1β was substantially increased by leukotoxin. Heat inactivation of leukotoxin completely abolished its ability to cause secretion of the pro-form, as well as the active IL-1β. Heat inactivation of the leukotoxin completely abolished its ability to induce IL-1β secretion and the leukotoxin did not affect the pro-IL-β production, neither the native nor the heat inactivated, which indicates no effect from non-proteinaceous contaminants (i.e., LPS). The total level of cell-associated and secreted IL-1β (pro- and active forms, taken together) from macrophages exposed to leukotoxin (10 ng/ml) for 60 min, increased two times as compared with the unchallenged cells (Figure 2e). Western blot analyses of macrophage cultures exposed to leukotoxin (10 ng/ml) or LPS (100 ng/ml) for 60 min, confirmed that leukotoxin exposure caused secretion of the active form of IL-1β, while LPS exposure mainly increased the cell-associated pro-IL-1β (Figure 2f). A similar effect could be shown already after 20 min of leukotoxin (10 ng/ml) exposure (data not shown).
Caspase-1 and p38 inhibition, and their effects on A. actinomycetemcomitans leukotoxin-induced activation of human macrophages
Western blot analyses of cell lysates from macrophages showed that exposure to leukotoxin (1 or 10 ng/ml) or LPS (100 ng/ml) for 15- or 30-min activated phosphorylation of mitogen-activated protein kinase (MAPK) p38 and the total levels of inhibitor of NF-κBα (IκBα) were not affected by the leukotoxin (data not shown). Time-course registration of p38 phosphorylation in macrophages by fluorescence-activated cell sorting (FACS) showed a more rapid effect by the leukotoxin than by the LPS (data not shown). Macrophages exposed to 10 ng/ml leukotoxin for 5 min showed a 10-fold increase in phosphorylated p38 as compared with the unchallenged control cells, while the levels of phosphorylated nuclear factor κB (p65) (NF-κB (p65)) in these cells were not affected (Figure 3a). To investigate the involvement of p38 and caspase-1 in the leukotoxin-induced cell lysis and IL-1β secretion from macrophages, the experiments were conducted in the presence of selective inhibitors. Neither of the two inhibitors used for p38 (SB 203580 or SKF-86002) affected the leukotoxin-induced cell lysis or IL-1β secretion (Figures 3b and c). In contrast, both selective inhibitors for caspase-1 (Ac-YVAD-CMK or Z-VAD-FMK) reduced the leukotoxin-induced lysis of macrophages to some extent (Figure 3b) and the leukotoxin-induced IL-1β secretion to levels similar to those found in unchallenged cells (Figure 3c). The combination of inhibitors for caspase-1 (Ac-YVAD-CMK) and p38 (SB 203580) had no additive inhibitory effect (Figures 3b and c). The presence of a p38 inhibitor (SB 203580) did not interfere with the secretion of any of the tested cytokines (IL-1β, tumor necrosis factor (TNF)-α and interleukin-6 (IL-6)) from leukotoxin-challenged macrophages, while this inhibitor (SB 203580) decreased the E. coli LPS-induced cytokine secretion (data not shown).
Caspase-1 and p38 inhibition, their effects on A. actinomycetemcomitans leukotoxin-induced lysis and IL-1β secretion from human macrophages. (a) Flow cytometric analysis of p38 and NF-κB (p65) phosphorylation in human macrophages exposed to 10 ng/ml Ltx for 5 min as compared with control cells. Mean values±S.D. of three experiments from macrophages obtained from different donors. (b) Extracellular release of LDH and (c) ELISA quantification of IL-1β secretion of human macrophages exposed to 0, 3 or 10 ng/ml leukotoxin for 60 min. The experiments were conducted without or with selective inhibitors: for p38 (SB 203580 or SKF-8600, 10 μM) or caspase-1 (Ac-YVAD-CMK or Z-VAD-FMK, 100 μM). Mean values±S.D. of four experiments with different macrophage donors
Role of caspase-1, glycine, calcium, potassium and oxidized adenosine-5′-triphosphate (oATP) in leukotoxin-induced macrophage lysis and IL-1β secretion
The presence of a cytoprotectant (glycine) and the caspase-1 inhibitor (Ac-YVAD-cmk) partially inhibited the leukotoxin-induced lysis of macrophages (Figure 4a). A combination of these inhibitors caused an additive decrease in the leukotoxin-induced macrophage lysis (Figure 4a). These results indicated that leukotoxin-induced macrophage lysis involved pore-formation as well as intracellular signaling pathways. The presence of glycine had no effect on the leukotoxin-induced IL-1β secretion from the challenged macrophages (Figure 4b). Depletion of extracellular calcium inhibited the IL-1β secretion caused by the leukotoxin, while the degree of cell lysis remained unchanged (Figure 4c). A similar effect was seen in samples with enhanced extracellular potassium (Figure 4c) that limits the ability of the cell to release intracellular potassium. Presence of oATP inhibited both leukotoxin-induced cell lysis (Figure 4d) and IL-1β secretion (Figure 4e) from macrophages. The cell-associated levels of IL-1β were not affected by the oATP (Figure 4e).
