Abstract
Background:
High plasma osteopontin (OPN) has been linked to tumour hypoxia, metastasis, and poor prognosis. This study aims to assess whether plasma osteopontin was a biomarker of increasing progression within prostate cancer (PCa) prognostic groups and whether it reflected treatment response to local and systemic therapies.
Methods:
Baseline OPN was determined in men with localised (n=199), locally recurrent (n=9) and castrate-resistant, metastatic PCa (CRPC-MET; n=37). Receiver-operating curves (ROC) were generated to describe the accuracy of OPN for distinguishing between localised risk groups or localised vs metastatic disease. We also measured OPN pre- and posttreatment, following radical prostatectomy, external beam radiotherapy (EBRT), androgen deprivation (AD) or taxane-based chemotherapy.
Results:
The CRPC-MET patients had increased baseline values (mean 219; 56–513 ng ml−1; P<0.0001) compared with the localised, non-metastatic group (mean 72; 12–438 ng ml−1). The area under the ROC to differentiate localised vs metastatic disease was improved when OPN was added to prostate-specific antigen (PSA) (0.943–0.969). Osteopontin neither distinguished high-risk PCa from other localised PCa nor correlated with serum PSA at baseline. Osteopontin levels reduced in low-risk patients after radical prostatectomy (P=0.005) and in CRPC-MET patients after chemotherapy (P=0.027), but not after EBRT or AD.
Conclusion:
Plasma OPN is as good as PSA at predicting treatment response in CRPC-MET patients after chemotherapy. Our data do not support the use of plasma OPN as a biomarker of increasing tumour burden within localised PCa.
Similar content being viewed by others
Main
Prostate cancer (PCa) is the most commonly diagnosed, non-cutaneous male cancer and is the third leading cause of cancer-related death in North America (Gibbons and Waters, 2003). The ability to predict, a priori, an individual PCa patient’s tumour response to surgery, image-guided radiotherapy (IGRT), external beam radiotherapy (EBRT), androgen deprivation (AD) or taxane-based chemotherapy is based on pretreatment clinical factors, including the absolute value and doubling time of prostate-specific antigen (PSA), tumour stage (TNM staging), pathologic Gleason score (GS) and performance status (Nichol et al, 2005; Wo et al, 2009; Armstrong et al, 2010). Prostate-specific antigen is a kallikrein protease produced almost exclusively by luminal cells in the prostate gland (Wo et al, 2009) and its tissue specificity is an important property as a serum biomarker. In large cohorts, the pre- and posttreatment absolute value, and doubling time of PSA, may predict disease-free survival (DFS) and long-term response to localised and systemic treatment (Christensen et al, 2008; Wo et al, 2009). Using PSA alone to monitor EBRT response can be problematic due to the long time (12–24 months) to reach a PSA-nadir, the difficulty in using PSA to monitor tumour cell kill during AD and PSA ‘bounces’ and changes due to benign causes (Christensen et al, 2008). Nonetheless, PSA remains the exclusive blood biomarker used to place patients into prognostic risk groups to determine overall tumour burden and track response following local or systemic treatment (Christensen et al, 2008).
Additional biomarkers that could be used with PSA to denote non-aggressive from aggressive disease, including increasing tumour bulk and/or the presence of occult metastases in the D’Amico high-risk group (any one of: PSA>20 ng ml−1, T3/T4N0M0, GS 8 or above), could effectively triage patients to more individualised PCa management (Christensen et al, 2008; Bristow, 2009). There has been substantial interest in osteopontin (OPN) as a biomarker of cancer aggression, tumour hypoxia and response to treatment (Rittling and Chambers, 2004; Overgaard et al, 2005; Blasberg et al, 2010; Weber et al, 2010; Anborgh et al, 2011). Osteopontin is a small integrin-binding ligand N-linked glycoprotein (SIBLING) that binds to cell surface receptors including integrins and CD44. It is expressed in many tissues and secreted into body fluids, including blood, milk and urine. Osteopontin has important physiological roles in bone remodeling, immune response and inflammation. It is also a tumour-associated protein and elevated OPN levels are associated with cellular proliferation, invasion and angiogenesis via altered activity of matrix metalloproteinases, the epidermal growth factor receptor and PI3K-AKT signaling (Castellano et al, 2008; Anborgh et al, 2011). These preclinical studies suggest that plasma OPN could be an important biomarker of occult systemic metastases.
