Abstract
Study design:
Thirty-six patients with unsatisfactory treatment of neurogenic bowel dysfunctions (NBD) were enrolled from Spinal Units and Rehabilitation Centers in Italy. Treatment was for 3 weeks using a newly developed integrated system with an enema continence catheter for transanal irrigation (Peristeen, Coloplast A/S Kokkedal Denmark).
Objectives:
To evaluate the effects of Peristeen Anal Irrigation on NBD and patient quality of life (QoL).
Setting:
Italy.
Methods:
Lesion level, ambulatory status and hand functionality were determined in all patients. NBD symptoms and QoL were evaluated before and after treatment, using a specific questionnaire. Statistical analysis was performed using McNemar Test and Sign Test.
Results:
Thirty-six patients were enrolled, and 32 patients completed the study. At the end of the treatment, 28.6% of patients reduced or eliminated their use of pharmaceuticals. Twenty-four patients became less dependent on their caregiver. There was a significant increase in patients' opinion of their intestinal functionality (P=0.001), QoL score (P=0.001) and their answers regarding their degree of satisfaction (P=0.001). A successful outcome was recorded for 68% of patients with fecal incontinence, and for 63% of patients with constipation.
Conclusion:
Peristeen Anal Irrigation is a simple therapeutic method for managing NBD and improving QoL. It should be considered as the treatment of choice for NBD, playing a role in the neurogenic bowel analogous to that of intermittent clean catheterization in bladder treatment.
Similar content being viewed by others
Introduction
Patients with neurological diseases affecting the spinal cord, such as spinal cord lesion, spina bifida and multiple sclerosis, often experience disturbances of bowel and bladder function. This reduces quality of life (QoL) and restricts social activities. These patients may suffer from constipation, fecal incontinence or both.1, 2, 3, 4, 5 While urological sequelae and their treatment are well documented,6, 7 neurogenic bowel dysfunctions (NBD) are among the least discussed topics in the literature, perhaps because of the misperception that there is little serious morbidity or mortality associated with NBD.8 For these reasons, treatment of NBD has been largely empirical and individual solutions have been sought. Management of NBD has often involved diet, mild laxatives combined with sporadic enemas or digital maneuvers.9 In most patients, a regular conservative bowel management is not effective, and during the last decade, several new therapeutic modalities were suggested: prokinetic agents,10 biofeedback,11 enema continence catheter,12 the Malone antegrade continence enema administered through an appendicostomy13, 14 and sacral nerve stimulation.15, 16 To date, there is limited evidence in the literature supporting any bowel management program for NBD.17 However, a recent randomized controlled trial found that patients treated with the Peristeen Anal Irrigation System (Coloplast A/S, Kokkedal, Denmark) had fewer complaints of constipation, less fecal incontinence, improved symptom-related QoL and reduced time consumption on bowel management procedures compared with patients treated by conservative bowel management.18
The Peristeen Anal Irrigation System is specially designed to ease bowel irrigation in spinal cord-injured patients. The irrigation procedure can be done without assistance from another person, even by immobilized patients and patients with poor hand function. This study aimed to evaluate whether this self-administered transanal irrigation system would improve the QoL and NBD symptoms of patients by comparing patient status before and after treatment.
Materials and methods
Thirty-six patients with severe NBD were enrolled into the study from Italian Spinal Units and Neurological Rehabilitation Centers between December 2005 and August 2006. Patients were classified according to International Standards for Neurological and Functional Classification of Spinal Cord Injury.19 Patients eligible for inclusion were aged ⩾18 years, had a congenital SCL or had acquired an SCL at least 6 months previously and had severe NBD with unsatisfactory bowel management defined as (a) spending half an hour or more attempting to defecate each day or every 2 days; (b) fecal incontinence occurring once or more in a month; (c) symptoms of autonomic dysreflexia before or during evacuation; or (d) abdominal discomfort or pain before or during defecation. Patients were excluded if they had mental instability or disability, evidence of bowel obstruction or inflammatory bowel diseases, previous abdominal or perineal surgery, implant of sacral nerve stimulation or were pregnant.
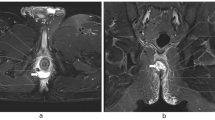
Eligible patients were admitted to the study after written informed consent was obtained. Patients using drugs or alternative methods for evacuation discontinued their treatment 7 days before entering the study. During initial and control visits, personal information and medical history were collected from patients, as well as information regarding intestinal function, its effect on daily activities and his/her general level of satisfaction. Urinary function was assessed by videourodynamic study. The Peristeen Anal Irrigation System (Coloplast A/S Kokkedal, Denmark) was used for NBD treatment.18 The system comprises a coated rectal balloon catheter, manual pump, pressure control unit and water container (Figure 1). The catheter is inserted into the rectum and the balloon inflated to hold the catheter in the rectum while a tap water enema is slowly administered with the manual pump. Subsequently, the balloon is deflated and the catheter removed, followed by bowel emptying of the enema and other bowel contents. The volume of water used, the degree of balloon inflation and the frequency of enema administration are determined during the first weeks of the treatment. Initially, 750 ml of tepid tap water is administered once a day. When the feeling of effective emptying is achieved, the irrigation frequency is reduced to once in every 2 days or less. During the first visit, patients were trained how to use the self-administered transanal irrigation system by specialized nurses. For all patients, the treatment period was 3 weeks.
