Abstract
Detection of coronary ischemic lesions by fractional flow reserve (FFR) has been established as the gold standard. In recent years, novel computer based methods have emerged and they can provide simulation of FFR using coronary artery images acquired from coronary computed tomography angiography (FFRCT). This meta-analysis aimed to evaluate diagnostic performance of FFRCT using FFR as the reference standard. Databases of PubMed, Cochrane Library, EMBASE, Medion and Web of Science were searched. Seven studies met the inclusion criteria, including 833 stable patients (1377 vessels or lesions) with suspected or known coronary artery disease (CAD). The patient-based analysis showed pooled estimates of sensitivity, specificity and diagnostic odds ratio (DOR) for detection of ischemic lesions were 0.89 [95%confidence interval (CI), 0.85–0.93], 0.76 (95%CI, 0.64–0.84) and 26.21 (95%CI, 13.14–52.28). At a per-vessel or per-lesion level, the pooled estimates were as follows: sensitivity 0.84 (95%CI, 0.80–0.87), specificity 0.76 (95%CI, 0.67–0.83) and DOR 16.87 (95%CI, 9.41–30.25). Area under summary receiver operating curves was 0.90 (95%CI, 0.87–0.92) and 0.86 (95%CI, 0.83–0.89) at the two analysis levels, respectively. In conclusion, FFRCT technology achieves a moderate diagnostic performance for noninvasive identification of ischemic lesions in stable patients with suspected or known CAD in comparison to invasive FFR measurement.
Similar content being viewed by others
Introduction
As the most common cause of cardiovascular disease mortality, the prevalence of coronary artery disease (CAD) is still increasing worldwide1. For diagnosis of CAD, invasive coronary angiography (ICA), the standard approach historically, is limited to provide only anatomic information2. Percutaneous coronary intervention (PCI) decision based merely on ICA can result in unbenefited stenting of functionally non-significant lesions or inappropriate deferral of PCI of functionally significant lesions3. Fractional flow reserve (FFR), measured during ICA, has been established as the reference standard in evaluating the functional significance of a coronary stenosis4. In addition, the clinical utility of FFR as a decisive tool for revascularization therapy has been evaluated by several prospective randomized trials, demonstrating how FFR-guided PCI can optimize benefits of revascularization and improve long-term outcomes compared with angiographic guidance alone5,6,7,8. Revascularization decision with FFR guidance has also been shown to be a sound strategy in terms of cost-benefits with significantly fewer stents implanted and less contrast agent used in comparison with PCI guided by ICA alone9. Nevertheless, FFR is an invasive method after all, bringing potential procedural risks for patients4.
An alternative technique called noninvasive fractional flow reserve derived from coronary computed tomography angiography (FFRCT) has been developed10. Through utilization of computational fluid dynamics and coronary artery images acquired from coronary computed tomography angiography, FFRCT enables estimation of FFR value without the need for additional invasive imaging, modification of acquisition protocols, or extra administration of medication. Hence, it is able to provide information both on the anatomic severity of a coronary lesion and its functional significance in a relatively safe and economical manner. Since its feasibility was initially validated in 201111, a number of clinical studies have been conducted to evaluate the diagnostic efficacy of FFRCT using FFR as the reference standard12,13,14,15.
Previous meta-analyses have evaluated the diagnostic performance of FFRCT both at the per-patient level and the per-vessel or per-lesion level as defined by the invasive FFR16,17. However, concerns have been raised about the applicability of univariate model in pooling estimates of sensitivity and specificity, either with fixed- or random-effects model, which might inadvertently produce inaccurate results by ignoring threshold effects and correlation between the two estimates18. Moreover, results of new diagnostic accuracy tests for assessment of FFRCT have recently been published as full papers19,20. Therefore, an updated meta-analysis was carried out to comprehensively search and review evidence available heretofore and derive reliable assessment of the diagnostic performances of FFRCT using a bivariate model as the method for pooling diagnostic measures.