Role of caspase-1, glycine, calcium, potassium and oATP in leukotoxin-induced macrophage lysis and IL-1β secretion. Extracellular release of LDH (a) and ELISA (b) quantification of IL-1β secretion from human macrophages exposed to 0 or 10 ng/ml of leukotoxin for 60 min. The experiments conducted without or with caspase-1 inhibitor (Ac-YVAD-CMK, 100 μM) and/or a cytoprotectant (glycine, 5 mM). (c) Experiments conducted in different buffers: physiological, without calcium or with enhanced potassium concentration. Mean values±S.D. from three experiments with different macrophage doors. (d and e) Extracellular release of LDH (d) and ELISA (e) quantification of IL-1β secretion from human macrophages exposed to 0 or 10 ng/ml of leukotoxin for 60 min. The experiments conducted without or with oATP (500 μM) added 30 min previous the toxin exposure. Mean values±S.D. from three experiments with different macrophage donors
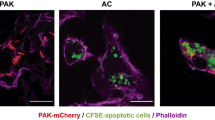
Effects of oATP on leukotoxin-exposed MNL
Analysis of MNL structure (forward scatter (FSC)–side scatter (SSC)) examined by FACS showed a time-dependant selective depletion of the macrophage population (with high FSC/SSC) caused by the leukotoxin (10 ng/ml) that was blocked in presence of oATP (Figure 5a). Leukotoxin (10 ng/ml) caused also an enhanced FSC after 10 min exposure, which was not affected by the added oATP (Figure 5b). The PI-uptake analysis by FACS showed that leukotoxin (10 ng/ml) caused a time-dependant cell death of MNL that was inhibited by oATP (Figure 5c).
Effects of oATP on leukotoxin-exposed MNL. The cell morphology (FSC/SSC) and viability (PI-uptake) of leukotoxin-exposed MNL were analyzed by FACS. MNL were exposed to 10 ng/ml leukotoxin with and without oATP (500μM) for up to 60 min. (a) Distribution of FSC/SSC in MNL during leukotoxin exposure. (b) Histogram of FSC of the exposed MNL (Co=0 min exposure, Ltx=10 min exposure). Mean FCS of the MNL population are indicated (c) PI-uptake in MNL during leukotoxin-exposure. Mean values of PI-positive cells are indicated. All the figures show representative results from three experiments with different macrophage donors. Mean values±S.D. are shown
P2X7 receptor expression and ATP release of MNL
The two different populations, R1 and R2, in the MNL-suspension were gated (Figure 6a) and the composition of leukocytes subsets (CD14+, CD3+ and CD19+) and P2X7R expression was documented by specific antibodies analyzed by FACS (Figure 6b). The majority of the P2X7R+ cells were found in the R1-population, which also consisted of mainly CD14+ cells, while the R2-population primarily was CD3+ cells without P2X7R-expression (Figures 6b and c). The high leukotoxin-sensitivity of the R1-population was further indicated by PI-staining examined by FACS. The leukotoxin-exposed (10 ng/ml) MNL showed a time-dependent decrease in living cells for the R1-population, but less pronounced for the R2-population (Figure 6d). Presence of oATP inhibited the leukotoxin-induced decrease in viable MNL (Figure 6d). Further, luminescence analysis of ATP-release from the macrophages showed a rapid extracellular ATP release induced by the leukotoxin (1 and 10 ng/ml) (Figure 6e).
P2X7 receptor expression and ATP release of MNL. (a–c) show unchallenged MNL examined by FACS and (d and e) show leukotoxin-exposed MNL. (a) Population identification (R1 and R2) of MNL based on FCS/SSC characteristics. A representative dot-plot is shown. (b) Distribution of cells with different surface markers in the two gated populations (R1 and R2). Mean values±S.D. from three different MNL donors are shown. (c) Illustration of P2X7R expression in R1 and R2 by representative histograms. (d) Number of viable cells (PI-negative) in the two different MNL populations (R1 and R2) analyzed by FACS during leukotoxin exposure (10 ng/ml) with and without oATP (500 μM). (e) ATP-release from the macrophages exposed to the leukotoxin (1 and 10 ng/ml)
Discussion
This report shows new features of leukotoxin-induced cell death of human macrophages that involves pro-inflammatory stimulation. This newly discovered death mechanism resembles the caspase-1-dependent programmed cell death designated pyroptosis.21, 22 Although major cell damage to the macrophages was initiated by leukotoxin (≤10 ng/ml), these cells were able to activate and secrete excessive amounts of IL-1β during the death process. In relation to cells exposed to E. coli LPS (one of the most widely used inducers of IL-1β production and secretion), the leukotoxin-challenged cells were able to induce >10-fold higher secretion of the active IL-1β after a short exposure time (60 min). This activation by the leukotoxin was mainly mediated by caspase-1 activation and was not correlated to any changes in the mRNA levels for IL-1β. The leukotoxin-induced IL-18 secretion seemed to follow the same pattern as for IL-1β. This is reasonable since both cytokines require caspase-1 activation for their activation and secretion. However, the leukotoxin-induced secretion of IL-1β from macrophages was 30 times higher than the IL-18 secretion.