In a recent meta-analysis of over 228 publications, high plasma or tissue OPN levels correlated with decreased overall survival and DFS across a number of different tumour types, including lung cancer, breast cancer, head and neck cancer, liver cancer and PCa (Weber et al, 2010). High tumour OPN levels as determined by immunohistochemistry (IHC) in situ are associated with pretreatment tumour hypoxia and are prognostic following PCa EBRT (Vergis et al, 2008). In the DAHANCA-5 head and neck trial, high plasma OPN concentrations were correlated with tumour hypoxia and predicted poor loco-regional control following EBRT (Overgaard et al, 2005). Hypoxia in PCa has an important role as it correlates with increased clinical stage and poor prognosis following EBRT and surgery (Movsas et al, 2000; Chan et al, 2007; Vergis et al, 2008; Milosevic et al, 2012).
To date, a definitive study of plasma OPN as a biomarker of increasing tumour aggression (bulk/stage, grade, PSA) across both localised and systemic disease has not been published. Given the reported aggressive nature of OPN-expressing tumours, we explored the role of circulating OPN expression as a potential surrogate biomarker of PCa tumour aggression and occult metastasis. We also assessed OPN levels in response to treatment in both localised and systemic disease.
Materials and methods
Patient samples
Plasma samples were prospectively collected from consenting patients with newly diagnosed PCa attending clinics at Princess Margaret Hospital (University Health Network; University of Toronto) or the London Regional Cancer Center (University of Western Ontario). Written informed consent for blood collection for research purposes was obtained from all patients on local Research Ethics Board (REB)-approved studies of proteomics and biobanking in genitourinary cancers (GU BioBank) (PMH-UHN REB 10-0223-T/08-0124-T). Additional plasma samples in patients with biopsy-proven locally recurrent PCa following treatment with radiotherapy were collected as part of a PHASE I study of MRI-guided prostate biopsies (PMH-UHN REB 05-0641-C). Specimens were collected from 208 men with localised PCa (54, 84, and 61 with low, intermediate and high risk, respectively, and 9 patients with biopsy-proven local recurrence (LR) following radiotherapy ) and 37 men with CRPC-MET. Risk categories were defined by the D’Amico criteria (D'Amico et al, 1999; Nichol et al, 2005) defined as: (1) low risk defined as clinical stage T1 to T2aN0M0, GS 4–6 and PSA of <10 ng ml−1; (2) intermediate risk defined as clinical stage T1 to T2N0M0 and GS of 7 or PSA of 10–20 ng ml−1; (3) high risk defined as clinical stage T3-T4N0M0 or GS of 8–10 or PSA>20 ng ml−1.
Patients with localised low-risk disease were treated with radical prostatectomy (28) or active surveillance (26). Intermediate-risk patients were treated with radical prostatectomy (22) with lymph node sampling or lymphadenectomy (with or without nerve sparing) or intensity-modulated radiotherapy with image guidance (IGRT-IMRT; 60 Gy in 20 fractions or 78 Gy in 39 fractions) (62) (Vesprini et al, 2011). Fifteen localised high-risk patients were treated with pelvic and prostatic IMRT radiotherapy (pelvic dose of 46 Gy and total prostate dose 74 Gy) plus AD therapy (e.g., LHRH-agonist injections given as concurrent and adjuvant therapy for a total period of 3 years) and 45 high-risk patients underwent radical prostatectomy with lymph node sampling or lymphadenectomy. Thirty seven CRPC-MET patients were treated with docetaxel chemotherapy at 75 mg m−2 every 3 weeks with prednisone (Tannock et al, 2004) (Supplementary Table 1). Control plasma OPN samples were collected from 26 healthy volunteers. We also assessed plasma OPN levels from 96 men presenting negative biopsies who were at higher risk for developing PCa (PMH-UHN REB 09-0787-T).