Results
Literature search and characteristics of the included studies
The initial search yielded 343 items from PubMed, the Cochrane Library, EMBASE, Medion and Web of Science. Because of using a board search strategy, most of the results were not eligible. After exclusion based on title, abstract and full-text, seven eligible studies fulfilled the pre-defined inclusion criteria and were included in this systematic review and meta-analysis11,12,13,14,15,19,20. Procedure of studies inclusion was described in Fig. 1. Characteristics of included studies and patients’ baseline demographic were presented in Table 1. Inclusion and exclusion criteria of each study were listed in Supplementary Table 1.
Out of these seven studies published between 2011 and 2015, four were prospective multicenter trials11,12,13,15, and the remaining three were retrospective single-center trials14,19,20. A total of 833 patients (1377 vessels or lesions) were analyzed. The sample size of each study ranged from 21 to 254 patients (23 to 484 vessels or lesions). All participants were stable patients with suspected or known CAD. More males were included than females, with mean age ranging from 60 to 65 years, diabetes prevalence from 14% to 32% in each study. All CT images in the seven studies were acquired in accordance with a standard coronary computed tomography angiography (CCTA) protocol using multi-slice CT scanner (64 slices or higher) or dual source CT scanner. For exact comparison, the point of FFRCT estimation was deduced from the position of the pressure guide wire for invasive FFR. And the process of FFRCT calculation was performed using either a HeartFlow or a Siemens software. In terms of cut-off points, most studies used the same one to define positive results (FFRCT ≤ 0.80; FFR ≤ 0.80) except one by Renker et al. (FFRCT < 0.80; FFR < 0.80). The diagnostic performance of FFRCT at the per-vessel or per-lesion level were reported by all included studies11,12,13,14,15,19,20, while the per-patient analysis was pooled from five studies11,12,14,15,20. The count data on the per-patient and the per-vessel or per-lesion basis for primary study including true positive (TP), false positive (FP), false negative (FN) and true negative (TN) were extracted and shown in Table 1.
Quality of studies
The results of Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) for included studies were summarized in Table 2 and Supplementary Fig. 1. In terms of signaling questions about interval between index and reference test in flow and timing of reference standard, most studies were recorded as “unclear” apart from the DISCOVER-FLOW trial. Nevertheless, all studies were well rated as “low risk” in all domains in relation with risk bias and applicability concerns. Proportion of studies with low risk of bias and with low concerns regarding applicability were 100%, respectively. Hence, all these primary diagnostic accuracy tests were included for synthesis of diagnostic performance.
Synthesis of diagnostic performance
Pooled diagnostic performances of FFRCT at the two analysis levels were summarized in Table 3.
At the per-patient level, the pooled estimates of sensitivity, specificity and diagnostic odds ratio (DOR) for the detection of ischemia-causing coronary stenosis were 0.89 [95% confidence interval (CI), 0.85–0.93], 0.76 (95% CI, 0.64–0.84) and 26.21 (95% CI, 13.14–52.28) (Fig. 2a). The corresponding summary positive likelihood ratio (PLR) and negative likelihood ratio (NLR) were 3.68 (95% CI, 2.41–5.61) and 0.14 (95% CI, 0.09–0.21), respectively, and the combined diagnostic score was 3.27 (95% CI, 2.58–3.96) (Table 3).
The pooled estimates of diagnostic performance at the per-vessel or per-lesion level were as follows: sensitivity 0.84 (95% CI, 0.80–0.87), specificity 0.76 (95% CI, 0.67–0.83), DOR 16.87 (95%CI, 9.41–30.25), PLR 3.51 (95% CI, 2.44–5.03), NLR 0.21 (95% CI, 0.16–0.27) and diagnostic score 2.83 (95% CI, 2.24–3.41) (Fig. 2b and Table 3).
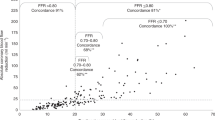
The area under summary receiver operating curves (SROC) at the per-patient level and at the per-vessel or per lesion level was 0.90 (95% CI, 0.87–0.92) and 0.86 (0.83–0.89), respectively (Fig. 2c,d). Through graphical examination of SROC plot, the threshold effects were deemed absent either at the per patient level nor at the per-vessel or per-lesion level, with Spearman correlation coefficients being−0.60 (P = 0.285) and−0.036 (P = 0.939) respectively.
