Abstract
Study design:
A case report of cervical myelopathy caused by epidural β2-microglobulin (β2m) amyloid deposits in a 50-year-old woman with haemodialysis treatment.
Objective:
Long-term haemodialysis in patients with end-stage renal disease leads to several complications based on β2m deposits, which can affect, in the cervical spine, the intervertebral disk, and in rare cases, they may compress the spinal cord and nerves. The objective of this report is to describe the clinical and radiological follow-up preceding the indispensable surgical excision of an amyloid mass in a 50-year-old woman with haemodialysis treatment. Long-term postoperative cervicalgia owing to subcondylian bone cyst-associated atlanto-occipital instability is also described and discussed.
Setting:
Department of Neurosurgery A, Hop Pellegrin, Bordeaux, France.
Case report:
We present a clinical case of a patient with spinal cord compression. The patient was treated by surgical excision of an amyloid mass subsequent to a C2–C3 laminectomy. The patient experienced clinical improvement with a regression of all of her neurological symptoms. Histological findings confirm the diagnosis of β2m amyloid deposition. However, 5 years after surgery the subcondylian bone cysts were still observed and atlanto-occipital instability required her to wear a minerva.
Conclusion:
Our case report confirms that surgical excision of β2m epidural deposits is necessary and relevant when neurological prognosis is discussed, and that pain is still the major symptom of disease evolution. The use of high-flux synthetic membranes could decrease the β2m blood level and early renal graft is the only method to prevent such complications.
Similar content being viewed by others
Introduction
Patients with end-stage renal disease are exposed to a variety of spondylarthropathy complications.1 Dialysis-related amyloidosis (DRA) is a unique type of amyloidosis affecting patients undergoing haemodialysis. Many symptoms of DRA are associated with β2-microglobulin (β2m) deposits inside and around joints. However, the most severe complication involves β2m deposits destroying paravertebral ligaments and disks, which can result in spinal cord compression. We report a case of cervical spinal compression by β2m deposits in haemodialysis patient, which required surgery.
Case report
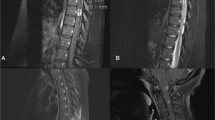
A 50-year-old woman with a 26-year history of haemodialysis for Cacchi and Ricci disease (medullary sponge kidney) was evaluated for moderate paresthesia of the shoulder and hand. The initial neurological examination was normal and spinal cord magnetic resonance imaging (MRI) showed a thickened cervical ligamentum flavum. Clinical and radiological follow-up was initiated for a few years. Progressively, without a traumatic event, mechanic-like cervical pain appeared that was less and less curbed at rest. Cervicalgia became both continuous and increasingly more intense. Afterwards, neuralgia in the greater occipital nerve territory was associated with dysesthesia of the right arm. Neurological examination located right C2, C3, and C4 neuralgia, but evidenced hyper-reflexia of the four limbs with clonic reflexes associated with neuropathic pain in the right arm, necessitating the prescription of carbamazepine. Electromyographic signs of polyneuropathy were highlighted. In the right median nerve, motor nerve conduction velocity was estimated at 38.34 m/s (normal >48 m/s), and six terminal motor nerve latency was estimated at 0.36 ms (normal <3.7 ms) −7 mV, between elbow and hand. Examination by the rheumatological department revealed an operated bilateral carpal tunnel, with recurrent syndrome, and a synovial cyst of the left elbow. Serum β2m and parahormone levels were 18 mg/l (normal range from 1.1 to 2.0 mg/l) and 320 pg/ml (normal range from 10 to 55 pg/ml), respectively. There were no clinical or biological signs of infection. Standard X-rays of the cervical spine were normal, but MRI showed a compressive mass at the lateral aspect of the C2–C3 level. A hypointense signal in T1-weighted images (Figure 1), and low signal intensity in T2-weighted images (not shown) were observed in the epidural space. After intravenous gadolinium administration, T1-weighted images revealed an enhancement of this epidural lesion (Figures 2 and 3).
Surgical excision of the mass was performed through a posterior cervical approach after a C2–C3 laminectomy. The yellowish pseudotumour was very firm, highly vascularised, and very strongly attached to a thick ligamentum flavum. Histopathological examination confirmed a DRA (Figure 4). Tissues were fixed in 10% formaldehyde buffer and embedded in paraffin. Specimens were stained using standard Congo red. We observed the presence of an amorphous substance with few histiocytes and multinuclear giant cells. Congo red became fluorescent after thioflavin staining, and became birefringent under polarised light (Figure 5). Immunohistochemistry of the substance revealed the omnipresence β2m (Figure 6).
