Abstract
Study design: Retrospective, descriptive study.
Objectives: To describe patients' length of stay (LOS), functional status and discharge setting after rehabilitation and how degree of impairment (complete/incomplete paraplegia/tetraplegia) impacts on these outcomes. To compare actual LOS with estimated LOS. Estimated LOS was based on an Australian model, the Australian National Sub-acute and Non-acute Patient Classification System (AN-SNAP), which classifies patients using admission Functional Independence Measure (FIM™) scores. To further describe outcomes for each AN-SNAP class by degree of impairment.
Setting: Spinal Injuries Unit of major Metropolitan hospital in Brisbane, Australia.
Methods: Retrospective chart review of 167 patients with traumatic spinal cord injury (SCI). Main outcome measures were rehabilitation LOS, discharge FIM™ scores and discharge setting. Injury measures were degree of impairment, acute LOS and rehabilitation admission FIM™ scores. Standard demographic measures were also collected.
Results: The median rehabilitation LOS was 83 days and mean discharge FIM™ scores 102 for all patients. These differed by impairment (incomplete paraplegia LOS 43, FIM 117; complete paraplegia LOS 96, FIM 109; incomplete tetraplegia LOS 64, FIM 100; complete tetraplegia LOS 206, FIM 78). Patients discharged to the community (noncare facility) ranged from 93% with incomplete paraplegia to 73% with complete tetraplegia. For patients in the three AN-SNAP classes with the lowest FIM scores, the actual LOS was up to twice the estimated LOS. A large variability in discharge outcomes was found within individual AN-SNAP classes, despite similar FIM™ scores on admission.
Conclusions: Rehabilitation outcomes differed substantially by impairment. The variability in outcomes for patients within the same AN-SNAP class questions the ability of this system to accurately predict LOS, and therefore cost of rehabilitation services, for patients with traumatic SCI in Australia.
Sponsorship: Some of this research was supported by a grant from Queensland Health. Leigh Tooth was supported by a National Health and Medical Research Council of Australia Public Health Fellowship (#997032) while some of this research was undertaken.
Similar content being viewed by others
Introduction
For patients with traumatic spinal cord injury (SCI), a complex interplay of sociodemographic and injury-related factors can impact on discharge outcomes such as length of stay (LOS), functional status and discharge setting following inpatient rehabilitation.1,2 Patients with low motor Functional Independence Measure (FIM™)3 scores on discharge are more dependent and are therefore more likely to be discharged to a long-term care facility.4,5,6 Those with high motor FIM scores on discharge are likely to return to community living on discharge, even though there may be a need for modification to the living environment to support independent living.4,5,6
As a result of such findings, an Australian classification system, termed the Australian National Sub-Acute and Non-Acute Patient Classification (AN-SNAP) system, has been developed to estimate the LOS for categories of rehabilitation patients.7 The AN-SNAP classification system was based on the analysis of data obtained from 4669 patients in overnight rehabilitation in 99 sites around Australia. Out of the 4669 patients, a sample of 88 with traumatic SCI was included in the analysis.7 For those with traumatic SCI, the classification of patients into AN-SNAP categories, and subsequent estimation of LOS, is based on patients' motor FIM scores on admission to rehabilitation. The AN-SNAP model has classified patients with traumatic SCI into four classes based on motor FIM scores. The classes and their estimated LOS are class 202 (admission motor FIM score=13, LOS=57.7 days), class 218 (admission motor FIM score=14–46, LOS=47.3 days), class 217 (admission motor FIM score=47–80, LOS=26.8 days) and class 216 (admission motor FIM=81–91, LOS=13.5 days).