Plasma OPN levels and PSA at baseline were determined for each group of patients before treatment. In a subgroup of patients, OPN and PSA were compared pre- and posttreatment. We defined response to chemotherapy as a >50% reduction in PSA following docetaxel chemotherapy. Blood samples were obtained from patients at the pretreatment appointment and at 1 year posttreatment. For CRPC-MET patients, blood samples were collected before and after the second, third or fourth cycles. Patient-derived toxicity grading was prospectively collected using the Common Terminology Criteria for Adverse Events v3.0 (CTCAE v3.0) as previously described (Christensen et al, 2009). Patients were asked to complete questionnaires concerning symptoms of rectal or bladder injury before, and every week during, radiotherapy as part of their standard of care.
Enzyme-linked immunosorbent assay (ELISA) for OPN
Reporting of plasma OPN measurements and analysis was completed using the National Cancer Institute and European Organization for Research and Treatment of Cancer recommendations for reporting tumour marker prognostic studies (McShane et al, 2006). The dual monoclonal human OPN ELISA kit (Catalog 900-142, Enzo Life Sciences, Plymouth Meeting, PA, USA), was used as previously published (Anborgh et al, 2009) using the manufacturer’s instructions. Human recombinant OPN provided with this kit was used as a standard. Duplicate readings of each plasma sample were averaged.
Statistical analyses
Non-parametric tests were applied to investigate the differences in OPN values between the different risk groups (Mann–Whitney test) or between the pre- vs posttreatment (Wilcoxon-signed rank test). Spearman’s correlation coefficients were calculated to assess correlations between OPN and PSA.
To evaluate the performance of OPN values as a predictor for metastatic disease we plotted the receiver-operating characteristic (ROC) curve. As a measure of performance we calculated the area under the ROC (AUC). The software programs utilized were SAS/STAT Version 9.2 (SAS Institute Inc., Cary, NC, USA) and R (Development Core Team, 2011). For all analyses, P⩽0.05 was interpreted as significant.
Results
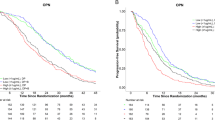
Table 1 shows the baseline characteristics of all the patients in the study. We initially tested differences in OPN and PSA between cohorts of patients with low-risk, intermediate-risk, high-risk prostate and CRPC-MET cancers. In pair-wise testing, PSA differentiated between all tested groups (see Supplementary Table 2). We then compared OPN values in the same groups of patients and found that OPN values were not statistically significantly different between low-, intermediate- or high-risk groups (Figure 1A, and Supplementary Table 2). The OPN values of the CRPC-MET group of patients in this study were similar to a previous published cohort of CRPC-MET using a similar ELISA (20). In each of the localised disease-risk groups, we observed heterogeneity in OPN with values ranging from 12 to 438 ng ml−1 (see Supplementary Table 3a). The OPN levels in the CRPC-MET group (range: 56–513 ng ml−1) were significantly higher to values measured in the localised risk groups (overall mean values of 72 vs 219 ng ml−1; P<0.0001; see 1 : 1 comparisons in Supplementary Table 2). To assess the performance of plasma OPN in distinguishing men with high-risk cancer vs intermediate and low-risk cancer (Figure 1B) or localised vs CRPC-MET disease (Figure 1C), ROC analyses were performed. Figure 1B shows that the AUC was 0.505 (95% confidence interval (CI) 0.417–0.542) for OPN alone. For PSA the AUC was 0.717 (95% CI; 0.632–0.803) and for PSA and OPN together the AUC was 0.72 (95% CI; 0.635–0.806). Figure 1C shows that the AUC for distinguishing CRPC-MET was 0.935 (95% CI; 0.889–0.982) for OPN alone. For PSA the AUC was 0.943 (95% CI; 0.872–1.0) and for PSA and OPN together the AUC was 0.969 (95% CI; 0.918–1.0).