The patient responded to radical surgery with a good decompression (Figure 7) and a progressive improvement of her neuralgia syndrome and neuropathic pain (decrease in medication). However, important posterior cervicalgia that increased with cervical movements necessitated a cervical collar for 3 months. Five years later, MRI images showed a persistent decompression, but also indicated a thickening of the ligamentum flavum that still remained visible. Subcondylian bone cysts were also observed (Figure 8), with resultant atlanto-occipital instability requiring the patient to wear a minerva.
Discussion
Cervical spinal cord compression due to β2m amyloid epidural deposits is rare. Deposits are possible in the lower cervical spine, in the upper part of the cervical spine, and at the craniocervical junction (atlanto-occipital joint). The incidence of craniocervical involvement observed by systematic MRI is 20–30%, and is often neurologically asymptomatic.2 Disk degeneracy and calcium deposition in the posterior longitudinal ligament and the periodontoidal region (very rarely associated with fracture of the odontoid) are described.1 In addition to destructive lesions, pseudotumours of the craniocervical hinge are noted.3
As we evidenced in our case, the course of deposits is unpredictable, but is generally progressive and poorly symptomatic.4, 5 Cervical pain may be the first symptom and prompt evaluation of long-term dialysis patients should be emphasised so that they can be referred for surgical evaluations.6 Vertebral erosion, end-plate erosion, and disk space collapse may induce spinal instability.7 In our patient, pain was probably associated with spinal instability and, in her clinical course, the patient had persistent postoperative cervicalgia, which was decreased by a minerva. We think that definitive stabilisation of the spine should be indicated, as mentioned by some authors.7 Medical therapy is limited to symptomatic approaches to lessen joint pain and inflammation.4 Nonsteroidal anti-inflammatory drugs or, in severe cases, low-dose prednisolone are available. Surgical decompression has a high morbi-mortality rate, but still remains the treatment of choice for compressive pseudotumours.8
Spinal cord compression was evidenced on MRI, which showed hypointense, or isointense deposits when compared to the spinal cord in T1-weighted sequences and hypointense deposits in T2-weighted images. Furthermore, gadolinium injection increased the T1-weighted signal of these deposits. In the epidural space, deposits were observed in the ligamentum flavum, without osteophytosis. Crystals of hydroxyapatite or calcium pyrophosphate dihydrate are often observed in haemodialysis patients and computed tomography or standard X-ray of the craniocervical hinges are the only valuable guides to diagnosis. Vertebral osteomyelitis may look similar, but MRI shows a T2 hyperintensity in the case of infection. Plasmocytoma is different from β2m deposits, with typical multiple bone punched-out lesions. Finally, renal osteodystrophy is described with subchondral and subperiostal bone resorption in conjunction with osteomalacia, osteoporosis, and osteosclerosis parallel to the vertebral end plate.7
The mechanism of development of amyloidosis is still debated. β2m is a normal component of the light chain of the major histocompatibility complex type I antigen found on the surface of all nucleated cells. Dialysis is an inflammatory stimulus, inducing cytokine production and complement activation. The released cytokines, including interleukin-1, tumour necrosis factor-alpha, and interleukin-6, are thought to stimulate β2m synthesis and release by macrophages.9 In the case of renal failure, the blood level of this protein increases and macrophages proteolyse β2m, which is then transformed into amyloid.10 In our case, the serum level of β2m was high, and explained the amyloid deposits. Clinical manifestations of DRA generally appear after 5 years of haemodialysis therapy. Unlike other types of amyloidosis, β2m is largely confined to joints and synovial membranes sites. The most frequent peripheral disorder is carpal tunnel syndrome, usually bilateral and progressive in nature. Flexor tenosynovitis, bone cysts, and pathological fractures are also observed.3 The lumbar canal is also a classic location, with subchondral sclerosis and/or infiltration of the epidural space, ligamentum flavum deposits, and intervertebral disk degeneracy. This is responsible for radiculopathy and the cauda equina syndrome.11 Visceral deposits are rare, and tend not to cause symptoms in most cases.3
The prognosis of β2m amyloidosis depends on the duration of dialysis, patient age, seniority of the dialysis, and type of dialysis membrane, which might play a role in the pathogenesis.12, 13 Cuprophan and the cellulose acetate membranes that are used in conventional haemodialysis have small pores and cannot clear substances up to 200 Da molecular mass, thus elevating β2m serum levels. Some authors noted a lowered incidence of DRA involvement when using a polyacrylonitrile membrane, which possesses a much higher clearance capacity for β2m than cuprophan. Effectively, high-flux membranes enhance β2m removal and decrease cytokine stimulation during haemodialysis and hemofiltration.14 Renal transplantation could stop β2m deposition by lowering the blood concentration of β2m to a normal range, halting the progression of the disease.15 Generally, symptoms such as joint pain, swelling, and stiffness disappear within the first week after transplantation.