Discharge outcomes are strongly influenced by severity and level of the injury. As the spinal cord lesion becomes more rostral and there is more extensive motor and sensory involvement, a person's level of functional independence decreases.2,8,9,10,11 As well as the level of the lesion, whether the injury is complete or incomplete has been used as a means of tracking patient outcomes, with complete lesions likely to have a more substantial impact on a patient's function, LOS and discharge setting.2,8,9,10,11
Recent research has identified limitations to the AN-SNAP model. Middleton et al12 documented significant differences in LOS and other discharge outcomes within AN-SNAP classes for patients with paraplegia or tetraplegia. Apart from this research and the original research that was conducted to generate the AN-SNAP model, there has been little research into this model. The fit between AN-SNAP-estimated LOS and actual rehabilitation LOS for patients with traumatic SCI within Australian hospitals requires further analysis, as a precursor to determining its suitability as a funding and clinical management tool.
In particular, it needs to be determined if the inclusion of other factors, such as injury type or degree of impairment (the completeness of the injury) in the model, would make it a more accurate predictor of LOS for patients with traumatic SCI.
This study aimed to:
-
1)
Describe patients' LOS, functional status and immediate setting on discharge from rehabilitation.
-
2)
Describe the effect of patients' degree of impairment on these outcomes.
-
3)
Compare patients' actual LOS with AN-SNAP-estimated LOS.
-
4)
Describe patients' actual LOS, functional status and immediate discharge setting for each impairment type within each AN-SNAP class.
Methods
Design
This was a retrospective study based on a review of the subjects' occupational therapy chart.
Subjects and setting
Subjects were patients admitted to the Spinal Injuries Unit (SIU) of a major metropolitan public hospital in Australia between 1st January 1993 and 31st December 1998. This SIU manages patients during both the acute and rehabilitation phases of their admission. During the study period, a transitional rehabilitation programme was introduced. This is a multidisciplinary rehabilitation programme that assists with the transition from inpatient rehabilitation to the community by providing ongoing rehabilitation in a home-like environment. The programme operates in the individual's own home if he or she lives within a defined distance from the SIU or supplies fully wheelchair accessible accommodation and personal care for the patient (at no cost to the individual) who lives a greater distance from the SIU.
For the purposes of FIM scoring within the SIU and for this study, rehabilitation LOS was calculated from the date of the patient's mobilisation from bed (ie the patient no longer immobilised in bed and attends occupational or physiotherapy regularly) to date of discharge. FIM scoring within the SIU was completed by occupational therapists who had acquired accredited FIM training.
Ethical approval for the study was obtained from the relevant hospital and University Ethics Committees.
Inclusion/exclusion criteria
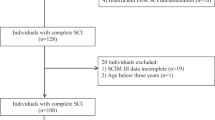
Subjects on their initial admissions with SCI of traumatic origin were included. Subjects whose SCI was of nontraumatic origin or who were not admitted for their initial episode were excluded. Since FIM scoring at the institution was completed solely by occupational therapists, only those subjects who attended occupational therapy as part of their rehabilitation had available FIM data. Of a total of 587 patients admitted to the SIU during the study period, 367 had an initial traumatic SCI and were seen by an occupational therapist and were therefore eligible to be included in the study.
A further 199 subjects were excluded because of missing FIM data, that is having total FIM scores rather than individual FIM item scores recorded in the occupational therapy charts. One subject died before discharge and was excluded. Complete FIM data were available for 167 subjects, 45.5% of the eligible sample.
Representativeness of sample
Owing to the high percentage of charts with missing FIM item scores, the final useable sample was compared to a database of all patients admitted to the SIU during a similar time period, that is July 1993 to June 1998 (n=446), on a number of demographic and injury characteristics (see Table 1). The database contained all first traumatic and nontraumatic admissions. It was not possible to separate out the nontraumatic injuries, which comprised 14.4% of the data set. The two samples were compared on age and total LOS using the one-sample t-test, and on gender, place of residence (SIU catchment area, other State of Australia/overseas) and degree of impairment (complete/incomplete paraplegia, complete/incomplete tetraplegia) using the χ2-goodness-of-fit statistic for a known distribution. There was no difference between the sample and total population on age, gender or LOS. There was a significant difference χ(1)2=7.0, P<0.01, for place of residence, with the sample containing proportionally more people from other Australian States and overseas. This probably reflected the fact that the sample contained only people with traumatic injuries, which may have been sustained while they were visiting this Australian State. There was also a significant difference χ(3)2=23.6, P<0.05, for degree of impairment, in that the sample had proportionally more people with incomplete tetraplegia and proportionally fewer with incomplete paraplegia. This may have reflected the incidence of nontraumatic injuries in the data set and that patients with specific injury types may have been more likely to be seen by an occupational therapist.