The results of this study indicate an irreversible loss of cell membrane integrity of macrophages exposed to ≥1 ng/ml leukotoxin, with a dose-dependent increase in affected cells correlated to the concentration of leukotoxin. The different cellular markers for both apoptosis and necrosis followed a similar pattern of dose dependency and indicated a heterogenic cell population with regard to leukotoxin sensitivity. TEM confirmed the presence of both apoptotic and necrotic cells in the macrophage populations exposed to the leukotoxin. The similar morphology of the affected cells exposed to different concentrations of leukotoxin indicated a threshold level for leukotoxin sensitivity for each cell subset. Each of the affected cells activated signaling pathways that finally ended up in cell death. An increase in leukotoxin enhanced the proportion of affected cells. Moreover, the additive inhibitory effect of a cytoprotectant (glycine) and a caspase-1 inhibitor on leukotoxin-induced macrophage lysis indicated that this process involved both pore-formation and activation of intracellular signaling pathways. In addition, our results showed that the leukotoxin-induced IL-1β secretion was modified by blockage of calcium influx or potassium efflux. These modifications did not affect the leukotoxin-induced cell lysis, which indicates that this cell lysis is independent of IL-1β secretion.
Several bacterial products, such as LPS, are known to increase expression of pro-IL-1β in macrophages.16 However, a secondary stimulus is needed to induce a substantial secretion of the bioactive IL-1β. It has been shown that this activation can be induced by various bacterial species through activation of the inflammasome (intracellular signal-induced multiprotein complex) that leads to caspase-1 activation and IL-1β secretion.23 This secondary activation can be induced by direct interactions of bacteria–bacterial compounds with the inflammasome, such as proteins secreted by Salmonella typhimurium23 or Francisella tularensis invasion.24 The other system for stimulating this secondary activation has been described through cell surface interactions as for Listeria monocytogenes and Staphylococcus aureus.23 The physiological properties of the leukotoxin as a large protein that involves interaction with a target cell receptor, the CD18 subunit of the β2-integrin,25 indicates that this toxin also acts through surface interactions.
Exposure of macrophages to leukotoxin also caused an increase in the total IL-β protein in the macrophage cultures (both cell-associated and secreted pro-IL-1β and IL-1β). In other words, leukotoxin seemed to make more pro-IL-1β available for activation than what normally exists in the cells, and the toxin also acted as the secondary stimulus needed for activation and secretion of IL-1β. Interestingly, we did not find any marked leukotoxin-induced production of IL-1β at the mRNA level that could explain this increase in IL-1β protein. The mechanism behind this phenomenon is not fully understood. However, it might involve post-transcriptional changes of the pro-IL-1β synthesis initiated by the leukotoxin-induced cell stress. It has been proposed that significant changes in translational efficiency occur for IL-1β mRNA, because there is a lack of correlation between IL-1β mRNA and protein levels.26 Leukotoxin-exposed macrophages showed a rapid increase in phosphorylated p38, but this activation was not correlated to cell lysis or IL-1β activation and secretion. Moreover, the lack of activation of NF-κB p65 (Ser536), IκBα and mRNA levels for IL-1β in leukotoxin-challenged macrophages indicated that the toxin mainly acted at a post-transcriptional level. These findings are in contrast to the LPS-induced pathways where p38-activation is involved in the production of IL-1β. In addition, LPS-induced IκBα phosphorylation and degradation allows translocation of NF-κB to the nucleus, which can induce pro-inflammatory cytokine production, including IL-1β.27, 28
The macrophages were sensitive targets for the leukotoxin and this cell population consists of mainly CD14-positive cells expressing P2X7R. This cell population responds to the leukotoxin with a rapid extracellular release of ATP and an increased cell volume (FSC). Prolonged leukotoxin exposure caused pore formation and cell death confirmed by increased uptake of nucleic acid dyes (YO-PRO1 and PI) followed by a complete collapse of the cells in this population. Addition of the P2X7R antagonist oATP inhibited the leukotoxin-induced cell death of the CD14+ population, which indicates involvement of P2X7R signaling in the leukotoxin-induced pro-inflammatory monocyte/macrophage death. Prolonged activation of the P2X7R by extracellular ATP have been shown to open up pores in the cell membrane that allows an uncontrolled ion exchange ending up in a similar pro-inflammatory cell death.17 The P2X7-R-dependent caspase-1 activation and IL-1β release in human monocytes/macrophages has been further evaluated in a recent publication.29
In conclusion, this report shows that leukotoxin activates a pro-inflammatory response in human macrophages leading to excessive and specific secretion of both IL-1β and IL-18. In addition, we show for the first time that this pro-inflammatory cell death was inhibited by oATP, which indicates involvement of the purinergic receptor P2X7 in this process.29 This novel virulence mechanism of the leukotoxin may have an important role in the pathogenic potential of this bacterium and can be a target for future therapeutic agents.30, 31 The specific mechanisms of purigenic receptor for A. actinomycetemcomitans pathogenicity need further investigations.