A validated questionnaire for assessing QoL in NBD was not available in Italian, so a questionnaire to measure the impact of NBD treatment on QoL was designed by a group of experts, including a colorectal surgeon, a gastroenterologist, a urologist, a neurologist and an epidemiologist.20 The short questionnaire was structured to cover (a) urinary function—bladder function, methods of bladder emptying, frequency of urinary tract infections and current prophylactic treatment; (b) bowel function—duration of the evacuation disorder, method of defecation currently used as well as pharmaceuticals, dietary supplements and/or other products, the need for assistance for evacuation and the predominant intestinal symptom during and after defecation; (c) NBD—difficulty and/or painful exertion in connection with evacuation, the feeling of incomplete evacuation, abdominal pain or discomfort before or after evacuation, leakage of feces, gas incontinence, time necessary for each evacuation or attempt at evacuation, the need to use the fingers to stimulate evacuation, time of the day at which evacuation usually occurs and opinion of the quality of intestinal functioning; and (d) QoL—opinion of daily activity and QoL and general satisfaction. The questionnaire was hospital administered during initial and control visits by medical personnel trained specifically for this purpose, using an out or in-patient regimen.
The statistical analysis was performed using the program SPSS/PC (SPSS Inc., Chicago, IL, USA), Version 13.0. The descriptive before-and-after analysis involved the calculation of frequency and percentages. Variables used in the QoL questionnaire included scale and nominal variables, answered using never, rarely, occasionally, often, always; ordinal variables, answered with increasing value; and dichotomous variables, answered using yes or no. The McNemar test was used to analyze the ordinal variables and for the before-and-after comparison of dichotomous variables (yes or no), the Sign test was used for numerical scale variables or value variables (including, for example, never, rarely, occasionally, often, always) and variation for numerical scales (from 0 to 10). Tests with P⩽0.01 were considered to be statistically significant.
We certify that all applicable institutional or governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Thirty-six patients were enrolled, 33 of these fulfilled the eligibility criteria and were included in the study. Thirty-two patients completed the study and were included in the analysis, and one patient was lost to follow-up. The patient lost to follow-up was accounted for in the analysis using statistical methods. The median age was 31.6 years (s.d.±13.3), and there were 18 male and 15 female patients. Demographic characteristics are summarized in Table 1.
The predominant intestinal symptom at the first visit was constipation in 27 patients, fecal incontinence in four patients and not recorded for one patient. These disorders were present from the time of the lesion in 78.8% of the cases. Regarding the need for assistance to evacuate, 19 patients were independent, nine patients were partially dependent and five patients were totally dependent. In all, 60.6% of patients used pharmaceuticals, dietary supplements or other products. Eleven patients regularly used rectal suppositories or enemas, two patients used manual evacuation and six patients did not use any specific treatment. Fourteen patients used more than one method of defecation simultaneously, and the combinations of methods used are summarized in Table 2.
Questionnaire responses, given before and after using the self-administered transanal irrigation system for evaluating symptoms during evacuation, sensation of incomplete evacuation, abdominal pain or discomfort, leakage of feces or gas incontinence, are reported in Table 3, and the time necessary for evacuation and the requirement for mechanical stimulation are given in Table 4. There was no significant change in the time of day at which evacuation usually occurred after the treatment period compared with before. Patients' opinion of their intestinal function, daily activity, QoL and general satisfaction is given in Table 5.
While using the Peristeen Anal Irrigation System, 88.9% of patients did not report any urinary infection. In all, 28.6% of patients reduced or eliminated their use of pharmaceuticals.18 When asked about symptoms in connection with evacuation, there was a net increase in the answers ‘never’ and ‘rarely’ in the before-and-after evaluation (P=0.001), as the feeling of incomplete evacuation was found to be considerably decreased. Abdominal pain or discomfort before or after evacuation was also reduced (P=0.001). After treatment, there was an increase in the number of patients not having leakage of feces (P=0.002), and the number of patients not experiencing gas incontinence (P=0.002). The time of evacuation after the treatment period also decreased (P=0.004). There was an increase in patients' opinion of their intestinal functionality (P=0.001), their QoL score (P=0.001) and their answers regarding the degree of satisfaction (P=0.001).