Data collection
Data collection, including demographic, injury severity and discharge data using a standardised collection form was completed by the first two authors between July and October 2000. Demographic measures collected were age (years), gender, marital status (single, married/defacto, widowed or divorced), preinjury living setting (community dwelling [house or apartment], hospital, hostel [assisted living], or skilled nursing care facility), preinjury living situation (living alone, with family/relatives or friends), employment status (employed, student, homemaker, not working, retired for age or disability) and usual place of residence on admission (SIU catchment area, other state of Australia or other country).
Injury severity variables were degree of impairment (complete/incomplete paraplegia or complete/incomplete tetraplegia according to the Frankel Grading System, with complete injuries being Frankel grade A and incomplete injuries Frankel grades B–E), acute LOS and admission (to rehabilitation) FIM scores. The FIM is a valid and reliable measure of function, which consists of 18 items that estimate the individual's care burden when summed. It yields two domain scores, motor (range 13–91) and cognitive (range 5–35), where lower scores indicate a greater level of disability or dependence.3
Variables measured on discharge were rehabilitation LOS (number of overnight stays), immediate discharge living setting (same community dwelling as living in preadmission, different community dwelling as living in preadmission, interim community dwelling funded by the SIU as part of a transitional rehabilitation programme to enable supported reintegration to the community, hospital, hostel, skilled nursing care facility), immediate discharge living situation (as above) and discharge FIM scores.
The demographic and injury severity details of the 167 patients included in the study are shown in Table 1, Table 2 and Table 3.
Data analysis
Descriptive statistics, analysed through SPSS (version 10), were used to report demographic, injury severity and discharge outcome variables. Owing to small cell sizes in some levels of the discharge living setting variable, only descriptive statistics could be used to present this outcome by LOS, functional status and degree of impairment. The relation between LOS and place of residence was also presented descriptively. One-way ANOVA was used to analyse the relation between LOS and discharge functional status and degree of impairment, with the least significance difference used for post hoc comparison tests. For the variable LOS, medians and interquartile ranges (IQR) were usually presented because of skewness of the data. However, where actual LOS was compared to AN-SNAP estimated LOS, means are used so the scores could be directly compared. To compare AN-SNAP estimated LOS with actual LOS for each of the AN-SNAP classes (202, 216, 217, 218), the one-sample t-test procedure in SPSS was used when there were enough cases in each category. The one-sample t-test procedure tests whether the mean of a single variable differs from a specified constant. In these, 95% confidence intervals of the differences were also presented.
Results
Length of stay
The median rehabilitation LOS for the total group was 83.0 days (IQR 35–139, range 3–317) (see Table 4). When LOS was considered for patients discharged to different discharge settings, the median rehabilitation LOS was longest for the two patients discharged to a hostel. Median LOS was shortest for those discharged to the same community dwelling, another hospital or a skilled nursing care facility.
Results comparing LOS to patients' place of residence revealed that patients from the SIU catchment area (n=150) had a median rehabilitation LOS of 89.0 days (IQR=39–141, range 3–317). For patients from other states of Australia (n=12), the median LOS was much lower at 58.0 days (IQR 25–103, range 16–204). Patients from other countries (n=5) had a median LOS of 37.0 days (IQR 16–134, range 3–205).
Rehabilitation LOS was significantly longer for patients with complete tetraplegia compared to incomplete tetraplegia or incomplete/complete paraplegia F(3,163)=13.4, P=0.000 (see Table 4). Post hoc analyses revealed that all of these pairwise differences were significant at P≤0.000.
Discharge functional status
The mean total FIM scores increased from 68.7 on admission to 102.2 (SD=22.9, range 30–126), a gain of 33.2 points. This gain was almost entirely because of improvement in mean motor FIM scores. There was only a small change in mean cognitive FIM scores (see Table 3).