Materials and Methods
Ethics
The blood was taken from donors visiting the University Hospital blood bank in Umeå, Sweden. Informed written approval was given by all subjects, and authorization for the study was granted by the Human Studies Ethical Committee of Umeå University, Sweden (§67/3, dnr 03-019).
Leukotoxin and leukocyte preparations
Leukotoxin was purified from A. actinomycetemcomitans strain HK 1519 (JP2 clone), described in detail previously.32 The purified leukotoxin was basically free from LPS (<0.001% of total protein).
Human leukocytes were isolated from an enriched leukocyte fraction (buffy coat) of venous blood (from blood donors at the University Hospital blood bank in Umeå, Sweden), as described previously.19 Mononuclear leukocytes (MNLs) were isolated by isopycnic centrifugation in Lymphoprep (Nycomed AB, Lidingö, Sweden). The fraction containing MNLs was collected and the cells were washed three times with phosphate-buffered saline (PBS) (250 × g, 5 min) to remove platelets. The cell pellet was then re-suspended in culture medium RPMI-1640 containing L-glutamine, 10% fetal bovine serum (FBS), and Penicillin–Streptomycin (Sigma-Aldrich, St. Louis, MO, USA) to yield 5 × 106 cells/ml. This suspension was distributed into 50-mm Petri dishes (NUNC A/S, Roskilde, Denmark) at 15 ml/dish and incubated at 37 °C in 5% CO2 for 2 h to allow the monocytes to adhere. The non-adherent leukocytes were removed by two rinses with 10 ml PBS. The adherent cells were detached from the dish surface with a sterile cell scraper (Corning Incorporated, Corning, NY, USA), washed twice with PBS and re-suspended in culture medium to yield 106 cells/ml. Further, 1 ml of this suspension was distributed to 2 cm2 culture dishes (NUNC) and cultured for 20 h at 37 °C in 5% CO2 to equilibrate the cells. Before experimentation, the culture medium was replaced by fresh medium. The adherent MNLs obtained by this procedure are termed macrophages.19, 20
Cell survival and cell death analysis
Cytolysis
Leukotoxin-induced cytolysis was determined by the release of the cytosol enzyme LDH as described earlier.18 The cells were incubated for 60 min at 37 °C in the presence of various concentrations of leukotoxin. The activity of the enzyme released from damaged cells into the supernatant was measured and expressed as a percentage of the total LDH activity released from cells lysed by exposure to 0.1% Triton X-100 for 60 min. In order to determine the role of calcium influx and potassium efflux, experiments were performed in buffers without calcium or enhanced potassium, in accordance to Moudy et al.33
Yo-PRO-1 and PI uptake quantified by FACS
The macrophages were incubated in culture medium for 60 min, at 37 °C in the presence of 1 or 10 ng/ml A. actinomycetemcomitans leukotoxin. Macrophages in plain culture medium served as controls. These cells were further analyzed for early detection of apoptosis/necrosis. The experiment was ended on ice, and Yo-PRO-1 and PI was added according to the Vybrant Apoptosis Assay Kit #4 protocol (Molecular Probes/Invitrogen Labeling and Detection, Eugene, OR, USA). These dyes were incubated for 30 min, the cells were detached with a sterile cell scraper (Corning Incorporated), transferred to FACS tubes and analyzed by FACS as soon as possible using 488 nm excitation with fluorescence emission at 530 nm (e.g., FL1) and >575 nm (e.g., FL3) (Calibur, Becton Dickinson Immunocytometry Systems, Becton Dickinson, Franklin Lakes, NJ, USA).