Fagan’s Nomogram analysis (Fig. 3) revealed that, with fixed pre-test probability of 20% and a pooled PLR of 3.68 at the per-patient level and 3.51 at the per-vessel or per-lesion level, the post-test probability was increased to 48% and to 47% respectively. Conversely, with a combined NLR of 0.14 and 0.21, the post-test probability was decreased to 3% and 5% at the two analysis levels, respectively.
In each plot, a vertical axis on the left showed the fixed pre-test probability. Using the likelihood ratio in the middle axis, post-test probability (patient’s probability of having the disease after the index test result was known) was acquired. (a) With a pre-test probability of a positive FFR of 20%, the post-test probability of positive FFR, given positive and negative FFRCT results, were 48% and 3%. (b) With a pre-test probability of a positive FFR of 20% on a per-lesion basis, the post-test probability of FFR, given positive and negative FFRCT results, were 47% and 5%.
Meta-regression analysis
The meta-regression analysis at the per-patient level and at the per-vessel or per-lesion level indicated that the publication date, study design, sample size, age, gender, diabetes, CT scanner type, time period between FFRCT and FFR, software for FFRCT calculation and cut-off value for FFRCT and FFR were not sources of heterogeneity.
Publication bias
The publication bias, at first, was visually assessed using Deeks funnel plots (Fig. 4). The two plots were both in symmetrical funnel shape, indicating the publication bias was likely absent. Moreover, P values for the Deeks funnel plot asymmetry test on the per-patient basis and on the per-vessel or per-lesion basis were 0.34 and 0.76, respectively. Therefore, publication bias did not exist at the two analysis levels.
Discussion
This current systematic review and meta-analysis of seven diagnostic accuracy studies including 833 suspected or known CAD patients (1377 vessels or lesions) investigated the potential of FFRCT for identification of ischemic lesions. Recently approved by the US Food and Drug Administration, FFRCT based on computational fluid dynamics allows for virtual assessment of “3-vessel FFR” at any point within the coronary artery bed from typically acquired CCTA imaging21. Thus, not only the anatomic severity but also the estimated physiological significance of coronary stenosis was taken into account. Notably, FFRCT technology is moving forward from comparison with invasive FFR measures and the real-world implementation of FFRCT for clinical decision making has been validated22.
As widely known, CCTA as a noninvasive technique for evaluation of CAD has been rapidly progressing in recent years23. And high diagnostic accuracy of 64-, 128-, 256-, 320-slice, CCTA in identification of CAD has been demonstrated by multiple studies24,25,26,27. In particular, the constantly high negative predictive value (NPV) makes CCTA a “gate keeper” in ruling out significant CAD. Indeed, for detection of ischemic lesions confirmed by the invasive FFR, CCTA maintained high combined estimates of sensitivity and NPV (92% and 87%, respectively) while the specificity and positive predictive value (PPV) was only modest (43% and 57%, respectively)17. As recently reported by an integrated analysis of three pivotal trials (DISCOVER-FLOW, DeFACTO and NTX), FFRCT exhibited numerically higher sensitivity (86.1% vs 82.8%, P = 0.369) and NPV (92.5% vs 91.6%, P = 0.645)28. Besides, FFRCT was found with significantly improved specificity (77.7% vs 55.7%, P < 0.001) and PPV (60.8% vs 38.7%, P < 0.001) compared with CCTA. In the current study, the pooled estimates of sensitivity (0.89 at the per-patient level and 0.84 at the per-vessel or per-lesion level) and specificity (0.76 at both of the two levels) was in line with the former findings16,17,28. To evaluate the real-world performance of FFRCT with improved specificity in differentiating a true-positive from a false-positive test, a pragmatic comparative effectiveness PLATFORM (Prospective Longitudinal Trial of FFRCT: Outcomes and Resource Impacts) trial was conducted29. Among patients referred to ICA in this trial, 12% of patients in the arm of FFRCT combined with CCTA were found with no obstructive CAD confirmed by ICA, while in the ICA arm the rate was 73% (risk difference 61%, P < 0.0001). In a recent report of PLATFORM trial regarding economic implications of FFRCT strategy, patients in the arm of FFRCT and CCTA were associated with a 32% reduction in costs compared with patients in the ICA arm30. This encouraging outcome which stemmed from a significant reduction in false-positive noninvasive test results was believed to be of considerable importance for health care milieu.