Mean discharge motor FIM scores for different discharge settings are presented in Table 4. Mean motor FIM scores on discharge appeared to be similar for patients who were discharged to the same or a different community dwelling or hostel and lower for those discharged to a skilled nursing care facility, other hospital or the transitional rehabilitation programme.
Results for degree of impairment showed that mean discharge total FIM scores were highest for patients with incomplete paraplegia at 117.4 (SD 5.5, range 102–126) and lowest for those with complete tetraplegia at 77.9 (SD 19.2, range 48–113) F(3,157)=17.1, P≤0.000. Post hoc analyses showed significant differences in mean discharge total FIM scores between people with incomplete paraplegia and incomplete (P≤0.000) and complete (P≤0.000) tetraplegia. Significant differences were also found between people with complete paraplegia and incomplete (P≤0.030) and complete (P≤0.000) tetraplegia, and between those with incomplete and complete tetraplegia (P≤0.000). Patients with complete tetraplegia were also found to have the least change in FIM score between admission and discharge (see Table 4).
Discharge living setting and situation
Changes in living setting from admission to discharge are presented in Table 2. The majority of patients (75.4%) were discharged to the same or a different community dwelling with the next largest group going to the transitional rehabilitation programme (10.8%). In all, 10% were discharged to another hospital with only a very small percentage being discharged to a hostel or a skilled nursing care facility. For those discharged to the transitional rehabilitation programme, the intended final living setting was always the community.
Table 2 also shows that of those who were discharged to the community (n=126), most (80.2%) returned to live with family or relatives, with 7.1% living alone and 7.9% with friends. An additional 4.8% lived alone but received community support services such as domiciliary nursing. When compared with preadmission living setting and situation a total of 48.5% of subjects changed either living setting or situation immediately on discharge.
Results for the degree of impairment showed that the percentage of patients discharged to the community (same, different or interim dwelling) decreased from 92.6% for those with incomplete paraplegia to 72.7% for those with complete tetraplegia (Figure 1). Those individuals with incomplete paraplegia appeared to be more likely than those with complete tetraplegia to return to the same community dwelling as prior to their injury (66.6 versus 45.4%).
Analysis of AN-SNAP classes: comparison between estimated and actual LOS and discharge functional status
AN-SNAP estimated versus actual LOS was compared using the one-sample t-test (Table 5). For AN-SNAP classes 202, 218 and 217 there were significant differences between the estimated and actual LOS with the most significant differences being found in class 218 where the actual LOS was more than twice that estimated by AN-SNAP. No statistical comparison was possible for class 216 because of the small sample size.
There were also marked differences found in the distribution of subjects within AN-SNAP classes with 66% of subjects falling into AN-SNAP class 218 at admission but only 2.9% in class 216.
As illustrated in Table 5, the mean discharge FIM scores for AN-SNAP classes progressively increased across the classes, from a minimum of 78.4 (SD 30.7, range 30–126) for class 202 to a maximum in class 216 of 123.4 (SD 3.6, range 119–126).
Discharge outcomes by degree of impairment within each AN-SNAP class: LOS, functional status and immediate discharge setting
Although the analyses for classes 202, 218 and 217 showed a statistical difference between estimated and actual LOS for the group of patients as a whole, the breakdown of LOS by AN-SNAP class and degree of impairment demonstrated further the variation within AN-SNAP classes in LOS (see Table 6). Differences between high and low median LOS values for degree of impairment categories within the AN-SNAP classes 202, 218 and 217 of up to 89, 150.5 and 69 days, respectively, were found.
Class 202 consisted predominantly of patients with tetraplegia (16 of 17 patients). LOS and discharge motor FIM scores were variable across the impairment types despite similar motor FIM scores on admission. Despite their high degree of disability on admission only two patients (15.4% of class 202) were discharged to a nursing care facility or hostel.