A high percentage of patients reported a change in their level of dependency after the treatment period: 24 patients considered they were less dependent, two patients considered they were more dependent and six patients reported no variation in their dependence on caregivers and family. Irrigation frequency was every 2 days for 18 patients, 1–3 times a week for 10 patients and one or more times a day for five patients. The average volume of water used during the irrigation operation was 789 ml (s.d.±222 ml). Twenty-one patients did not encounter any difficulty in inserting the catheter, nine patients experienced difficulties occasionally and only one patient always had difficulties. This information was not recorded for two patients. When using the Peristeen Anal Irrigation System, 14 patients did not record leakage of irrigation fluid, 14 patients recorded leakage occasionally and five patients recorded leakage often. Catheter expulsion was recorded occasionally in only 11 patients. No adverse events were recorded.
Discussion
Neurogenic bowel dysfunctions are a well-established complication of several neurological conditions. Studies have shown that NBD patients have a prolonged colonic transit time, and that anal squeeze pressure, anorectal sensibility and anal resting pressure may also be impaired. Furthermore, a reduced rectal compliance due to hyperreactivity of the rectum to distension was demonstrated in patients with high spinal lesions. NBD affect 62.5–95% of spinal cord lesion patients.12 For the two most common symptoms of NBD, constipation or obstructive defecation is reported by 36–81% of patients in the different pathologies and fecal incontinence is reported by 13.9–75% of patients, depending on the definition used.17 While it is well established that NBD have a major impact on daily life activities and QoL in spinal cord lesion patients, treatment of NBD is still controversial owing to a lack of complete trial and long-term studies in different neurological diseases. While bowel conservative management has been suggested in most patients, NBD are mostly left untreated. Transanal irrigation was originally developed for treating NBD in children with spina bifida, and there are very few published results of the use of the transanal enema administration in adults. The effect of enema administration is in part due to a simple mechanical wash-out effect, but studies of enema administration through colostomies have shown that irrigation with an enema above 250 ml generates colonic mass movements. However, there is the potential risk of bowel perforation when introducing a catheter into the anorectum, as well as of autonomic dysreflexia in patients with lesions above T6. In some patients, this may increase the effect of irrigation, but in patients using transanal irrigation, it may lead to giant contractions of the rectum and subsequently leakage or expulsion of the catheter, as in patients with supraconal injury.
While using the Peristeen Anal Irrigation System, patients reported improved intestinal functioning. Further data analysis showed that the most striking results were related to symptoms associated with evacuation: the feeling of incomplete evacuation, abdominal pain or discomfort before or after evacuation, leakage of feces and gas incontinence. At the final visit, none of the patients reported having these disorders ‘always’ or ‘often’, and the number of people who reported not having these problems any more increased considerably.
Our results confirmed a successful outcome regarding fecal incontinence (68%) and constipation (63%). In a recent trial using the Peristeen Anal Irrigation System, a successful outcome was reported for 73% of patients regarding fecal incontinence and 40% of patients regarding constipation.18 Difficulties with catheter introduction, expulsion of catheter, leakage and burst of balloon were reduced with the Peristeen Anal Irrigation System.18 The ease of manual handling of the pump, control unit and irrigation system effectively increased the independence of patients.
Therefore, using the Peristeen Anal Irrigation System improved intestinal functioning and increased QoL in the opinion of the majority of the patients who took part in the study; at a minimum follow-up of 6 months after the end of the study, 39.3% of patients had a high level of physical acceptance of the self-administered transanal irrigation system, were extremely satisfied and preferred to use the self-administered transanal irrigation system rather than previous bowel emptying habits. However, only a small number of patients participated in this brief study, and long-term follow-up is needed to further support the use of the self-administered transanal system.
Conclusion
Transanal irrigation is a simple therapeutic method of managing NBD. The Peristeen Anal Irrigation System was effective in facilitating transanal irrigation treatment in the patients in this study, including those with impaired mobility and diminished hand function. Patients found the self-administered transanal irrigation system easy-to-use and all experienced improved QoL, with minor side effects. The Peristeen Anal Irrigation System seems to be highly suitable for adults with spinal cord lesion, suggesting that transanal irrigation may play a role in bowel emptying, analogous to the use of intermittent clean catheterization for neurological bladder treatment. Long-term follow-up data are required to confirm the results of this study. However, in our opinion, the self-administered transanal irrigation system should be considered in all neurological patients as a first therapeutic approach for NBD before using more invasive treatment modalities such as Malone antegrade continence enema or construction of a permanent left-side colostomy.
References
Christensen P, Olsen N, Krogh K, Bacher T, Laurberg S . Scintigraphic assessment of retrograde colonic washout in fecal incontinence and constipation. Dis Colon Rectum 2003; 46: 68–76.