Transmission electron microscopy
The macrophages were obtained as described above and were further treated with 1 or 10 ng/ml leukotoxin for 1 h. Macrophages alone were used as a negative control. All samples were fixed with 2.5% glutaraldehyde for at least 30 min at room temperature and then washed in sodium cacodylate buffer and postfixed in 2% osmium tetroxide in the same buffer for 1 h. The samples were centrifuged and the pellets were dehydrated and embedded in Epoxy resin LX-112. The embedded samples were cut into ultra-thin sections, placed on grids and stained with uranyl acetate and lead citrate. Sections were examined with a transmission electron microscope (Philips 420, Fei, Hilsboro, OR, USA). The measurements of four equally large fields on every grid were done to count percentages of normal, apoptotic and necrotic cells in each sample. Distinguishing features for apoptosis were chromatin condensation and DNA fragmentation (karyorrhexis); features of necrosis were plasma membrane disruption and nuclear disintegration as described previously.34
Cytokine quantification
ELISA
The macrophages were exposed to bacterial stimuli as described above. The amounts of IL-1β, IL-6 and TNF-α secreted into the culture medium, or retained intracellularly in the macrophages, were determined by ELISA using DuoSet kits (R&D Systems Inc., Minneapolis, MN, USA). IL-18 was quantified by a kit from Medical & Biological Laboratories Co., Ltd. (Nagoya, Japan). To obtain maximum release of the intracellular cytokines, the cells were lysed with 0.1% Triton X-100 for 60 min. All samples were stored at –80 °C pending analysis. The maximum level of active IL-1β (both secreted and cell associated) in the leukotoxin-challenged macrophages (10 ng/ml) was set at 100 %, while the maximum level of IL-6 and TNF-α were obtained from the E. coli LPS-challenged cells and were set at 100%. To allow discrimination between pro-IL-1β and active IL-1β the Quantikine Kits (R&D Systems Inc.) were used. Specificity tests of the Quantikine Kits showed negligible cross-reactivity of pro-IL-1β with IL-1β and vice versa. For all ELISA kits the procedures were done according to the manufacturer's protocol.
Western blot
Detection of IL-1β in supernatants and cell pellets was also assayed by an immunoblot technique that allows discrimination of the biologically inactive pro-IL-1β (31 kDa) and the active protein (17 kDa).19 Briefly, the proteins in the supernatants and cell pellets were boiled in sample buffer, separated by SDS-PAGE, transferred to a Polyscreen membrane (NEN Life Science Products, Boston, MA, USA) and incubated with polyclonal rabbit anti-human IL-1β antibodies (R&D Systems Inc.), which recognize both pro- and active IL-1β. For endogenous control a polyclonal rabbit anti-human GAPDH (R&D Systems Inc.) was used. As a secondary antibody, horseradish peroxidase-conjugated goat anti-rabbit IgG (Dako, Glostrup, Denmark) was used. Recombinant human IL-1β was used to verify the position of the active IL1β (Sigma-Aldrich). The immunoreactive protein bands were enhanced by chemiluminescence technique (Pierce, Rockford, IL, USA) and visualized using ChemiDoc XRS (BIORAD Laboratories AB, Sundbyberg, Sweden).
Effect on expression of IL-1β mRNA
RNA extraction and cDNA synthesis
Total RNA was extracted from 2 × 106 macrophages per well, from experiments in 12-well plates (NUNC) by the RNAqueous-4PCR kit (Ambion Inc., Austin, TX, USA), according to the manufacturer's protocols. Further, extracted total RNA was treated with DNase I to eliminate genomic DNA. The RNA was quantified by spectrophotometer and used for the complementary deoxyribonucleic acid (cDNA) synthesis; 0.1 μg of total RNA was reverse transcribed into single-stranded cDNA with a 1st Strand cDNA Synthesis Kit (Roche Applied Science, Mannheim, Germany) using AMV reverse transcriptase and oligo-p(dT)15 primers. After incubation at 25 °C for 10 min and at 42 °C for 60 min, the AMV reverse transcriptase was denaturated at 99 °C for 5 min, followed by cooling to +4 °C for 5 min. The cDNA was kept at –20 °C until PCR analysis.
Quantitative real-time reverse transcription polymerase chain reactions (RT-PCRs)
Quantitative real-time RT-PCR analyses were performed using Taqman kinetics with fluorescence labeled probes (reporter fluorescent dye VIC at the 5′ end and quencher fluorescent dye TAMRA at the 3′ end) (Applied Biosystems, Foster City, CA, USA): human GAPDH assay ID Hs00266705_g1, human RPL13A assay ID Hs03043885_g1 and human IL-1β assay ID Hs00174097_m1. In each reaction, cDNA was diluted 20-fold with nuclease-free water and amplified using the TaqMan Universal PCR Master Mix, 300 nM of each primer and 100 nM of probe. The reaction conditions were an initial step of 2 min at 50 °C and 10 min at 95 °C, followed by 40 cycles of denaturation at 95 °C for 15 s and annealing/extension at 60 °C for 1 min. The amplifications were performed using the ABI PRISM 7900 HT Sequence Detections System and software (Applied Biosystems). No amplifications were detected in samples where the RT reaction had been absent. To control for variability in amplification because of differences in starting mRNA concentrations, GAPDH or RPL13A were used as endogenous controls. The relative expressions of IL-1β mRNAs were computed from the IL-1β Ct values and GAPDH or RPL13A Ct values using the standard curve method. Ct values for GAPDH and RPL13A were confirmed not to vary over time or because of treatment.