Elevated plasma OPN is associated with CRPC-MET patients. (A) Baseline plasma OPN expression per risk category and in normal volunteers. Plasma OPN values were measured by ELISA assay in localised PCa patients (low, intermediate, high-risk and LR-locally recurrent cancer following radiotherapy); CRPC-MET – castrate-resistant metastatic PCa and non-cancer normal volunteers. (The mean value of plasma OPN values in CRPC-MET as previously published by Anborgh et al (2009) is shown by the black bar (219 μg ml−1)). CRPC-MET patients had significantly increased OPN values compared with localised PCas, including high-risk patients (P-value 0.0001). (B) Receiver-operating curves (ROC) analysis for high-risk patients vs low- and intermediate-risk patients. For OPN: AUC=0.505; 95% CI=0.417–0.542; PSA: AUC=0.717, 95% CI=0.632–0.803; OPN+PSA: AUC=0.72, 95% CI=0.635–0.806. (C) Receiver-operating curves analysis for localised vs castrate resistance PCa patients with known metastatic disease. For OPN: AUC=0.935; 95% CI=0.889–0.982; PSA: AUC=0.943, 95% CI=0.872–1.0; OPN+PSA: AUC=0.969, 95% CI=0.918–1.0.
Taken together, these data confirm that higher circulating plasma OPN levels are observed in CRPC-MET patients as compared with other groups; plasma OPN does not differentiate high-risk patients when compared with intermediate-risk and low-risk patients; plasma OPN is as good as PSA as a predictor of CRPC-MET.
Plasma OPN could be an important biomarker of local or systemic recurrence following surgery or EBRT. However, plasma OPN levels were not uniquely elevated in biopsy-proven LRs following EBRT when compared with localised PCas or non-cancer normal volunteers (P>0.05; Figure 1A). We also noted high plasma levels outliers in Figure 1A (defined as OPN>100 ng ml−1 for non-CRPC-MET patients and OPN>400 ng ml−1 for CRPC-MET patients). A careful chart review did not show that these patients have different clinical outcomes as compared with individuals from the same risk category. This could also represent inflammation-related comorbidities (e.g., rheumatoid arthritis) (24); however, we did not find an association to known comorbidities or clinical symptoms at the time of assay.
Given its role in cell proliferation, hypoxia, angiogenesis and metastasis, OPN could also be an important biomarker for treatment response if it reflected overall local and/or tumour bulk similar to PSA. We therefore investigated whether there was any evidence for change in OPN levels in localised PCas treated with surgery or EBRT (Figure 2). In the low-risk patients that were treated by surgery (Figure 2A), 13 out of 18 patients showed decreased OPN values following surgery with the removal of the entire prostate gland. One out of the five patients without decreasing OPN postsurgery had detectable PSA. The mean change in OPN was −26.5 ng ml−1. A significant decrease in OPN was not observed in high- and intermediate-risk patients after surgery (Figures 2B and C, respectively). There was great heterogeneity in the response of intermediate-risk patients to EBRT with the prostate gland remaining in situ as the overall mean change of OPN in this group was −0.9 ng ml−1 (Figures 2D and E and Figure 4). We also hypothesised that OPN response may differ based on EBRT fraction size or duration and we therefore compared the response in patients receiving 60 Gy in 20 daily fractions (3 Gy fractions; 4 weeks) vs 78 Gy in 39 daily fractions (2 Gy fractions; 8 weeks) using EBRT. We did not find any significant OPN change related to altered fraction size or duration during or after EBRT (Figures 2D and E and Supplementary Figure 1). We also found no evidence for increased baseline or intra-treatment OPN values in patients that had increased acute toxicity (i.e., maximum CTCAE scores 2 out of 3 vs 0 out of 1) during EBRT (see Supplementary Table 4).
Plasma OPN expression in response to local treatment. For each figure: black lines represents patients with decreasing plasma OPN from baseline following treatment, whereas red lines represents patients with increasing plasma OPN from baseline following treatment. The median values pre and post treatment are indicted by the horizontal black bar. (A) Low-risk PCa treated with radical prostatectomy (n=18); (B) High-risk PCa treated with radical prostatectomy and pelvic lymph node dissection (n=39); (C) Intermediate risk PCa treated with radical prostatectomy±pelvic lymph node dissection (n=22); (D) Intermediate-risk PCa treated with IMRT 60 Gy in 20 daily fractions (n=12); (E) Intermediate-risk PCa treated with IMRT 78 Gy in 39 daily fractions (n=29); Only in the low risk group there was a significant response in OPN following surgery (P-value 0.005).