The area under the SROC provides a general evaluation of diagnostic efficacy. According to the recommended guideline for interpretation of AUSROC value31, the diagnostic ability of FFRCT for identification of ischemic lesions was moderate at the per-patient level and at the per-vessel or per-lesion level (AUSROC: 0.90, 0.86). DOR is a measure combining sensitivity and specificity together. And the higher value of DOR, the higher the diagnostic efficacy of the test to detect between subjects with and without the disease of interest. Our pooled estimates of DOR were 26.21 and 16.87 at the two analysis levels, respectively, indicating a moderate diagnostic value of FFRCT in detection of lesion-specific ischemia. As shown in Fig. 4, Fagan’s nomogram revealed that the application of FFRCT would raise the post-test probability of patients having ischemic lesions (confirmed by invasive FFR) from 20% to 48% at the per-patient level and to 47% at the per-vessel or per-lesion level. Meanwhile, the probability of having negative FFR status was decreased from 20% to 3% on the per-patient basis and to 5% on the per-vessel or per-lesion basis. According to these findings, FFRCT was demonstrated to be of moderate value in determining the lesions causing ischemia.
It is generally known that CCTA image quality could be suboptimal owing to technical issues such as severe calcification23. In this situation, CCTA examination was uninterpretable and the subsequent FFRCT analysis could not be done. 12.05% of subjects (5.21% with severe calcification) in the NXT trial and 8.20% of subjects (4.92% with severe calcification) in the study by Coenen et al. were excluded from analysis due to unavailable CCTA image. Hence, there were concerns about the influence of selection bias and test heterogeneity in the pooled diagnostic accuracy of FFRCT. However, according to a sub-study of NXT trial32, FFRCT was immune to the influence of calcification since no difference of diagnostic efficacy was observed across any coronary artery calcium (CAC) score quartiles. Even among patients with Agatston CAC score above 416, FFRCT was observed with improved detection of ischemic lesions over the CCTA (AUC: 0.91 vs 0.71; P = 0.0004).
In addition to these diagnostic features, an emerging body of clinical evidence has indicated that the application of FFRCT may have an influence on therapeutic strategy21. In the RIPCORD (Does Routine Pressure Wire Assessment Influence Management Strategy at Coronary Angiography for Diagnosis of Chest Pain) trial, 36% of patients were observed with a change in diagnostic and therapeutic management. Based on the results of FFRCT, 12% of patients with planned medical therapy alone were sent for ICA, while 30% of patient assigned with ICA were reassigned to medical therapy33. Among patients with intended revascularization, 18% were found to have ischemic lesions in different vessels. Furthermore, not merely diagnosing ischemic lesions before PCI, FFRCT was also capable of predicting hemodynamic effect of revascularization, thus enabling “virtual stenting” of a coronary lesion, which may be beneficial to treatment planning before invasive procedures13.
Compared with high diagnostic performance of FFRCT for identification of lesion-specific ischemia reported by the most recent meta-analysis16, the diagnostic efficacy was moderate in the present study. The difference can be explained by several reasons. Firstly, the current meta-analysis retrieved studies until January 31st, 2016, adding two studies with 127 patients and 212 vessels or lesions, so that more comprehensive evaluation of the diagnostic efficacy of FFRCT was obtained19,20. Secondly, software for FFRCT analysis used in three studies was different from the rest. Last but not least, a different statistical method for combining diagnostic estimates was applied in the current study.
Combined with patient-specific CT image-based modeling, computational fluid dynamics technology and lumped cardiac and coronary microcirculatory model, FFRCT is applied for determining the individual physiologic conditions of CAD patients34. Although two different kinds of software, HeartFlow and Siemens cFFR, were used in the included studies based on the same principles mentioned above, the algorithms for FFRCT analysis were different. In terms of HeartFlow11,12,13,15, the CCTA data were transferred to a parallel supercomputer off-site for construction of the coronary flow model on the basis of full order algorithm. Meanwhile, FFRCT calculation in studies with application of Siemens cFFR14,19,20 was based on integration of the full and reduced order algorithm in the software. In atherosclerotic or stenotic vascular segments of interest, the full order algorithm was applied while the reduced order algorithm, usually performed on a regular workstation on-site within hospital, was used for the rest healthy coronary artery segments.