Effect on p38 MAPK, NF-κB (p65) and IκBα
Specific antibodies were used to test the activation of the MAPK p38, NF-κB and IκBα. Phospho-p38 MAP kinase rabbit pAb (thr180/tyr182) #9211; total p38 MAP kinase rabbit pAb #9212; and phospho-NF-κB p65 (Ser536) (93H1) rabbit mAb (Alexa Fluor 647 Conjugate) #4887 were obtained from Cell Signaling Technology Inc. (Danvers, MA, USA). Rabbit anti-IκBα was obtained from (Santa Cruz Biotechnology, Santa Cruz, CA, USA). All the procedures and dilutions of the antibodies for western blot and FACS analyses were according to the manufacturer's protocol (Cell Signaling Technology Inc.). In western blot analysis, the cell lysates were prepared in accordance with the manufacturer's protocol (Cell Signaling Technology Inc.), and a horseradish peroxidase-conjugated goat anti-rabbit IgG (Dako) was used as a secondary antibody. In FACS analysis, a rabbit IgG, chromatographically purified isotype (Zymed Laboratories Inc., San Francisco, CA, USA) was used as nonspecific negative control. Further, a secondary fluorescein isothiocyanate (FITC) conjugated goat anti-rabbit (Rockland Immunochemicals Inc., Gilbertsville, PA, USA) was used in FACS analysis. After following the recommended step in the manufacture's protocol, the final volumes 0.5 ml with a final concentration of 106 cells per tube, were analyzed by FACS using 488 nm excitation with fluorescence emission at 530 nm (e.g., FL1) (Calibur, Becton Dickinson Immunocytometry Systems).
Inhibition of leukotoxin-induced cell lysis and IL-1β secretion
All inhibitors used in this study were diluted in dimethyl sulphoxide (DMSO) and added to the cell cultures 15 min before leukotoxin or LPS exposure. The final concentrations of DMSO in the cell cultures containing these inhibitors was 0.1%, and in these experiments DMSO (0.1%) was also added to the corresponding control groups (without inhibitor). The inhibitors used were as follows: caspase-1 inhibitors (Ac-YVAD-CMK (C24H33CIN4O8) or Z-VAD-FMK (C22H30FN3O7) (Calbiochem, La Jolla, CA, USA) at a final concentration of 100 μM, p38 MAPK inhibitors (SB 203580 (C21H16N3OSF) or SKF-86002(C16H12FN3S) (Calbiochem) at a final concentration of 10 μM, and Glycine (NH2CH2COOH) at a final concentration of 5 mM (water soluble). In order to determine the role of calcium influx and potassium efflux, experiments were performed in buffers without calcium or enhanced potassium, in accordance to Moudy et al.33 Incubations were also performed in presence of leukotoxin (10 ng/ml) with or without oATP (500 μM) (Sigma-Aldrich) added 30 min previous the toxin.
Cell characterization by FACS and ATP release
Flow cytometric analyzes
MNL were isolated from buffy coat as described washed and resuspended in PBS do a density of 106 cells/ml. The cells were characterized based on their different distribution in light scatter (SSC and FSC) by FACS, (Calibur, Becton Dickinson). The two distinct populations (G1 and G2) were characterized with specific fluorescein (FITC)-conjugated antibodies for expression of cell surface receptors: CD14 (Clone TüK4), CD3 (Clone UCHT1) CD19 (Clone HD37) (all from DakoCytomation, Copenhagen, Denmark) and P2X7 (Rabbit polyclonal) (Alomone Labs, Jerusalem, Israel). Analyzes were performed in accordance to the manufacturer's protocol as described previously (Kelk et al., 2008). Incubations were also performed in presence of leukotoxin (10 ng/ml) with or without oATP (500 μM) (Sigma-Aldrich) added 30 min previous the toxin. To discriminate between viable and dead cells PI (75 μM) (Sigma-Aldrich) was added to the mixtures before analyzes. Twenty thousand cells from each sample were analyzed.
ATP release
Release of ATP was analyzed in culture supernatants with a commercial kit (Chrono-Lume 395) in accordance to the manufacturer's protocol (Chrono-Log Corp., Havertown, PA, USA). Analyzes were performed in EC-buffer and the supernatants immediately transferred to −20 °C and stored frozen until quantification in a luminometer (Becton Dickinson).
