Abstract
OBJECTIVE:
To determine the prevalence of low cortisol values and to evaluate clinical responses to hydrocortisone in ill term and near-term newborns.
STUDY DESIGN:
Retrospective cohort study including infants ≥35 weeks gestational age who were mechanically ventilated, received vasopressor therapy, and had a cortisol concentration obtained for evaluation of vasopressor-resistant hypotension. In those infants treated with hydrocortisone, physiologic responses were evaluated and correlated with cortisol values (<15 vs ≥15 μg/dl).
RESULTS:
A total of 32 infants had cortisol values obtained; 18 (56%) were <15 μg/dl. In all, 21 infants were treated with hydrocortisone of whom 13 had cortisol values <15 μg/dl. These 13 infants showed decreased heart rate, dopamine support and fluid bolus requirements after treatment, compared to infants with values ≥15 μg/dl (n=8).
CONCLUSIONS:
A significant number of hypotensive, mechanically ventilated infants have evidence of inadequate adrenal function. Hydrocortisone therapy resulted in hemodynamic stabilization in this population.
Similar content being viewed by others
INTRODUCTION
Hypotension resulting in the use of volume expanders and vasopressor therapy is a frequent occurrence in critically ill term and near-term newborns. Many of these infants remain hypotensive and poorly perfused even after institution of these therapies. In other critically ill patient populations, vasopressor-resistant hypotension has been linked to a functional or “relative” adrenal insufficiency. Although absolute adrenal insufficiency is rare, relative adrenal insufficiency in the face of severe illness may be much more common. Small studies, using various criteria, have estimated the incidence of relative adrenal insufficiency in critically ill adults and children to be between 3 and 56%.1, 2, 3, 4, 5, 6, 7, 8 Cardiovascular instability with vasopressor-resistant hypotension is a primary manifestation of relative adrenal insufficiency, which has been associated with morbidity and mortality.3, 4, 5, 6, 8, 9, 10, 11
Adult patients with relative adrenal insufficiency and cardiovascular instability respond to glucocorticoid replacement therapy with improvement in blood pressure and decreased vasopressor support.11, 12, 13 A large randomized trial recently demonstrated that hydrocortisone therapy decreased mortality in adults with septic shock and relative adrenal insufficiency.14 In preterm infants, several studies have correlated hypotension with low cortisol values and have shown that blood pressure improves in response to glucocorticoid therapy.15, 16, 17, 18, 19, 20 However, to our knowledge, only one study has measured low cortisol levels and response to glucocorticoid therapy in a small series of hypotensive term infants.21
The aim of this observational study was to examine a cohort of term and near-term infants with hypotension refractory to fluid and vasopressor therapy and to (1) evaluate clinical responses to hydrocortisone, (2) determine the prevalence of basal cortisol values that meet criteria for relative adrenal insufficiency in children and adults (cortisol <15 μg/dl)2, 11 and (3) determine whether there is a significant difference in response between infants whose cortisol values are <15 μg/dl compared with those ≥15 μg/dl.
METHODS
Patient Population
This study was approved by the institutional review board of the University of New Mexico Health Sciences Center. The clinical database of the University of New Mexico (UNM) Children's Hospital was used to identify all infants ≥35 weeks gestational age (GA) admitted to the neonatal intensive care unit between November 1, 2000 and August 1, 2002 who received mechanical ventilation and vasopressors. During this time period, intravenous hydrocortisone (1 to 2 mg/kg/day) was given at the discretion of the attending neonatologist to treat infants with hypotension unresponsive to fluid boluses and vasopressor support. The hydrocortisone was discontinued when the attending neonatologist deemed the patient cardiovascularly stable. Prior to the administration of hydrocortisone, cortisol values were routinely obtained.
Study Procedures
Data collected from nursing bedside flowsheets included mean arterial blood pressure, heart rate, vasopressor support (dopamine and dobutamine), fluid boluses for volume expansion, and urine output for the 12 hours prior to and 24 hours after initiation of hydrocortisone therapy. Heart rate and blood pressure were averaged over 4-hour time intervals. Fluid boluses and urine output were averaged over the 12 hours before and 24 hours after hydrocortisone. Mean arterial blood pressures were measured by umbilical or peripheral arterial catheters connected to pressure transducers and/or oscillometry. The maximum dopamine and dobutamine infusion rate during each 4-hour time interval was recorded. Serum cortisol concentrations were measured in the clinical laboratory of the UNM Hospital by competitive binding immunoenzymatic assays.