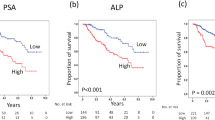
We next investigated whether OPN levels were altered in response to systemic therapies. In the high-risk patients treated with radiotherapy plus AD therapy, the mean OPN level significantly surprisingly increased (+12.4 ng ml−1) even though all patients had PSA response at this time point with no evidence of castrate resistance (Figure 3A). In patients with CRPC-MET receiving two to four cycles of docetaxel chemotherapy there was a statistically significant decrease in OPN levels (−29.1 ng ml−1, P-value=0.027; see Figure 3B). In five patients, there was no reduction in both PSA and OPN with chemotherapy. Fifteen patients had both OPN and PSA decrease after treatment. In all of the responding patients, five patients had an increase in plasma OPN and the remaining seven patients showed minimal change in OPN. The PSA and OPN differences by chemotherapy cycle are presented in Supplementary Figure 2.
Plasma OPN expression response to systemic therapies. For each figure: black lines represents patients with decreasing plasma OPN from baseline following treatment, whereas red lines represents patients with increasing plasma OPN from baseline following treatment. The median values pre and post treatment are indicted by the horizontal black bar. (A) High-risk PCa treated with combined modality therapy of IMRT 74 Gy in 37 daily fractions and AD therapy (ADT) for 3 years (At 1 year post IMRT all patients were continuing on ADT). (B) Metastatic castrate-resistant PCa treated with two to four cycles of chemotherapy.
Finally, we correlated OPN to PSA in our patient cohorts. The change in OPN and PSA following treatment for each patient was calculated and shown in Figure 4. For patients receiving local therapy or systemic therapies, we observed expected reductions in PSA values, but a heterogeneous response with respect to OPN values. The change in OPN does not track with the change of PSA in patients receiving EBRT. Finally, we tested whether plasma OPN levels were a surrogate for serum PSA at baseline or following treatment (Supplementary Figure 3a–c). Plasma PSA and plasma OPN are not correlated at baseline (in all patients or even in the subgroup analysis of localised PCas; Spearman’s correlation coefficients of 0.226 and −0.05, respectively), nor at 1 year posttreatment (Spearman’s correlation coefficient=0.366). We conclude that plasma OPN expression is not a surrogate for serum PSA.
Discussion
Unlike the suggested role of OPN in treatment response in head and neck, lung and breast cancers (Overgaard et al, 2005; Bramwell et al, 2006; Hui et al, 2008; Blasberg et al, 2010), our novel report suggests that plasma OPN in localised PCa is not predictive of response to local therapy when compared with changes in PSA following therapy. In particular, we found no evidence of significantly elevated baseline levels of OPN in high-risk but localised disease relative to low- and intermediate-risk disease. Hence, unlike PSA, OPN is not a direct marker of tumour burden. Longer follow-up will be needed to absolutely determine whether the high OPN outliers in localised risk groups will ultimately fail but we had no evidence that ultra-high levels (>100 ng ml−1) of OPN in localised disease at diagnosis heralds a more aggressive cancer after treatment.
Vergis et al (2008) suggested that IHC staining for tumour OPN in situ was prognostic for response following EBRT or surgery. We did not examine OPN-IHC expression in PCa biopsies in this study. But given the lack of an observed difference between baseline expression of plasma OPN in patients with high-risk PCa and normal volunteers, we would not expect a high degree of concordance between plasma OPN and OPN-IHC as positive staining of OPN in situ occurs in 25% percent of localised PCas (Vergis et al, 2008). Jain et al (2009) recently reported on a number of SIBLING proteins, including plasma OPN, in men with PCa treated with radical prostatectomy. Our results are consistent with their findings, as they did not observe a significant difference in plasma OPN expression between subgroups of patients with different GSs. However, their study did not categorise the patients according to risk group nor treatment response. We observed a significant correlation of plasma OPN to PSA levels pre- and posttreatment following surgery or chemotherapy, but not following radiotherapy or AD, despite strong PSA decline. Plasma OPN levels are therefore not likely to directly reflect PCa cell death during radiotherapy or AD when the prostate gland remains in situ. Further preclinical work using PCa models will be needed to understand this observation. It will also be important to study OPN following second-generation AD therapies such as abiraterone or MDV3100 (de Bono et al, 2011; Scher et al, 2012).