Statistical analysis
Mean values and S.D. are shown in the figures and tables. The statistical analyses were done in the SPSS software (IBM, Somers, NY, USA) by using t-test. P-values of <0.05 were considered indicative of statistically significant differences.
Abbreviations
- cDNA:
-
complementary deoxyribonucleic acid
- ELISA:
-
enzyme-linked immunosorbent assay
- FACS:
-
fluorescence-activated cell sorting
- FBS:
-
fetal bovine serum
- FITC:
-
fluorescein isothiocyanate
- GAPDH:
-
glyceraldehyde-3-phosphate dehydrogenase
- IκB:
-
inhibitor of NF-κB
- IL-1β:
-
interleukin-1β
- IL-6:
-
interleukin-6
- LDH:
-
lactate dehydrogenase
- LPS:
-
lipopolysaccharide
- MAPK:
-
mitogen-activated protein kinase
- MNL:
-
mononuclear leukocytes
- NF-κB:
-
nuclear factor κB
- oATP:
-
oxidized adenosine-5′-triphosphate
- PBS:
-
phosphate-buffered saline
- PCR:
-
polymerase chain reaction
- RPL13A:
-
ribosomal protein L13A
- RTX:
-
repeats-in-toxin
- TEM:
-
transmission electron microscopy
- TNF-α:
-
tumor necrosis factor-α
References
Pihlstrom BL, Michalowicz BS, Johnson NW . Periodontal diseases. Lancet 2005; 366: 1809–1820.
Slots J, Ting M . Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis in human periodontal disease: occurrence and treatment. Periodontol 2000 1999; 20: 82–121.
Darveau RP . Periodontitis: a polymicrobial disruption of host homeostasis. Nat Rev Microbiol 8: 481–490.
van Winkelhoff AJ, de Groot P, Abbas F, de Graaff J . Quantitative aspects of the subgingival distribution of Actinobacillus actinomycetemcomitans in a patient with localized juvenile periodontitis. J Clin Periodontol 1994; 21: 199–202.
van Winkelhoff AJ, Slots J . Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis in nonoral infections. Periodontol 2000 1999; 20: 122–135.
Fine DH, Kaplan JB, Kachlany SC, Schreiner HC . How we got attached to Actinobacillus actinomycetemcomitans: a model for infectious diseases. Periodontol 2000 2006; 42: 114–157.
Kachlany SC . Aggregatibacter actinomycetemcomitans leukotoxin: from threat to therapy. J Dent Res 2010; 89: 561–570.
Welch R . RTX toxin structure and function: a story of numerous anomalies and few analogies in toxin biology. Curr Top Microbiol Immunol 2001; 257: 85–111.
Lally ET, Hill RB, Kieba IR, Korostoff J . The interaction between RTX toxins and target cells. Trends Microbiol 1999; 7: 356–361.
Haraszthy VI, Hariharan G, Tinoco EM, Cortelli JR, Lally ET, Davis E et al. Evidence for the role of highly leukotoxic Actinobacillus actinomycetemcomitans in the pathogenesis of localized juvenile and other forms of early-onset periodontitis. J Periodontol 2000; 71: 912–922.
Haubek D, Ennibi OK, Poulsen K, Vaeth M, Poulsen S, Kilian M . Risk of aggressive periodontitis in adolescent carriers of the JP2 clone of Aggregatibacter (Actinobacillus) actinomycetemcomitans in Morocco: a prospective longitudinal cohort study. Lancet 2008; 371: 237–242.
Bueno LC, Mayer MP, DiRienzo JM . Relationship between conversion of localized juvenile periodontitis-susceptible children from health to disease and Actinobacillus actinomycetemcomitans leukotoxin promoter structure. J Periodontol 1998; 69: 998–1007.
Guthmiller JM, Lally ET, Korostoff J . Beyond the specific plaque hypothesis: are highly leukotoxic strains of Actinobacillus actinomycetemcomitans a paradigm for periodontal pathogenesis? Crit Rev Oral Biol Med 2001; 12: 116–124.
Johansson A, Sandström G, Claesson R, Hänström L, Kalfas S . Anaerobic neutrophil-dependent killing of Actinobacillus actinomycetemcomitans in relation to the bacterial leukotoxicity. Eur J Oral Sci 2000; 108: 136–146.
Dinarello CA . Biologic basis for interleukin-1 in disease. Blood 1996; 87: 2095–2147.
Mosser DM, Edwards JP . Exploring the full spectrum of macrophage activation. Nat Rev Immunol 2008; 8: 958–969.
Skaper SD, Debetto P, Giusti P . The P2X7 purinergic receptor: from physiology to neurological disorders. FASEB J 2010; 24: 337–345.
Kelk P, Johansson A, Claesson R, Hänström L, Kalfas S . Caspase 1 involvement in human monocyte lysis induced by Actinobacillus actinomycetemcomitans leukotoxin. Infect Immun 2003; 71: 4448–4455.