Different from therapeutic or intervention studies, diagnostic accuracy studies are characteristic of evaluation by a pair of summary estimates (sensitivity and specificity), different thresholds chosen from a wide range of values, and commonly larger between-study heterogeneity31. Bivariate model is a multivariate method, jointly analyzing and assessing diagnostic accuracy of a test35. This model, unlike separate pooling methods such as fixed- or random-effects model, utilizes a hierarchical structure of the distribution of data in terms of two levels. In detail, a within-study variability is considered by supposing a binomial distribution for the sensitivity and 1-specificity of each study at the first level, while at the second level a between-study heterogeneity is modeled by assuming a bivariate normal distribution through the logit-transformed sensitivity and specificity18. Hence, bivariate model preserves the two-dimensional nature of diagnostic accuracy, allows for a potential correlation between sensitivity and specificity, and manages the differences in the precision of the two estimates. It should be noted that, the bivariate model is currently regarded as the optimal method for acquiring pooled statistics from diagnostic accuracy trials with recommendation from the Diagnostic Test Accuracy Working Group of the Cochrane Collaboration and the Agency for Healthcare Research and Quality (AHRQ)31. As shown in Supplementary Table 2, diagnostic performances of FFRCT at the two analysis levels with or without two recent studies (Coenen et al. and Geer et al.19,20) using two different pooling statistical methods was pooled. The synthesized AUSROC by the bivariate model was numerically conservative in comparison with that by univariate model both in per-patient level and per-vessel or per-lesion level. In consideration of the significant between-study heterogeneity in this study, it is appropriate to use the model of bivariate. Therefore, the pooled estimates of FFRCT diagnostic measures in our systematic review and meta-analysis, with incorporation of updated clinical data and application of the optimal combing method, were believed to be comprehensive and reliable.
There are several limitations which deserve to be mentioned. Firstly, the number of studies included in this systematic review and meta-analysis was relatively small. Secondly, subjects in our study were limited to stable patients with stable known or suspected CAD, excluding patients with complex lesions and a history of prior percutaneous coronary intervention or coronary bypass surgery in vessels of interest. Hence the diagnostic performance of FFRCT on wider groups of patients are unknown. Thirdly, diagnostic efficacy of FFRCT in patients with intermediate lesions was reported by DeFACTO study and NXT study at the per-patient level12,15, while DISCOVER-FLOW study, DeFACTO study and study by Coenen et al. have reported diagnostic measures on the per-vessel or per-lesion basis11,12,19. In consideration of the minimum number of studies required for data synthesis using the bivariate model, the combination of diagnostic accuracy of FFRCT in patients with coronary stenosis of intermediate severity was not performed. In addition, covariates that affect sensitivity and specificity in the bivariate model were not used due to limited data presented by the original included studies. Finally, heterogeneities did exist in this study but the sources of them could not be identified using the current pre-defined factors.
In conclusion, up-to-date evidence available about the FFRCT diagnostic efficacy was synthesized in the present systematic review and meta-analysis with inclusion of seven diagnostic accuracy studies. And FFRCT may in the future be of help for identification of lesions causing ischemia among stable patients with suspected or known CAD. However, more pragmatic clinical trials with larger subsets of CAD patients are warranted to demonstrate its clinical benefits in real world practice.
Methods
Literature search strategy
To identify eligible studies published through January 31st, 2016, the main search was conducted in databases of PubMed, the Cochrane Library, EMBASE, Medion and Web of Science using various combinations of Medical Subject Headings (MeSH) and non-MeSH terms: fractional flow reserve, FFR, noninvasive fractional flow reserve, noninvasive FFR, non-invasive fractional flow reserve, non-invasive FFR and FFR derived from coronary computed tomography angiography. We also searched related reports from major annual meetings in field of Cardiology and Radiology. Manual search of reference sections of eligible studies and all relevant reviews was also performed. We did not apply any language restrictions.
