Abstract
Study design:
Retrospective cohort examination.
Objectives:
Data on expectations and satisfaction rates in elderly patients operated for lumbar spinal stenosis (LSS) are limited. The present study aimed to investigate these issues as well as the factors that might affect them.
Setting:
A university affiliated hospital.
Patients and methods:
A follow-up study of 367 consecutive patients aged 65 years and older (mean age 71.4 years), who underwent surgery for degenerative LSS between 1990 and 2000. Data collection included patients' preoperative expectation, demographic data, body mass index, operative risk, duration of symptoms, clinical presentation and patients' satisfaction on follow-up, pain level, activities of daily living level and walking ability. Data were recorded before operation and on follow-up. Preoperative and follow-up data were analyzed by univariate and multivariable models.
Results:
The response rate on follow-up was 81% (298 patients). A logistic regression analysis showed that advanced age, male gender and high education level were independently associated with positive expectations, while a great number of covariates were associated with patients' satisfaction. High patients' expectations were positively interrelated with satisfaction (r=0.332, P<0.001).
Conclusions:
In the elderly, preoperative expectations reasonably predict their postoperative satisfaction rate. It is suggested that a greater effort should be made to narrow the gaps between expectations and satisfaction, perhaps by providing more accurate preoperative information data regarding the outcomes of planned surgery.
Similar content being viewed by others
Introduction
Much of the interaction between patients and physicians is based upon the mutual goal of optimizing patients' health. This has been suggested to affect patients' compliance, satisfaction level and the degree of ‘doctor shopping’.1 Patients' expectations and satisfaction are key measures of the quality of care and are more likely to associate with the quality of life.2
Some studies have concluded that levels of satisfaction are not affected by unmet expectations, or that there was little evidence to show that expectations play a significant role in the evaluation of satisfaction with care.3, 4, 5 However, others have shown that levels of satisfaction do relate to preoperative expectations6, 7 and may serve as significant predictors of dissatisfaction and mood disturbance.1, 2 In particular, patients' satisfaction or dissatisfaction after spinal surgery has been shown to be influenced by patients' expectations, their medical condition and health status, psychosocial variables, and characteristics of the treatment.8, 9, 10 These studies included younger age groups and cannot be generalized to the elderly. A recent follow-up study11 comprising 83 patients reported that patients satisfaction correlated with postoperative back pain, leg pain, numbness and subjective difficulty in walking; however, by multivariate regression analysis the only independent correlate was a subjective walking difficulty, and it was concluded that postoperative level of functioning was weakly correlated with satisfaction.
Satisfaction level reflects both various care variables and patients' own variables such as expectations, characteristics and psychosocial determinants.7 The study of preoperative expectations and postoperative satisfaction in elderly patients operated for lumbar spinal stenosis (LSS) may assist in identifying the factors that affect patients' expectations and satisfaction and uncover the possible interrelations between them.
Methods
Subjects
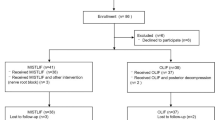
The study took place in the spinal surgery unit of a university affiliated hospital. We included all 367 consecutive patients aged 65 years and older, who underwent surgery for LSS between 1990 and 2000. Upon conclusion of the follow-up period, 5% (17/367) of patients died and the other 7% (52/367) could not be contacted. Informed consent was obtained from all participants and the study was approved by the local Institutional Review Board of the hospital.
The diagnosis of LSS was made on the basis of clinical and radiographic evidence. Indications for surgery included disabling back and/or leg pain and progressively limited walking ability. Only patients with stenosis due to degenerative spondylosis were included.
Assessment of patients
All patients were interviewed by one of the authors (ZA). A locally developed structured questionnaire was used, and a database was compiled using inpatient medical records. We included demographic data, body mass index (BMI), associated comorbidities (based on ICD-9 codes), preoperative risk as assessed by the scale of the American Society of Anesthesiology12 (ASA, graded from ‘ASA class I’ – a normal healthy patient to ‘ASA class V’ – a patient not expected to survive 24 h, with or without surgery), pain perception by the visual analogue scale (VAS, graded as ‘0’ for no pain to ‘10’ point for maximal pain), duration of symptoms, clinical presentation, and walking ability (distance, meters). The level of basic activities of daily living (ADL) was evaluated by the Barthel index13 (patients with an index of less than 55 are defined as dependent, 55–84 need modified dependency, and 85 and more as independent).