Christensen P, Olsen N, Krogh K, Laurberg S . Scintigraphic assessment of antegrade colonic irrigation through an appendicostomy or a neoappendicostomy. Br J Surg 2002; 89: 1275–1280.
Glickman S, Kamm MA . Bowel dysfunction in spinal-cord injury patients. Lancet 1996; 347: 1651–1653.
Krogh K, Nielsen J, Djurhuus JC, Mosdal C, Sabroe S, Laurberg S . Colorectal function in patients with spinal cord lesions. Dis Colon Rectum 1997; 40: 1233–1239.
Harari D, Sarkarati M, Gurwitz JH, McGlinchey-Berroth G, Minaker KL . Constipation-related symptoms and bowel program concerning individuals with spinal cord injury. Spinal Cord 1997; 35: 394–401.
Malone PS, Wheeler RA, Williams JE . Continence in patients with spina bifida: long term results. Arch Dis Child 1994; 70: 107–110.
Bakke A, Myhr KM, Gronning M, Nyland H . Bladder, bowel and sexual dysfunction in patients with multiple sclerosis a cohort study. Scand J Urol Nephrol Suppl 1996; 179: 61–66.
Menter R, Weitzenkamp D, Cooper D, Bingley J, Charlifue S, Whiteneck G . Bowel management outcomes in individuals with long-term spinal cord injuries. Spinal Cord 1997; 35: 608–612.
Whitehead WE, Wald A, Norton NJ . Treatment options for fecal incontinence. Dis Colon Rectum 2001; 44: 131–142.
Binnie NJ, Creasey GH, Edmond P, Smith AN . The action of Cisapride on the chronic constipation of paraplegia. Paraplegia 1988; 26: 151–158.
Loening-Baucke V, Desch L, Wolraich M . Biofeedback training for patients with myelomeningocele and fecal incontinence. Dev Med Child Neurol 1988; 30: 781–790.
Christensen P, Kvitzau B, Krogh K, Buntzen S, Laurberg S . Neurogenic colorectal dysfunction—use of new antegrade and retrograde colonic wash-out methods. Spinal Cord 2000; 38: 255–261.
Squire R, Kiely EM, Carr B, Ransley PG, Duffy PG . The clinical application of the Malone antegrade colonic enema. J Pediatr Surg 1993; 28: 1012–1015.
Krogh K, Laurberg S . Malone antegrade continence enema for faecal incontinence and constipation in adults. Br J Surg 1998; 85: 974–977.
Rosen HR, Urbarz C, Holzer B, Novi G, Schiessel R . Sacral nerve stimulation as treatment for fecal incontinence. Gastroenterology 2001; 121: 536–541.
Marshall DF, Boston VE . Altered bladder and bowel function following cutaneous electrical field stimulation in children with spina bifida—interim results of a randomized double-blind placebo controlled trial. Eur J Pediatr Surg 1997; 7 (Suppl 1): 41–43.
Coggrave M, Wiesel PH, Norton C . Management of faecal incontinence and constipations in adults with central neurological diseases. Cochrane Database Syst Rev 2006 (February 22 (2)); CD002115, Review.
Christensen P, Bazzocchi G, Coggrave M, Abel R, Hultling C, Krogh K et al. A randomized controlled trial of transanal irrigation versus conservative bowel management in spinal cord-injured patients. Gastroenterology 2006; 131: 738–747.
American Spinal Injury Association. Manual for the International Standards for Neurological Classification of Spinal Cord Injury. American Spinal Injury Association: Chicago, 2003.
Krogh K, Christensen P, Sabroe S, Laurberg S . Neurogenic bowel dysfunction score. Spinal Cord 2006; 44: 625–631.
Acknowledgements
We thank Dr Cristian Cintori, Dr Achille Grisetti and Dr Alessandro Porciani for their support in data collection and analysis. We thank Dianthus Medical Limited for providing medical writing services. This research was supported for data analysis by Coloplast Italia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Del Popolo, G., Mosiello, G., Pilati, C. et al. Treatment of neurogenic bowel dysfunction using transanal irrigation: a multicenter Italian study. Spinal Cord 46, 517–522 (2008). https://doi.org/10.1038/sj.sc.3102167
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102167
Keywords
This article is cited by
-
Neurogenic Bowel: Traditional Approaches and Clinical Pearls
Current Physical Medicine and Rehabilitation Reports (2020)
-
Peristeen Transanal Irrigation System to Manage Bowel Dysfunction: A NICE Medical Technology Guidance
Applied Health Economics and Health Policy (2019)
-
From misbelieve to proofs in transanal irrigation for functional bowel problems
Techniques in Coloproctology (2016)
-
Application of transanal irrigation for patients with spinal cord injury in South Korea: a 6-month follow-up study
Spinal Cord (2013)
-
The effects of transanal irrigation as a stepwise bowel management program on the quality of life of children with spina bifida and their caregivers
Spinal Cord (2013)