Conclusion
In DRA, β2m deposits can induce spinal stenosis with nervous compression. Generally, pain inaugurates a patient spinal amyloidosis history, and the physician should care for haemodialysis patients presenting with this symptom. Surgical excision is necessary when deposits become compressive to the spinal cord. The use of high-flux synthetic membranes can decrease the β2m blood level. Early renal graft may prevent these complications.
References
Kuntz D, Naveau B, Bardin T, Druëke T, Treves R, Dryll A . Destructive spondylarthropathy in hemodialyzed patients: a new syndrome. Arthritis Rheum 1984; 27: 369–375.
Chassagne P et al. Spinal cord compression revealing a destructive arthropathy of the atlanto-occipital joint associated with beta-2 microglobulin amyloidosis in a haemodialysed patient. Br J Rheumatol 1992; 31: 427–428.
Rousselin B et al. Pseudotumor of the craniocervical junction during long-term hemodialysis. Arthritis Rheum 1990; 33: 1567–1573.
Danesh FR, Klinkmann J, Yokoo H, Ivanovich P . Fatal cervical spondylarthropathy in a hemodialysis patient with systemic deposition of β2-microglobulin amyloid. Am J Kidney Dis 1999; 33: 563–566.
Allain JJ, Stevens PJ, Bridges LR, Phillips ME . Dialysis myelopathy: quadriparesis due to extradural amyloid of β2-microglobulin. BMJ 1988; 269: 752–753.
Nokura K et al. Dialysis-related spinal canal stenosis: a clinicopathological study on amyloid deposition and its AGE modification. J Neurol Sci 2000; 178: 114–123.
Nair S, Vender J, McCormack TM, Black P . Renal osteodystrophy of the cervical spine: neurosurgical implications. Neurosurgery 1993; 33: 349–354.
Shiota E, Naito M, Tsuchiya K . Surgical therapy for dialysis-related spondyloarthropathy: review of 30 cases. J Spinal Disord 2001; 14: 165–171.
Ramadori G, Mitsch A, Rieder H, Meyer zum Buschenfelde KH . Alpha- and gamma-interferon (IFN alpha, IFN gamma) but not interleukin-1 (IL-1) modulate synthesis and secretion of beta 2-microglobulin by hepatocytes. Eur J Clin Invest 1988; 18: 343–351.
Koch KM . Dialysis-related amyloidosis. Kidney Int 1992; 41: 1416–1429.
Marcelli C et al. Amyloidosis-related cauda equina compression in long-term hemodialysis patients. Three case reports. Spine 1996; 21: 381–385.
Korzets A et al. Quadriparesis and faecal incontinence in a long-term haemodialysis patient. Nephrol Dial Transplant 1997; 12: 224–225.
Hardouin P et al. Current aspects of osteoarticular pathology in patients undergoing hemodialysis: study of 80 patients. J Rheumatol 1987; 14: 784–787.
Davidson GS, Montanera WJ, Fleming JF, Gentili F . Amyloid destructive spondyloarthropathy causing cord compression: related to chronic renal failure and dialysis. Neurosurgery 1993; 33: 519–522.
Jadoul M, Druëcke T, Zingraff J, Van Ypersele De Strihou C . Does dialysis-related amyloidosis regress after transplantation? Nephrol Dial Transplant 1997; 12: 655–657.
Acknowledgements
We are particularly grateful to Professor Jean Guérin, Department of Neurosurgery of Bordeaux, France, for his support in our work.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vignes, JR., Eimer, S., Dupuy, R. et al. β2-Microglobulin amyloidosis caused spinal cord compression in a long-term haemodialysis patient. Spinal Cord 45, 322–326 (2007). https://doi.org/10.1038/sj.sc.3101969
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101969
Keywords
This article is cited by
-
Cervical amyloidoma of transthyretin type: a case report and review of literature
BMC Geriatrics (2022)
-
Spinal cord compression in dialysis-related upper cervical amyloidoma – a case report
Spinal Cord Series and Cases (2021)
-
The unresolved problem of beta-2 microglobulin amyloid deposits in the intervertebral discs of long-term dialysis patients
Journal of Orthopaedic Surgery and Research (2017)
-
Hemodialysis-related upper cervical extradural amyloidoma presenting with intractable radiculopathy
European Spine Journal (2012)