We have previously reported using the same plasma samples from the EBRT cohort that there was a significant increase in IFN-gamma and IL-6 during EBRT. In this study, increasing IL-2 and IL-1 expression were associated with increased probability of acute gastrointestinal and genitourinary toxicity, respectively (Christensen et al, 2009). As OPN is secreted by activated macrophages, leukocytes and activated T lymphocytes and is chemotactic for macrophages and neutrophils, we hypothesised that OPN could have a role in EBRT-associated toxicity and acute inflammatory response (Rittling and Chambers, 2004; Castellano et al, 2008; Bazzichi et al, 2009; Weber et al, 2010). However, our data do not support plasma OPN as a biomarker of endogenous or iatrogenic (e.g., EBRT-induced) inflammation (See Supplementary Figure 1 and Supplementary Table 4). We speculate that the overall driving mechanism of increased baseline plasma OPN levels in our CRPC-MET patients is secondary to OPN’s roles in tumour cell adhesion, migration and matrix degradation during the formation of bone metastases (Hotte et al, 2002; Rittling and Chambers, 2004; Weber et al, 2010). It would be of interest to measure OPN response to intermittent AD during the intervals ‘on’ and ‘off’ therapy in prostate patients with biochemical recurrent disease. In the setting of CRPC-MET and docetaxel chemotherapy treatment, reduced OPN levels was observed in 23 of 31 patients. Reductions in plasma OPN in CRPC-MET patients may therefore be biomarker of response relating to bone metastases.
Conclusion
Plasma OPN is a biomarker of CRPC-MET. Plasma OPN might be used to track response to chemotherapy, where it correlates to treatment-induced changes in PSA. However, OPN levels do not directly track PSA changes following EBRT or AD and may not reflect local or occult metastatic burden in PCa. Our studies support future prospective studies of the use of plasma OPN as a response biomarker in PCa chemotherapy trials.
Change history
08 August 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Anborgh PH, Mutrie JC, Tuck AB, Chambers AF (2011) Pre- and post-translational regulation of osteopontin in cancer. J Cell Commun Signal 5: 111–122
Anborgh PH, Wilson SM, Tuck AB, Winquist E, Schmidt N, Hart R, Kon S, Maeda M, Uede T, Stitt LW, Chambers AF (2009) New dual monoclonal ELISA for measuring plasma osteopontin as a biomarker associated with survival in prostate cancer: clinical validation and comparison of multiple ELISAs. Clin Chem 55: 895–903
Armstrong AJ, Garrett-Mayer E, de Wit R, Tannock I, Eisenberger M (2010) Prediction of survival following first-line chemotherapy in men with castration-resistant metastatic prostate cancer. Clin Cancer Res 16: 203–211
Bazzichi L, Ghiadoni L, Rossi A, Bernardini M, Lanza M, De Feo F, Giacomelli C, Mencaroni I, Raimo K, Rossi M, Mazzone AM, Taddei S, Bombardieri S (2009) Osteopontin is associated with increased arterial stiffness in rheumatoid arthritis. Mol Med 15: 402–406
Blasberg JD, Pass HI, Goparaju CM, Flores RM, Lee S, Donington JS (2010) Reduction of elevated plasma osteopontin levels with resection of non-small-cell lung cancer. J Clin Oncol 28: 936–941
Bramwell VH, Doig GS, Tuck AB, Wilson SM, Tonkin KS, Tomiak A, Perera F, Vandenberg TA, Chambers AF (2006) Serial plasma osteopontin levels have prognostic value in metastatic breast cancer. Clin Cancer Res 12: 3337–3343
Bristow RG (2009) IMRT and molecular biological approaches in radiotherapy for prostate cancer. Eur J Cancer 45 (Suppl 1): 429–430