Statistical Analysis
The clinical responses to hydrocortisone were first evaluated in all study infants. Then, based on the proposed definition of presumptive relative adrenal insufficiency in acutely ill children and adults (random cortisol <15 μg/dl),2, 11 the infants were divided into two groups: infants with cortisol values <15 μg/dl and infants with cortisol values ≥15 μg/dl. The clinical responses to hydrocortisone in each group were evaluated and the groups compared by analysis of repeated measures over time using random coefficient regression22 in PROC MIXED in SAS (SAS/STAT, Version 8, Cary, NC, 1999). This analysis allows each subject to have its own trajectory over time, and flexibly models the covariance structure of random effects and within-subject variability over time. Two-sample t-test was used to compare the duration of hydrocortisone treatment between groups. Paired t-test was used to compare fluid bolus administration and urine output before and after hydrocortisone treatment. Data are presented as mean±standard deviation unless otherwise noted. The level of significance was set at p<0.05.
RESULTS
Between November 2000 and August 2002, 673 infants ≥35 weeks GA were admitted to the UNM neonatal intensive care unit. A total of 169 infants were supported with mechanical ventilation, and 73 (43%) of these were treated with vasopressors. Of these 73 infants, 32 (44%) had cortisol values obtained because they were considered to be refractory to vasopressor therapy. Population characteristics and cortisol values for these 32 patients are shown in Table 1. Nine of the infants subsequently stabilized without hydrocortisone therapy, while 23 were treated with hydrocortisone. Three of the infants not treated with hydrocortisone had cortisol values <15 μg/dl. These infants were not apparently different from the other infants, (one meconium aspiration syndrome, one respiratory distress syndrome, one aortic stenosis). These three infants had cortisol values ranging from 7 to 11.8 μg/dl and all survived to discharge.
Of the 23 patients treated with hydrocortisone, 21 charts were available for review of the physiologic responses and relationship to cortisol concentration. The infants were divided into those with cortisol concentrations <15 μg/dl (n=13) and those ≥15 μg/dl (n=8). Table 2 shows that infants whose cortisol values were <15 μg/dl received hydrocortisone longer than those whose cortisol values were ≥15 μg/dl (p<0.05).
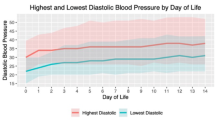
Figure 1 shows the clinical responses of these two groups of infants to hydrocortisone therapy. For blood pressure (Figure 1a), a linear trend was fit from baseline (average of 4 hours of data just prior to hydrocortisone administration) through 24 hours with interaction between trend and groups. The analysis of repeated measures over time showed the same overall increasing trend from baseline through 24 hours after hydrocortisone for both groups (slope=0.20, p=0.011). The interaction (p=0.73) and group effect (p=0.53) was not significant after hydrocortisone.
(a) Blood pressure, (b) heart rate and (c) dopamine infusion from 12 hours before to 24 hours after initiating hydrocortisone therapy are shown, separated into infants whose cortisol values were <15 μg/dl (▴, n=13) and infants whose cortisol values were ≥15 μg/dl (○, n=8). Baseline is the average of 4 hours of data just prior to hydrocortisone administration (vertical line). Data are presented as mean±SEM.
For heart rate (Figure 1b), from baseline through 24 hours, there was a significant overall decreasing trend down over time (p=0.0003) and a significant group effect (p=0.03) but no significant group × time interaction. The most notable feature, however, is the apparent between-group visual difference from 0 to 16 hours. Modeling a linear trend over that time period showed a significant group x time interaction such that for those infants with cortisol concentrations <15 μg/dl, heart rate significantly decreased (p=0.04) while heart rate did not change significantly over that time period for infants with cortisol values ≥15 μg/dl.
For dopamine (Figure 1c), modeling is complicated by a clear jump from baseline for the group with cortisol values ≥15 μg/dl. Modeling this properly would require somewhat more data than we have. Therefore, we restricted analysis to 0 to 12 hours. Within that time frame, modeling linear trends for groups showed significant decrease in dopamine both groups (p=0.0005) and a significant group effect (p=0.04), with the group with cortisol concentrations <15 μg/dl showing lower dopamine support after hydrocortisone. Only five patients in each group received dobutamine in addition to dopamine. Although the visual trend was downward, the small sample size precluded significant statistical analysis.