Preoperative expectations were assessed by a single question: ‘Do you have low, or high, expectations to have a successful surgical treatment?’ to which patients answered with ‘low/high’. Upon conclusion of the study (December 2000), a telephonic interview was conducted and patients were asked whether they were ‘very or somewhat satisfied’, or ‘somewhat or very dissatisfied’. The reliability and validity of this type of a single-question questionnaire of health care behavior and satisfaction has already been established.5
Statistical analysis
This was a retrospective cohort study. Descriptive statistics were performed by SPSS 12.0. Univariate associations between independent variables and expectations and satisfaction were calculated with the Wilcoxon rank test for categorical variables and Pearson's correlation test for continuous variables. Nonparametric data were analyzed by the χ2 test. A logistic regression analysis was used to assess factors related to patients' positive expectations and satisfaction. Odds ratio and their 95% confidence interval (CI) were calculated. We constructed a logistic model, based on results of the univariate analysis and potential clinical relevance. For covariates we used gender, age, years of education, BMI, Barthel score of ADL, severity of pain on follow-up, number of comorbidities and ASA class.
Results
The mean age of the patients at the time of surgery was 71.4±5.4 years. In all, 62% of them were aged between 65 and 74 years, 29% between 75 and 85 years and 9% were older than 85 years. The general characteristics of the study population are presented in Table 1.
Expectations
There were some differences in baseline characteristics between the group of patients expressing positive preoperative expectations and the group expressing negative expectations. Those having positive expectations were older (71.9±5.4 versus 70.7±5.2 years, P=0.004), males (71% of all group patients versus 18%, χ2=99.9, P<0.001), were not living alone (96% of all group patients versus 89%, χ2=5.8, P=0.016) and had more years of formal education (9.7±3.1 versus 8.5±2.5, P=0.001). Other data regarding duration and clinical presentation of spinal stenosis, type of surgery, decompressed levels and rate of reoperation were similar in the two groups. There was also no significant difference between the age groups (65–74 years, 75–84 years and 85 years and older) with regard to expectations for successful surgery. The logistic regression showed that only male gender, education level, and advanced age were independently and significantly associated with patients' positive expectations (Table 2). The overall accuracy of this model to predict patients' positive expectations was 70%. Sensitivity and specificity were 80 and 55%, respectively, positive predictive value 72% and negative predictive value 43%.
Satisfaction/dissatisfaction
This was evaluated after a mean follow-up time of 41.62 months. The response rate on follow-up was 81% (298/367). Significant improvements were reported with regard to pain perception (ΔVAS scale 4.93, P<0.001), and functional status (ΔBarthel index (15.59, P<0.001). The number of patients who were limited in walking distance up to 50 m decreased by 22% (χ2=44.9, P<0.001), and the number of patients having no walking limitation increased by 27% (χ2=70.6, P<0.001).
On follow-up, 66% of the patients reported to be satisfied. This was more prevalent among males, compared with females (77 and 57%, respectively; χ2=12.94, P<0.001), but was not associated with age.
A logistic regression analysis (Table 3) showed that patients' satisfaction (somewhat or very satisfied) was associated with a number of covariates. These included high preoperative expectations, male gender, education level and walking distance on follow-up. Number of comorbidities (in particular the presence of osteoarthritis, diabetes mellitus, and depression) did not adversely affect satisfaction. The overall accuracy of this model to predict positive patients' satisfaction is 71%, and sensitivity is 85%, specificity is 43.0%, and positive and negative predictive values were 75 and 33%, respectively.
Expectations and satisfaction interrelations
In all, 80% of satisfied patients belonged to those expecting (preoperatively) successful surgery, while only 48% (P<0.001, χ2=33.89) belonged to the group expressing negative expectation. A correlation analysis of expectations and satisfaction resulted in an r value of 0.332, P<0.001.
Discussion
We have retrospectively evaluated expectations, satisfaction and the interrelations existing between expectations and satisfaction in elderly patients undergoing surgery for LSS. Our results suggest that patients' preoperative expectations and their postoperative satisfaction exhibit a complex of multiple relationships of sociodemographic factors, associated diseases and clinical presentation.