Class 218 contained the majority of subjects (n=110) and all impairment types were well represented. Median LOS was shorter for incomplete injuries and mean discharge FIM scores decreased across the four categories of impairment, despite the uniformity in admission motor FIM scores across all patients. The percentage of patients discharged to the community (same, different or interim dwelling) was high overall, but decreased across the categories from 92% for incomplete paraplegia to 78% for complete tetraplegia.
Class 217 (n=35) consisted predominantly of patients with incomplete injuries (80%). This class revealed the most consistency in mean discharge FIM scores. Discharge to a community dwelling was the norm in this class and no patients were discharged to a long-term care facility.
Analysis of AN-SNAP class 216 is difficult because of extremely small numbers in this class (n=5). All subjects had incomplete injuries, short LOS, high discharge FIM scores and all returned to a community dwelling.
Discussion
This study documented the discharge outcomes (LOS, functional status on discharge and immediate discharge setting) of patients admitted with traumatic SCI over a 5-year interval. Comparisons were made between AN-SNAP-estimated LOS and actual LOS. Variability in outcomes based on the degree of impairment within specified AN-SNAP classes was identified.
The demographic profile of the 167 patients included in this study, namely that they were mostly young, male, single and employed, is consistent with the profiles reported in other studies of patients with spinal cord injury, both overseas6,13,14 and in Australia.9,12,15,16
Discharge outcomes: LOS, functional status and discharge setting
The documentation of rehabilitation LOS as an outcome measure has escalated in recent decades. This has enabled researchers and clinicians to evaluate and compare the efficiency and effectiveness of rehabilitation interventions against national and international benchmarks. In the present study, while LOS varied considerably by degree of impairment, it was generally consistent with figures reported from other Australian SCI Units.9,12,15,16 The LOS reported in the current study would, however, appear to be longer than figures reported in US studies.10,17 However, some caution is needed when directly comparing LOS between different countries because LOS can be driven by other factors such as health systems management and financial considerations. For example, LOS in the US has decreased so much over the last 10 years, driven by a combination of factors including managed care, that authors are questioning the link between this and the corresponding increase in incidence of rehospitalization rates and numbers of patients with SCI being discharged into nursing care facilities instead of home.10
The shorter median LOS found in this study for patients whose place of residence was in other states of Australia or other countries was not unexpected as these individuals were usually discharged as soon as possible to an SCI Unit closer to their home to complete rehabilitation.
The finding that the median rehabilitation LOS was shorter for patients with incomplete and more caudal injuries may be explained by the influence of multiple inter-related factors. These include: the greater potential for neurological recovery in incomplete injuries, the ability to reach a degree of independence (higher discharge FIM scores) sufficient for discharge at an earlier stage in the rehabilitation programme and the ability to move from an inpatient to an outpatient rehabilitation programme sooner.11
The increase in mean total FIM scores (68.7–102.2) and mean motor FIM scores (35.3–67.3) for the patients from admission to discharge is consistent with the gains documented in other studies.11,12,14,18 For example, Ditunno et al18 reported that people with traumatic SCI generally have a mean total FIM score of 59.5 on admission and 95.3 on discharge (mean gain of 35.9), and a mean motor FIM score of 28.6 on admission and 62.1 on discharge (mean gain of 33.5). Data from the United Data System for Medical Rehabilitation (UDSMR) for SCI admissions during 1995–1997, with corresponding sample sizes of 3444, 4337 and 4652 cases, showed lower discharge FIM total scores (means of 89.8 to 88.8 over the 3 years, respectively) and lower FIM gains (mean of 26 for 1997) than patients showed in the present study.17 The total and motor FIM gains for patients in this study were 33.2 and 32.0 points, respectively, indicating that almost all of the gain occurred in the motor component. The results of this study confirm that patients with traumatic SCI generally present with high cognitive FIM scores on admission and discharge. The FIM has been previously shown to be relatively insensitive to changes that may occur in cognitive function in this group of patients.11
Research has highlighted that FIM score gain is related to the neurological level and severity of the injury.5,11,12,18 In view of this, the descriptive profile of patients in the present study would appear to be relatively consistent with the SCI literature, where patients with complete and more rostral injuries were found to have lower motor FIM scores on discharge. In this study, patients with complete tetraplegia showed the least improvement in their FIM scores from admission to discharge.