Study Identification
Two investigators (Wen Wu and Dao-Rong Pan) independently carried out the systematic literature search, study identification, data extraction and quality assessment in accordance with Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement36. (kappa index = 0.956, indicating excellent between the two investigators). Any discrepancy was resolved by discussion with a third reviewer (Si Pang). Studies were included when following criteria were met: (1) conducted as a diagnosis accuracy test; (2) the index test was FFRCT and the standard test was FFR; (3) at least 10 study subjects were involved; (4) a two-by-two contingency table could be constructed from data presented by the study. Trials were excluded on the basis of the following criteria: (1) phantom-only study; (2) studies conducted on animals or in-vitro systems; (3) the article pertained to review, case report, editorial comment or prognostic study; (4) study containing overlapping participants. Notably, article by the same author or research group was included only when it used a different sample of patients.
Data extraction
At first, basic information about studies including first author, study design and publication year was extracted. Further extracted variables comprising patients’ baseline demographics, technical information and absolute numbers of TP, FP, FP and FN were also exacted from eligible studies using a standardized form.
Quality assessment
The QUADAS-2 tool was used to flag facets of a study which were associated with the potential bias37. Aimed to help reviewers judge risks of bias, QUADAS-2 consists of four key domains including patient selection, index test, reference test flow of patients through the study and timing of the index test and the reference test (flow and timing). These four domains were applied for assessing risks of bias and the first three were used to evaluate concerns of applicability. Based on reviewer authors’ answers for all signaling questions in each domain, risks of bias were judged as “low risk”, “high risk” or “unclear risk”. In terms of applicability concerns, review authors were asked to record relevant information and then to assess their concerns if the study matched the review question. In a similar way, concerns with respect to applicability were rated as “low risk”, “high risk” or “unclear risk”. And the results of the QUADAS-2, with numbers of studies observed with low, high or unclear bias risk or applicability concern for each domain, were summarized in a standardized table and figure recommended by the QUADADS-2 official website.
Data synthesis and statistical analysis
The analysis of diagnostic performance was carried out on both of the per-patient and the per-vessel or per-lesion basis. Using a bivariate model, pooled estimates of sensitivity, specificity, PLR, NLR, DOR, diagnostic score and AUSROC with the corresponding 95% CI were calculated38. To be notable, sensitivity, specificity, DOR and AUSROC were regarded as the major outcome measures. Two-tailed P-value of less than 0.05 was considered to be significant.
To estimate a patient’s probability of having a disease of interest after the FFRCT test, Fagan’s nomogram analysis was conducted39. Briefly, the plot comprises a vertical axis on the left with fixed pre-test probability, an axis in the middle signifying the likelihood ratio (to what extent the index test would raise or lower the probability of having the disease), and a vertical axis on the right standing for the post-test probability, which indicates the patient’s probability of having the disease (or having the positive result of reference standard test) after the index test result was known.
A Cochrane-Q test was used to assess heterogeneity40. Inconsistency index, I2, quantifies the magnitude of heterogeneity as a percentile, with a cut-off valve of I2 at 50% being defined statistically significant heterogeneity. Meta-regression analysis was performed to explore the possible sources of heterogeneity in terms of publication date, study design, sample size, age, gender, diabetes, CT scanner type, time period between FFRCT and FFR, software for FFRCT calculation and cut-off value for FFRCT and FFR. Other possible sources of heterogeneity were not included as a result of data insufficiency in at least one study.
Diagnostic threshold effects were identified by visual evaluation of SROC plots at first and then by Spearman correlation analysis40. And publication bias was inspected by Deeks funnel plot, a scatter plot of the inverse of the square root of the effective sample size (1/root (ESS)) against the ln (DOR)41.
Data synthesis and most statistical analyses were performed by STATA software version 12.0 (College Station, TX, USA) except the Meta-regression analysis by Meta-Disc version 1.4 (Clinical Biostatistics Unit, Hospital Ramon y Cajal, Madrid, Spain).
Additional Information
How to cite this article: Wu, W. et al. Noninvasive fractional flow reserve derived from coronary computed tomography angiography for identification of ischemic lesions: a systematic review and meta-analysis. Sci. Rep. 6, 29409; doi: 10.1038/srep29409 (2016).
References
Mozaffarian, D. et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 133, e38–38e360 (2016).
Lotfi, A. et al. Expert consensus statement on the use of fractional flow reserve, intravascular ultrasound, and optical coherence tomography: a consensus statement of the Society of Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 83, 509–518 (2014).