The results of the present study are instructive with regard to the following points:
(1) Expectations: Male gender, higher education level, and increasing age were independently associated with high (positive) expectations. These three variables have been recently identified as affecting expectations in patients with other medical conditions also.14 Expectations seem to rely more heavily on personal variables rather than on proper knowledge, thus casting doubt even on aspects concerning informed consent of elderly patients. Expectations represent a cognitive aspect (such as a belief) and may be influenced or even modified by available information. Once established, beliefs manifested as expectations can affect patients' attitudes. Therefore, greater efforts should be made to narrow the gaps between expectations and information data regarding the outcomes of planned surgery.
(2) Satisfaction: A large number of variables were associated with patients' satisfaction/dissatisfaction. These findings are not surprising considering the many publications15, 16, 17, 18 concluding with similar findings, thus emphasizing the complexity of factors associated with the satisfaction level. The findings are in accordance with a previous study,19 suggesting that self-reported nonphysical health status, as well as levels of functional walking ability (rather than functional ADL), may be more important than clinical status when judging patients' satisfaction.
(3) Expectation/satisfaction interrelation: In our sample, satisfaction positively correlated with patients' expectation and satisfied patients were most likely to express preoperatively higher expectations. This is in fact the first study showing such interrelation with regard to elderly patients operated for LSS. The results are in accordance with earlier studies concluding that patients' expectations were the best predictor of patient satisfaction11 and that the extent to which expectations were met influenced the outcome in terms of satisfaction.7, 13 Another study20 concluded that expectations served as independent predictors of satisfaction but were not associated with patients' age, gender, marital status, or race. Our results, however, suggest that patients' age, gender and education level were the main determinants and were inversely related to patients' preoperative expectations. Certainly, high patients' expectations do not necessarily lead to high satisfaction levels, in particular, when they are initially high. It is possible that satisfaction does not result merely from meeting their expectations, but rather from other reasons.
(4) Satisfaction and postoperative function: Our data support recent findings21 on the nonsignificant correlation of satisfaction with postoperative ADL functioning. In a study similar to ours, Yamashita et al13 showed that subjective postoperative difficulty in walking and postoperative level of functioning were associated with patients' satisfaction, but were much less important compared with postoperative symptoms. We were unable to show significant interrelations between patients' walking ability or functional ADL status (either before surgery or on follow-up) and their levels of expectations or satisfaction.
(5) Role of age, gender and comorbidities: In our study, female gender was inversely related to patients' expectation of surgical success, and their postsurgical satisfaction rate was lower than that in males. Age positively related to patients' expectations and satisfaction, and this trend increased with advanced age. These data support other studies,22, 23 albeit in palliative-oncology, reporting that age and gender served as the most influential socio-demographic factors related to satisfaction. In addition, we have shown that the number of comorbidities (in particular, the presence of osteoarthritis, diabetes mellitus, and depression) did not adversely affect satisfaction. This contrasts results of previous studies reporting on association between these diseases and poor surgical outcome of spinal stenosis.24, 25
The present study has several limitations resulting from its relatively small number of participants, and those limitations related to its retrospective design, such as those related to data collection and outcome variable. In particular, the long-term span of patient enrollment may result in some differences in expectations and satisfaction rates, as well as a possible bias of consistency on the type of information that the participants may have retrieved preoperatively.
In conclusion, the current study suggests that patients' presurgical expectation and postsurgical satisfaction exhibit a complex relationship, influenced by multiple factors. Careful examination and characterization of expectations and their relations to postoperative satisfaction is required to improve the management of these patients, and to narrow existing gaps between preoperative expectations and postoperative satisfaction.
References
Garrity TF . Medical compliance and the clinician–patient relationship: a review. Soc Sci Med [E] 1981; 15: 215–222.
Guldvog B . Can patient satisfaction improve health among patients with angina pectoris? Int J Qual Health Care 1999; 11: 233–240.
Sanchez-Menegay C, Hudes ES, Cummings SR . Patient expectations and satisfaction with medical care for upper respiratory infections. J Gen Intern Med 1992; 7: 432–434.
Williams B . Patient satisfaction: a valid concept? Soc Sci Med 1994; 38: 509–516.
Buetow SA . What do general practitioners and their patients want from general practice and are they receiving it? A framework. Soc Sci Med 1995; 40: 213–221.