Castellano G, Malaponte G, Mazzarino MC, Figini M, Marchese F, Gangemi P, Travali S, Stivala F, Canevari S, Libra M (2008) Activation of the osteopontin/matrix metalloproteinase-9 pathway correlates with prostate cancer progression. Clin Cancer Res 14: 7470–7480
Chan N, Milosevic M, Bristow RG (2007) Tumor hypoxia, DNA repair and prostate cancer progression: new targets and new therapies. Future Oncol 3: 329–341
Christensen E, Evans KR, Menard C, Pintilie M, Bristow RG (2008) Practical approaches to proteomic biomarkers within prostate cancer radiotherapy trials. Cancer Metastasis Rev 27: 375–385
Christensen E, Pintilie M, Evans KR, Lenarduzzi M, Menard C, Catton CN, Diamandis EP, Bristow RG (2009) Longitudinal cytokine expression during IMRT for prostate cancer and acute treatment toxicity. Clin Cancer Res 15: 5576–5583
D'Amico AV, Whittington R, Malkowicz SB, Fondurulia J, Chen MH, Kaplan I, Beard CJ, Tomaszewski JE, Renshaw AA, Wein A, Coleman CN (1999) Pretreatment nomogram for prostate-specific antigen recurrence after radical prostatectomy or external-beam radiation therapy for clinically localized prostate cancer. J Clin Oncol 17: 168–172
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, Chi KN, Jones RJ, Goodman OB, Saad F, Staffurth JN, Mainwaring P, Harland S, Flaig TW, Hutson TE, Cheng T, Patterson H, Hainsworth JD, Ryan CJ, Sternberg CN, Ellard SL, Flechon A, Saleh M, Scholz M, Efstathiou E, Zivi A, Bianchini D, Loriot Y, Chieffo N, Kheoh T, Haqq CM, Scher HI (2011) Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 364: 1995–2005
Development Core Team (2011) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, ISBN 3-900051-07-0. URL: http://www.R-project.org/
Gibbons L, Waters C (2003) Prostate cancer–testing, incidence, surgery and mortality. Health Rep 14: 9–20
Hotte SJ, Winquist EW, Stitt L, Wilson SM, Chambers AF (2002) Plasma osteopontin: associations with survival and metastasis to bone in men with hormone-refractory prostate carcinoma. Cancer 95: 506–512
Hui EP, Sung FL, Yu BK, Wong CS, Ma BB, Lin X, Chan A, Wong WL, Chan AT (2008) Plasma osteopontin, hypoxia, and response to radiotherapy in nasopharyngeal cancer. Clin Cancer Res 14: 7080–7087
Jain A, McKnight DA, Fisher LW, Humphreys EB, Mangold LA, Partin AW, Fedarko NS (2009) Small integrin-binding proteins as serum markers for prostate cancer detection. Clin Cancer Res 15: 5199–5207
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100: 229–235
Milosevic M, Warde P, Menard C, Chung P, Toi A, Ishkanian A, McLean M, Pintilie M, Sykes J, Gospodarowicz M, Catton C, Hill RP, Bristow R (2012) Tumor hypoxia predicts biochemical failure following radiotherapy for clinically localized prostate cancer. Clin Cancer Res 18: 2108–2114
Movsas B, Chapman JD, Greenberg RE, Hanlon AL, Horwitz EM, Pinover WH, Stobbe C, Hanks GE (2000) Increasing levels of hypoxia in prostate carcinoma correlate significantly with increasing clinical stage and patient age: an Eppendorf pO(2) study. Cancer 89: 2018–2024
Nichol AM, Warde P, Bristow RG (2005) Optimal treatment of intermediate-risk prostate carcinoma with radiotherapy: clinical and translational issues. Cancer 104: 891–905
Overgaard J, Eriksen JG, Nordsmark M, Alsner J, Horsman MR (2005) Plasma osteopontin, hypoxia, and response to the hypoxia sensitiser nimorazole in radiotherapy of head and neck cancer: results from the DAHANCA 5 randomised double-blind placebo-controlled trial. Lancet Oncol 6: 757–764
Rittling SR, Chambers AF (2004) Role of osteopontin in tumour progression. Br J Cancer 90: 1877–1881
Scher H, Fizazi K, Saad F, Taplin M-E, Sternberg C, Miller K, De Wit R, Mulders P, Hirmand M, Selby M, De Bono J (2012) Effect of MDV3100, an androgen receptor signaling inhibitor (ARSI), on overall survival in patients with prostate cancer postdocetaxel: results from the phase III AFFIRM study. J Clin Oncol 30 (suppl 5): abstr LBA1