Infants with cortisol values <15 μg/dl required significantly fewer fluid boluses in the 24 hours after beginning hydrocortisone compared to the 12 hours before treatment (3.4±3.6 vs 8.8±9.4 cm3/kg, p=0.02). Infants with cortisol values ≥15 μg/dl showed no change after treatment (15±9.9 vs 10±12.8 cm3/kg, p=0.4). There was no change in urine output after hydrocortisone in either group.
DISCUSSION
In this retrospective review of a cohort of mechanically ventilated term and near-term infants, we found that a high percentage of these critically ill infants — 43% — received vasopressor support for hypotension. Of these, almost half were considered resistant to vasopressor therapy and therefore had cortisol values obtained. More than half of the cortisol concentrations obtained met the criteria for the diagnosis of relative adrenal insufficiency in critically ill children and adults. Applying this definition to our population would suggest a prevalence of relative adrenal insufficiency of at least 25% (13/73) in the infants receiving vasopressors during this time period. This is consistent with the incidence of adrenal insufficiency reported in other critically ill populations.1, 2, 3, 4, 5, 6, 7, 8 The prevalence of relative adrenal insufficiency in this infant population may have been higher, since some critically ill patients have cortisol values >15 μg/dl but still show inadequate response to ACTH stimulation.11
We did not observe any adverse events attributable to hydrocortisone in this study, such as hypertension or gastrointestinal bleeding. The dose of hydrocortisone used in our institution is lower than many texts recommend for older patients23 and is based on an anticipated decreased metabolic clearance in newborns.
While there may not be agreement on the cutoff value to define adrenal insufficiency in the stressed term newborn, we have no a priori reason to accept a lower cutoff value than for children and adults. In this study, infants with cortisol values <15 μg/dl showed significant improvement in blood pressure and heart rate, as well as a decreased need for dopamine and fluid support after hydrocortisone therapy, while infants with cortisol values ≥15 μg/dl continued to have higher heart rates, require higher dopamine infusion rates and more fluid boluses to maintain blood pressure. This difference in response certainly supports the hypothesis that a cortisol concentration <15 μg/dl is evidence of relative adrenal insufficiency in this population, as it is in other patient populations.
Normal values for cortisol binding globulin (CBG) are somewhat lower for newborns than for adults (approximately 2 vs 3 mg/dl).24 However, since CBG in normal adult plasma can bind approximately 25 μg/dl of cortisol before saturation,25 a total cortisol concentration of 15 μg/dl in an infant should not exceed the usual binding capacity of CBG, and should result in a similar percentage of free cortisol in the term infant. Because of the variability in CBG concentrations, though, particularly in severely ill patients,26 measurement of free cortisol or CBG in addition to total cortisol concentration would add valuable information to future studies.
Our findings are consistent with one previous report that tested seven critically ill, hypotensive term newborns and found that six had cortisol values of <15 μg/dl and responded to dexamethasone with hemodynamic stabilization.21 Three additional small studies have described cortisol concentrations that seem inappropriately low in critically ill term newborns. Thomas et al. found that three of 11 ill infants had basal cortisol values <2 μg/dl, while Pittinger et al. reported that 79% of 34 cortisol levels measured in 10 infants with congenital diaphragmatic hernia were <7 μg/dl.27, 28 Soliman et al.29 recently reported 11 of 30 nonventilated, septic term newborns with basal cortisol values <15 μg/dl, four of whom had low responses to ACTH and a high mortality rate. To our knowledge, our study is the first to describe the prevalence of low cortisol concentrations as well as the response to hydrocortisone therapy in a cohort of term and near-term ventilated infants with vasopressor-resistant hypotension.