Discharge to the community is another indicator of a successful outcome and may be closely related to injury severity, functional status on discharge and LOS. Although the discharge setting of patients following rehabilitation for traumatic SCI has been previously studied in the US,1,4,6,19 there is a paucity of similar Australian information. The majority of patients in this study (86.2%) were discharged back to the community (same, different or interim dwelling), which is similar to previous findings in the literature indicating a range between 80 and 95%.1,4,17 Research has also shown that between 3.1 and 10% of patients are discharged to skilled nursing care facilities and between 1.4 and 5% to another hospital.1,4,17 In this study, 2.4% were discharged to a skilled nursing care facility and 10.2% to another hospital. In a study of outcomes of 4652 patients with traumatic SCI in 1997 using data from the UDSMR, Fiedler et al17 reported three times as many patients being discharged into nursing care as was recorded in the present study. These patients also showed lower discharge FIM scores and shorter LOS figures, perhaps accounting for this finding.
There is also limited literature that documents the number of patients with traumatic SCI who change living setting or situation from admission to discharge. In the present study, almost half of the patients were found to have a change in living setting or situation on discharge.
Previous research has shown that the typical reasons why people are discharged to a skilled nursing care facility or another hospital is because of the severity of their disability, the need for supervision or support or the need to be closer to family support.4,19 Typically, patients discharged to another hospital in this study were those whose place of residence was in another state or country and who were discharged to a hospital closer to home to continue rehabilitation. Furthermore, patients discharged to a skilled nursing care facility or another hospital had a lower mean motor FIM score on discharge than patients discharged to a community dwelling. This indicates that patients with low motor FIM scores require proportionally more daily assistance than those with high motor FIM scores, thus reflecting the utility of the FIM in identifying burden of care.5,20
Patients with a greater degree of impairment at admission (complete tetraplegia versus incomplete paraplegia) were also less likely to be discharged to the community, especially to the same dwelling. This result is in keeping with the lower discharge FIM scores and smaller FIM gains found in those with greater impairment.
Comparison between AN-SNAP-estimated and actual LOS
Comparison between actual and AN-SNAP-estimated LOS in the current study revealed that patients with high motor FIM scores (81–91) on admission (AN-SNAP class 216) had an LOS similar to that estimated by AN-SNAP. However, the small number of patients in this class makes reliable analysis difficult. Patients with low motor FIM scores on admission (AN-SNAP classes 202 and 218) were found to have a mean rehabilitation LOS approximately twice as long as the AN-SNAP estimated LOS. The results were similar for AN-SNAP class 217. These differences between estimated and actual LOS may indicate that while the AN-SNAP classification system may be accurate in predicting the overnight rehabilitation needs for patients with high motor FIM score on admission, it may underestimate the LOS of patients who have a low-to-mid-functional status on admission.
As noted previously, development of the AN-SNAP classes for patients with traumatic SCI was based on a sample of only 88 patients. In addition to this small sample size, the data collection time period used for the classification system was only 3 months although some specialist SCI and brain injury units continued data collection for 6 months. Since subjects needed to be both admitted and discharged within the data collection period to be included, even this longer timeline may have omitted or under-reported patients with complete or more rostral spinal cord injuries who would have been likely to have a longer LOS.
The discrepancy between the actual and the AN-SNAP-estimated LOS might also be because of the fact that functional status on admission is not a sufficient indicator of LOS. It may be necessary to investigate the impact of other factors, which are independent of and not measured by the AN-SNAP classification system, that may affect LOS, and to consider these effects together with admission motor FIM scores. Furthermore, given the large number of data collection sites across Australia that were used in the AN-SNAP study, it is possible that interfacility variation would occur. For example, facilities may differ on the degree to which they provide more intensive or extensive inpatient rehabilitation services.
Discharge outcomes by injury type within each AN-SNAP class
When the outcomes of LOS, discharge motor FIM scores and discharge setting were considered by the degree of impairment within each AN-SNAP class, there was a substantial variability in outcome, particularly for patients with low admission motor FIM scores (class 218).