Kelk P, Claesson R, Hänström L, Lerner UH, Kalfas S, Johansson A . Abundant secretion of bioactive interleukin-1beta by human macrophages induced by Actinobacillus actinomycetemcomitans leukotoxin. Infect Immun 2005; 73: 453–458.
Kelk P, Claesson R, Chen C, Sjöstedt A, Johansson A . IL-1beta secretion induced by Aggregatibacter (Actinobacillus) actinomycetemcomitans is mainly caused by the leukotoxin. Int J Med Microbiol 2008; 298: 529–541.
Cookson BT, Brennan MA . Pro-inflammatory programmed cell death. Trends Microbiol 2001; 9: 113–114.
Fink SL, Cookson BT . Caspase-1-dependent pore formation during pyroptosis leads to osmotic lysis of infected host macrophages. Cell Microbiol 2006; 8: 1812–1825.
Mariathasan S, Weiss DS, Newton K, McBride J, O'Rourke K, Roose-Girma M et al. Cryopyrin activates the inflammasome in response to toxins and ATP. Nature 2006; 440: 228–232.
Mariathasan S, Weiss DS, Dixit VM, Monack DM . Innate immunity against Francisella tularensis is dependent on the ASC/caspase-1 axis. J Exp Med 2005; 202: 1043–1049.
Dileepan T, Kachlany SC, Balashova NV, Patel J, Maheswaran SK . Human CD18 is the functional receptor for Aggregatibacter actinomycetemcomitans leukotoxin. Infect Immun 2007; 75: 4851–4856.
Schindler R, Clark BD, Dinarello CA . Dissociation between interleukin-1 beta mRNA and protein synthesis in human peripheral blood mononuclear cells. J Biol Chem 1990; 265: 10232–10237.
Guha M, Mackman N . LPS induction of gene expression in human monocytes. Cell Signal 2001; 13: 85–94.
Hsu HY, Wen MH . Lipopolysaccharide-mediated reactive oxygen species and signal transduction in the regulation of interleukin-1 gene expression. J Biol Chem 2002; 277: 22131–22139.
Ward JR, West PW, Ariaans MP, Parker LC, Francis SE, Crossman DC et al. Temporal interleukin-1beta secretion from primary human peripheral blood monocytes by P2X7-independent and P2X7-dependent mechanisms. J Biol Chem 2010; 285: 23147–23158.
Dinarello CA . Anti-inflammatory agents: present and future. Cell 2010; 140: 935–950.
Henderson B, Ward JM, Ready D . Aggregatibacter (Actinobacillus) actinomycetemcomitans: a triple A* periodontopathogen? Periodontol 2000; 54: 78–105.
Johansson A, Hanstrom L, Kalfas S . Inhibition of Actinobacillus actinomycetemcomitans leukotoxicity by bacteria from the subgingival flora. Oral Microbiol Immunol 2000; 15: 218–225.
Moudy R, Manning TJ, Beckers CJ . The loss of cytoplasmic potassium upon host cell breakdown triggers egress of Toxoplasma gondii. J Biol Chem 2001; 276: 41492–41501.
Abd H, Wretlind B, Saeed A, Idsund E, Hultenby K, Sandström G . Pseudomonas aeruginosa utilises its type III secretion system to kill the free-living amoeba Acanthamoeba castellanii. J Eukaryot Microbiol 2008; 55: 235–243.
Acknowledgements
We thank Marie Lindgren, Anita Lie and Inger Lundgren for kind and professional support during the real-time RT-PCR analyses. This study was supported by the Research Fund of Västerbotten County and the Swedish Dental Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by P Meier
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Kelk, P., Abd, H., Claesson, R. et al. Cellular and molecular response of human macrophages exposed to Aggregatibacter actinomycetemcomitans leukotoxin. Cell Death Dis 2, e126 (2011). https://doi.org/10.1038/cddis.2011.6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2011.6
Keywords
This article is cited by
-
The Role of Macrophage Death in Periodontitis: A Review
Inflammation (2024)
-
Leukotoxin (LtxA/Leukothera) induces ATP expulsion via pannexin-1 channels and subsequent cell death in malignant lymphocytes
Scientific Reports (2021)
-
Oral Lactobacillus strains reduce cytotoxicity and cytokine release from peripheral blood mononuclear cells exposed to Aggregatibacter actinomycetemcomitans subtypes in vitro
BMC Microbiology (2020)
-
Relevance of Caspase-1 and Nlrp3 Inflammasome on Inflammatory Bone Resorption in A Murine Model of Periodontitis
Scientific Reports (2020)
-
Dual action of highbush blueberry proanthocyanidins on Aggregatibacter actinomycetemcomitans and the host inflammatory response
BMC Complementary and Alternative Medicine (2018)