Liga, R. et al. Multicentre multi-device hybrid imaging study of coronary artery disease: results from the EValuation of INtegrated Cardiac Imaging for the Detection and Characterization of Ischaemic Heart Disease (EVINCI) hybrid imaging population. Eur Heart J Cardiovasc Imaging. 6, jew038 doi: 10.1093/ehjci/jew038 (2016).
Pijls, N. H., Tanaka, N. & Fearon, W. F. Functional assessment of coronary stenoses: can we live without it. Eur. Heart J 34, 1335–1344 (2013).
Pijls, N. H. et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J. Am. Coll. Cardiol. 49, 2105–2111 (2007).
van Nunen L. X. et al. Fractional flow reserve versus angiography for guidance of PCI in patients with multivessel coronary artery disease (FAME): 5-year follow-up of a randomised controlled trial. Lancet. 386, 1853–1860 (2015).
De Bruyne B. et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N. Engl. J. Med. 371, 1208–1217 (2014).
Tonino, P. A. et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 360, 213–224 (2009).
Fearon, W. F. et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation. 122, 2545–2550 (2010).
Taylor, C. A., Fonte, T. A. & Min, J. K. Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: Scientific basis. J. Am. Coll. Cardiol. 61, 2233–2241 (2013).
Koo, B. K. et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms: Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J. Am. Coll. Cardiol. 58, 1989–1997 (2011).
Min, J. K. et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. 308, 1237–1245 (2012).
Kim, K. et al. A novel noninvasive technology for treatment planning using virtual coronary stenting and computed tomography-derived computed fractional flow reserve. JACC Cardiovasc Interv. 7, 72–78 (2014).
Renker, M. et al. Comparison of diagnostic value of a novel noninvasive coronary computed tomography angiography method versus standard coronary angiography for assessing fractional flow reserve. Am. J. Cardiol. 114, 1303–1308 (2014).
Nørgaard, B. L. et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J. Am. Coll. Cardiol. 63, 1145–1155 (2014).
Deng, S. et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in coronary artery disease: A systematic review and meta-analysis. Int. J. Cardiol. 184, 703–709 (2015).
Gonzalez, J. A. et al. Meta-Analysis of Diagnostic Performance of Coronary Computed Tomography Angiography, Computed Tomography Perfusion, and Computed Tomography-Fractional Flow Reserve in Functional Myocardial Ischemia Assessment Versus Invasive Fractional Flow Reserve. Am. J. Cardiol. 116, 1469–1478 (2015).
Lee, J., Kim, K. W., Choi, S. H. & Huh, J. Systematic Review and Meta-Analysis of Studies Evaluating Diagnostic Test Accuracy : A Practical Review for Clinical Researchers–Part II . Statistical Methods of Meta-Analysis. Korean J Radiol 16, 1188–1196 (2015).
Coenen, A. et al. Fractional flow reserve computed from noninvasive CT angiography data: diagnostic performance of an on-site clinician-operated computational fluid dynamics algorithm. Radiology. 274, 674–683 (2015).
De Geer, J. et al. Software-based on-site estimation of fractional flow reserve using standard coronary CT angiography data. Acta Radiol. 0, 1–7 (2015).
Min, J. K. et al. Noninvasive fractional flow reserve derived from coronary CT angiography clinical data and scientific principles. JACC: Cardiovascular Imaging. 8, 1209–1222 (2015).
Nørgaard, B. L. et al. Clinical Use of Coronary CTA-Derived FFR for Decision-Making in Stable CAD. JACC: Cardiovascular Imaging. 6, 2015.11.025 doi: 10.1016/j.jcmg.2015.11.025 (2016).
Maurovich-horvat, P., Ferencik, M., Voros, S., Merkely, B. & Hoffmann, U. Comprehensive plaque assessment by coronary CT angiography. Nat Rev Cardiol. 11, 390–402 (2014).
Paech, D. C. & Weston, A. R. A systematic review of the clinical effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of suspected coronary artery disease. BMC Cardiovasc Disord. 11, 32 (2011).
Alkadhi, H. et al. Low-dose, 128-slice, dual-source CT coronary angiography: accuracy and radiation dose of the high-pitch and the step-and-shoot mode. Heart. 96, 933–938 (2010).