Hsieh MO, Kagle JD . Understanding patient satisfaction and dissatisfaction with health care. Health Soc Work 1991; 16: 281–290.
Williams S, Weinman J, Dale J, Newman S . Patient expectations: what do primary care patients want from the GP and how far does meeting expectations affect patient satisfaction? Fam Pract 1995; 12: 193–201.
Hall JA, Dornan MC . Patient sociodemographic characteristics as predictors of satisfaction with medical care: a meta-analysis. Soc Sci Med 1990; 30: 811–818.
Sorlie T, Sexton HC, Busund R, Sorlie D . Predictors of satisfaction with surgical treatment. Int J Qual Health Care 2000; 12: 31–40.
McMillan JR, Younger MS, DeWine LC . Satisfaction with hospital emergency department as a function of patient triage. Health Care Manage Rev 1986; 11: 21–27.
Yamashita K, Hayashi J, Ohzono K, Hiroshima K . Correlation of patient satisfaction with symptom severity and walking ability after surgical treatment for degenerative lumbar spinal stenosis. Spine 2003; 28: 2477–2481.
Keats AS . Classification status – a recapitulation. Anaesthesiology 1978; 49: 233–236.
Collin C, Wade DT, Davis S, Horne V . The Barthel Index: a reliability study. Int Disabil Stud 1988; 10: 61–63.
Hofman M et al. Cancer patients' expectations of experiencing treatment related side effects: a university of Rochester cancer center-community clinical oncology program study of 938 patients from community practices. Cancer 2004; 101: 851–857.
Welk TA, Smith Jr WB . Family surveys: measuring more than just satisfaction. Am J Hosp Palliat Care 1999; 16: 533–540.
Malacrida R et al. Reasons for dissatisfaction: a survey of relatives of intensive care patients who died. Crit Care Med 1998; 26: 1187–1193.
Rahmqvist M . Patient satisfaction in relation to age, health status and other background factors: a model for comparisons of care units. Int J Qual Health Care 2001; 13: 385–390.
Hargraves JL et al. Adjusting for patient characteristics when analyzing reports from patients about hospital care. Med Care 2001; 39: 635–641.
Da Costa D et al. The relationship between health status, social support and satisfaction with medical care among patients with systemic lupus erythematosus. Int J Qual Health Care 1999; 11: 201–207.
Mahomed NN et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol 2002; 29: 1273–1279.
Cohen G . Age and health status in a patient satisfaction survey. Soc Sci Med 1996; 42: 1085–1093.
Fakhoury WK, McCarthy M, Addington-Hall J . The effects of the clinical characteristics of dying cancer patients on informal caregivers' satisfaction with palliative care. Palliat Med 1997; 11: 107–115.
Lecouturier J, Jacoby A, Bradshaw C, Lovel T, Eccles M . Lay carers' satisfaction with community palliative care: results of a postal survey. South Tyneside MAAG Palliative Care Study Group. Palliat Med 1999; 13: 275–283.
Airaksinen O, Herno A, Turunen V, Saari T, Suomlainen O . Surgical outcome of 438 patients treated surgically for lumbar spinal stenosis. Spine 1997; 22: 2278–2282.
Arinzon Z, Adunsky A, Fidelman Z, Gepstein R . Outcomes of decompression surgery for lumbar spinal stenosis in elderly diabetic patients. Eur Spine J 2004; 13: 32–37.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gepstein, R., Arinzon, Z., Adunsky, A. et al. Decompression surgery for lumbar spinal stenosis in the elderly: preoperative expectations and postoperative satisfaction. Spinal Cord 44, 427–431 (2006). https://doi.org/10.1038/sj.sc.3101857
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101857
Keywords
This article is cited by
-
The dynamics of satisfaction in surgical and non-surgical adult spinal deformity patients
European Spine Journal (2021)
-
Exploring the expectation-actuality discrepancy: a systematic review of the impact of preoperative expectations on satisfaction and patient reported outcomes in spinal surgery
Neurosurgical Review (2018)
-
Is it safe to perform lumbar spine surgery on patients over eighty five?
International Orthopaedics (2017)
-
Influence of gender on patient-oriented outcomes in spine surgery
European Spine Journal (2016)
-
Patient satisfaction with double-door laminoplasty for cervical compression myelopathy
Journal of Orthopaedic Science (2015)