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, Oudard S, Theodore C, James ND, Turesson I, Rosenthal MA, Eisenberger MA (2004) Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 351: 1502–1512
Vergis R, Corbishley CM, Norman AR, Bartlett J, Jhavar S, Borre M, Heeboll S, Horwich A, Huddart R, Khoo V, Eeles R, Cooper C, Sydes M, Dearnaley D, Parker C (2008) Intrinsic markers of tumour hypoxia and angiogenesis in localised prostate cancer and outcome of radical treatment: a retrospective analysis of two randomised radiotherapy trials and one surgical cohort study. Lancet Oncol 9: 342–351
Vesprini D, Sia M, Lockwood G, Moseley D, Rosewall T, Bayley A, Bristow R, Chung P, Menard C, Milosevic M, Warde P, Catton C (2011) Role of principal component analysis in predicting toxicity in prostate cancer patients treated with hypofractionated intensity-modulated radiation therapy. Int J Radiat Oncol Biol Phys 81: e415–e421
Weber GF, Lett GS, Haubein NC (2010) Osteopontin is a marker for cancer aggressiveness and patient survival. Br J Cancer 103: 861–869
Wo JY, Chen MH, Nguyen PL, Renshaw AA, Loffredo MJ, Kantoff PW, D'Amico AV (2009) Evaluating the combined effect of comorbidity and prostate-specific antigen kinetics on the risk of death in men after prostate-specific antigen recurrence. J Clin Oncol 27: 6000–6005
Acknowledgements
This research is funded by operating funds from a Terry Fox Project Program PMH Hypoxia grant (RGB), the PMH-Campbell Family Cancer Research Institute PCa Program (RGB/NF/CC/JWT) and the RMP-PMH Academic Fund (RGB/CC), monies form the Orillia Motorcycle Ride for Dad (RGB), the Lloyd Carr-Harris Foundation (PHA/AFC) and also in part by the Ontario Ministry of Health and Long-Term Care. The views expressed do not necessarily reflect those of the OMOHLTC. RGB is a Canadian Cancer Society Research Scientist. AFC is Canada Research Chair in Oncology, supported by the Canada Research Chairs Program. We thank Dr. Eric Winquist for his review of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
AFC received in-kind research support and royalties from Enzo Life Sciences Inc., for sale of OPN antibody products. The other authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies the paper on British Journal of Cancer website
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Thoms, J., Dal Pra, A., Anborgh, P. et al. Plasma osteopontin as a biomarker of prostate cancer aggression: relationship to risk category and treatment response. Br J Cancer 107, 840–846 (2012). https://doi.org/10.1038/bjc.2012.345
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.345
Keywords
This article is cited by
-
Fibroblasts play a potential role in bone destruction via osteopontin related caldesmon expression and polymerization in human non-functioning pituitary adenomas
Scientific Reports (2017)
-
Osteopontin splice variants are differential predictors of breast cancer treatment responses
BMC Cancer (2016)
-
Changes in plasma biomarkers following treatment with cabozantinib in metastatic castration-resistant prostate cancer: a post hoc analysis of an extension cohort of a phase II trial
Journal of Translational Medicine (2016)
-
The combination of serum insulin, osteopontin, and hepatocyte growth factor predicts time to castration-resistant progression in androgen dependent metastatic prostate cancer- an exploratory study
BMC Cancer (2016)
-
The role of osteopontin expression in melanoma progression
Tumor Biology (2015)