Patients with the lowest admission motor FIM scores (class 202) predominantly had tetraplegia and all but two failed to return to their previous community dwelling, instead requiring further hospital care, nursing care or different housing.
Class 218 or those with low admission motor FIM scores contained the majority of patients and most of those with tetraplegia, although all four impairment categories were well represented. Although median LOS increased and mean discharge motor FIM scores decreased with more complete and rostral injuries, there was substantial variability in discharge setting across impairment types. These findings are supported by Stineman et al,11 who reported the most variable outcomes for patients with low-admission motor FIM scores. These researchers reported that patients in this FIM range have outcomes spanning the whole spectrum from total dependence to total independence. As well as differences in underlying pathology, this variability in outcome may also reflect such factors as the presence of social support and a committed carer, as well as financial access to a motorised wheelchair, paid assistance and home modifications.
The majority of patients with mid-admission motor FIM scores (class 217) had incomplete lesions and none were discharged into skilled nursing care facilities. Patients with high-admission motor FIM scores (class 216) all had incomplete lesions and a short LOS, and all were discharged to the community.
From the results of this study, it would appear that admission motor FIM score, and classification of patients into AN-SNAP classes based on this, might not be the best basis on which to predict outcomes for SCI patients such as LOS and discharge setting. While those with the highest- and lowest-admission motor FIM scores appear to have a fairly predictable outcome, those with low- and mid-admission motor FIM scores have a more variable outcome. Consideration of the actual level and completeness of the injury may provide a more accurate basis on which to predict LOS.9,21 For example, when considering tetraplegia, the functional ability of an individual with an injury at the fourth cervical spinal segment compared to an individual with a lesion at the eighth cervical spinal segment would be substantially different. Furthermore, considering patients' social and financial situation may also assist with predicting outcomes.
Limitations
Limitations of this study include that it was based on retrospective data collected from a single centre and that although the sample was found to be representative of all patients admitted to the unit on age, gender and LOS, it was different in terms of the percentage of patients with incomplete injuries and the percentage from outside the Australian State in which the SIU was located. The discharge outcomes for patients with nontraumatic SCI have not been investigated in this study. This group warrants further investigation.
Conclusion and implications for further research
This study supports several common patterns pertaining to discharge outcomes of patients with traumatic SCI that have been previously documented in the literature. For SCI clinicians, knowledge of these patterns may assist with rehabilitation and discharge planning. Further investigation of discharge outcomes in Australian SCI units would be informative.
In view of this study's findings, the current AN-SNAP classification system may not adequately predict inpatient rehabilitation LOS for patients with traumatic SCI. Further research on the appropriateness and accuracy of the AN-SNAP classification system for patients with SCI is required, prior to consideration of its adoption as a formal prospective funding and clinical management tool for these patients.
Additional research is also needed to investigate how clinical service providers might adequately address the cost containment and other demands proposed by prospective funding systems and policy makers, while maintaining and improving high-quality outcomes for SCI patients.
References
DeVivo MJ . Discharge disposition from model spinal cord injury care system rehabilitation programs. Arch Phys Med Rehabil 1999; 80: 785–790.
Saboe LA, Darrah JM, Pain KS, Guthrie J . Early predictors of functional independence 2 years after spinal cord injury. Arch Phys Med Rehabil 1997; 78: 644–650.
Hamilton BB, Laughlin JA, Fiedler RC, Granger CV . Interrater reliability of the 7-level Functional Independence Measure. Scand J Rehabil Med 1994; 26: 115–119.
Dijkers MP, Buda Abela M, Gans BM, Gordon WA . The aftermath of spinal cord injury. In: Stover SL, DeLisa JA, Whiteneck GG (eds). Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen: Gaithersburg, MD, 1995, pp 185–212.
Dodds TA, Martin DP, Stolov WC, Deyo RA . A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil 1993; 74: 531–536.
DeVivo MJ et al. Trends in spinal cord injury demographics and treatment outcomes between 1973 and 1986. Arch Phys Med Rehabil 1992; 73: 424–430.