Korosoglou, G. et al. Quantitative assessment of stenosis severity and atherosclerotic plaque composition using 256-slice computed tomography. Eur Radiol. 20, 1841–1850 (2010).
Li, S. et al. Diagnostic accuracy of 320-slice computed tomography angiography for detection of coronary artery stenosis: meta-analysis. Int. J. Cardiol. 168, 2699–2705 (2013).
Xu, R., Li, C., Qian, J. & Ge, J. Computed Tomography-Derived Fractional Flow Reserve in the Detection of Lesion-Specific Ischemia: An Integrated Analysis of 3 Pivotal Trials. Medicine (Baltimore). 94, e1963 (2015).
Douglas, P. S. et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFRct: outcome and resource impacts stud. Eur. Heart J 36, 3359–3367 (2015).
Hlatky, M. A. et al. Quality-of-Life and Economic Outcomes of Assessing Fractional Flow Reserve With Computed Tomography Angiography: PLATFORM. J. Am. Coll. Cardiol. 66, 2315–2323 (2015).
Bae, J. M. An overview of systematic reviews of diagnostic tests accuracy. Epidemiol Health. 36, e2014016 (2014).
Nørgaard, B. L. et al. Influence of Coronary Calcification on the Diagnostic Performance of CT Angiography Derived FFR in Coronary Artery Disease: A Substudy of the NXT Trial. JACC Cardiovasc Imaging. 8, 1045–1055 (2015).
Curzen, N. et al. Does routine pressure wire assessment influence management strategy at coronary angiography for diagnosis of chest pain?: the RIPCORD study. Circ Cardiovasc Interv. 7, 248–255 (2014).
Taylor, C. A., Fonte, T. A. & Min, J. K. Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: scientific basis. J. Am. Coll. Cardiol. 61, 2233–2241 (2013).
Reitsma, J. B. et al. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 58, 982–990 (2005).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 339, b2700 (2009).
Whiting, P. F. et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 155, 529–536 (2011).
Menke, J. Bivariate random-effects meta-analysis of sensitivity and specificity with the Bayesian SAS PROC MCMC: methodology and empirical evaluation in 50 meta-analyses. Med Decis Making. 33, 692–701 (2013).
Caraguel, C. G. & Vanderstichel, R. The two-step Fagan’s nomogram: ad hoc interpretation of a diagnostic test result without calculation. Evid Based Med. 18, 125–128 (2013).
Devillé, W. L. et al. Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol. 2, 9 (2002).
Deeks, J. J., Macaskill, P. & Irwig, L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 58, 882–893 (2005).
Acknowledgements
We appreciate Hai Chen, Xin-lei Wu for assistance with the statistics analysis and valuable discussion. With great honor, we acknowledge the editors and reviewers for insightful suggestions on this reviewing work.
Author information
Authors and Affiliations
Contributions
W.W., D.-R.P. and S.P. were responsible for the systematic literature search, study identification, data extraction and quality assessment. P.Y., X.-M.R. and J.L. analyzed the results. W.W. and N.F. wrote this paper. N.H., A.N. and S.-L.C. revised the manuscript. All authors have reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Wu, W., Pan, DR., Foin, N. et al. Noninvasive fractional flow reserve derived from coronary computed tomography angiography for identification of ischemic lesions: a systematic review and meta-analysis. Sci Rep 6, 29409 (2016). https://doi.org/10.1038/srep29409
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep29409
This article is cited by
-
Impact of Pressure Guidewire on Model-Based FFR Prediction
Cardiovascular Engineering and Technology (2024)
-
CTA-Based Non-invasive Estimation of Pressure Gradients Across a CoA: a Validation Against Cardiac Catheterisation
Journal of Cardiovascular Translational Research (2021)
-
Adjustment of CT-fractional flow reserve based on fluid–structure interaction underestimation to minimize 1-year cardiac events
Heart and Vessels (2020)
-
Computed tomographic evaluation of myocardial ischemia
Japanese Journal of Radiology (2020)
-
Computationally simulated fractional flow reserve from coronary computed tomography angiography based on fractional myocardial mass
The International Journal of Cardiovascular Imaging (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.