Eager K et al. The Australian National Sub-Acute and Non-Acute Patient Classification (AN-SNAP): Report of the National Sub-Acute and Non-Acute Casemix Classification Study. Centre for Health Service Development: University of Wollongong, 1997.
Lazar R et al. Prediction of a functional outcome by motor capability after spinal cord injury. Arch Phys Med Rehabil 1989; 70: 819–822.
Middleton JW, Truman G, Geraghty TJ . Neurological level effect on the discharge functional status of spinal cord injured persons after rehabilitation. Arch Phys Med Rehabil 1998; 79: 1428–1432.
Eastwood EA et al. Medical rehabilitation length of stay and outcomes for persons with traumatic spinal cord injury 1990–1997. Arch Phys Med Rehabil 1999; 80: 1457–1463.
Stineman MG et al. Functional gain and length of stay for major rehabilitation impairment categories: patterns revealed by function related groups. Am J Phys Med Rehabil 1996; 75: 68–78.
Middleton J, Truman G, Cameron I, Perry G . Effect of admission class and impairment type on length of stay for SCI patients in AN-SNAP classes 217 and 218. Conference Proceedings of the 7th Annual Scientific Meeting of the Australasian Faculty of Rehabilitation Medicine, 1999.
Waters RL, Adkins RH, Yakura JS, Sie I . Motor and sensory recovery following complete tetraplegia. Arch Phys Med Rehabil 1993; 74: 242–247.
Müslümanoglu L et al. Motor, sensory and functional recovery in patients with spinal cord lesions. Spinal Cord 1997; 35: 386–389.
Cripps R, O'Connor P . Spinal cord injury, Australia 1996/97. Australian Injury Prevention Bulletin (18, AIHW Cat. No. INJ013, April 1998). Research Centre for Injury Studies, Flinders University of South Australia: Adelaide, 1998.
O'Conner P, Cripps R . Spinal cord injury, Australia 1997/98. Australian Injury Prevention Bulletin (21, AIHW Cat. No. INJ19, December 1998). Research Centre for Injury Studies, Flinders University of South Australia: Adelaide, 1998.
Fiedler RC, Granger CV, Russell CF . Uniform data system for medical rehabilitation: report of first admissions for 1997. Am J Phys Med Rehabil 1998; 77: 444–450.
Ditunno JF, Cohen ME, Formal C, Whiteneck GG . Functional outcomes. In: Stover SL, DeLisa JA, Whiteneck GG (eds). Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen: Gaithersburg, MD, 1995, pp 170–184.
Roth EJ et al. The older adult with a spinal cord injury. Paraplegia 1992; 30: 520–526.
Hamilton BB et al. Relation of disability costs to function: spinal cord injury. Arch Phys Med Rehabil 1999; 80: 385–391.
Ota T et al. Functional assessment of patients with spinal cord injury: measured by the motor score and the functional independence measure. Spinal Cord 1996; 34: 531–535.
Acknowledgements
We acknowledge Mrs Kellie Bowden and Julie Connell for their contributions to an earlier phase of this research.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tooth, L., McKenna, K. & Geraghty, T. Rehabilitation outcomes in traumatic spinal cord injury in Australia: functional status, length of stay and discharge setting. Spinal Cord 41, 220–230 (2003). https://doi.org/10.1038/sj.sc.3101433
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101433
Keywords
This article is cited by
-
Rehabilitation length of stay and functional improvement among patients with traumatic spinal cord injury
Spinal Cord (2022)
-
Retrospective trends in length of stay and bowel management at discharge from inpatient rehabilitation among individuals with spinal cord injury
Spinal Cord (2022)
-
Risk indicators of length of acute hospital stay after traumatic spinal cord injury in South Africa: a prospective, population-based study
Spinal Cord (2019)
-
The delivery of specialist spinal cord injury services in Queensland and the potential for telehealth
BMC Health Services Research (2015)
-
Traumatic spinal cord injuries: evidence from 30 years in a single centre
Spinal Cord (2014)