Postulated mechanisms underlying relative adrenal insufficiency in ill patients have included cytokine-related suppression of ACTH or cortisol synthesis, inadequate perfusion of the adrenal gland or a limited adrenocortical reserve.5, 9 Newborn infants may have additional factors predisposing them to relative adrenal insufficiency, unique to the newborn period, such as delayed maturation of the adrenal glands or a slow transition from intrauterine to extrauterine function.30 Infant adrenal glands are biochemically and morphologically different from adult adrenals; zonation of the adrenal gland is not complete and the pattern of secreted steroids differs.30
There are likely to be several mechanisms by which hydrocortisone therapy improves hemodynamic stability in critically ill patients. The downregulation of beta-adrenergic receptors found in critical illness can be reversed or prevented by glucocorticoids.20 In addition, as discussed thoroughly by Seri et al.,20 other mechanisms may include increased intracellular calcium availability, inhibition of catecholamine metabolism, decreased reuptake of catecholamines, inhibition of nitric oxide synthase expression and prostacyclin production, and improved capillary integrity.
In summary, this retrospective review found that a significant proportion of critically ill infants showed evidence of inadequate adrenal function, confirming the importance of evaluation of adrenal function and glucocorticoid therapy in the ill term and near-term newborn with refractory hypotension. Although the study captured a cohort of all infants admitted during a specific time period, interpretation of the results is limited by the heterogenous patient population included, the small numbers, the uncontrolled nature of the intervention and the lack of provocative testing. Prospective studies of the hypothalamic–pituitary axis and randomized trials of hydrocortisone replacement therapy in these infants would provide more information on the benefits and risks of treating relative adrenal insufficiency in this population.
References
Baldwin WA, Allo M . Occult hypoadrenalism in critically ill patients. Arch N Surg 1993;128:673–676.
Bone M, Diver M, Selby A, Sharples A, Addison M, Clayton P . Assessment of adrenal function in the initial phase of meningococcal disease. Pediatrics 2002;110:563–569.
Briegel J, Kellermann W, Forst H, et al. Low-dose hydrocortisone infusion attenuates the systemic inflammatory response syndrome. Clin Invest 1994;72:782–787.
Finlay WE, McKee JI . Serum cortisol levels in severely stressed patients. Lancet 1982;1:1414–1415.
Joosten KFM, De Kleijn ED, Westerterp M, et al. Endocrine and metabolic responses in children with meningococcal sepsis: striking differences between survivors and nonsurvivors. J Clin Endocrinol Metab 2000;85:3746–3753.
Rothwell PM, Udwadia ZF, Lawler PG . Cortisol response to corticotropin and survival in septic shock. Lancet 1991;337:582–583.
Sibbald WJ, Short A, Cohen MP, Wilson RF . Variations in adrenocortical responsiveness during severe bacterial infections: unrecognized adrenocortical insufficiency in severe bacterial infections. Ann Surg 2003;186:29–33.
Soni A, Pepper GM, Wyrwinski PM, et al. Adrenal insufficiency occurring during septic shock: incidence, outcome, and relationship to peripheral cytokine levels. Am J Med 1995;98:266–271.
Lamberts SWJ, Bruining HA, De Jong FH . Corticosteroid therapy in severe illness. N Engl J Med 1997;337:1285–1292.
McKee JI, Finlay WE . Cortisol replacement in severely stressed patients. Lancet 1983;1:484–485.
Cooper MS, Stewart PM . Corticosteroid insufficiency in acutely ill patients. N Engl J Med 2003;348:727–734.
Claussen MS, Landercasper J, Cogbill TH . Acute adrenal insufficiency presenting as shock after trauma and surgery: three cases and review of the literature. J Trauma 1992;32:94–100.
Kidess AI, Caplan RH, Reynertson RH, Wickus GG, Goodnough DE . Transient corticotropin deficiency in critical illness. Mayo Clin Proc 1993;68:435–441.
Annane D, Sébille V, Charpentier C, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 2002;288:862–871.
Ng PC, Lam CWK, Fok TF, et al. Refractory hypotension in preterm infants with adrenocortical insufficiency. Arch Dis Child Fetal Neonatal Ed 2001;84:F122–4.
Scott SM, Watterberg KL . Effect of gestational age, postnatal age, and illness on plasma cortisol concentrations in premature infants. Pediatr Res 1995;37:112–116.
Helbock HJ, Insoft RM, Conte FA . Glucocorticoid-responsive hypotension in extremely low birth weight newborns. Pediatrics 1993;92:715–717.
Fauser A, Pohlandt F, Bartmann P, Gortner L . Rapid increase of blood pressure in extremely low birth weight infants after a single dose of dexamethasone. Eur J Pediatr 1993;152:354–356.
Gaissmaier RE, Pohlandt F . Single-dose dexamethasone treatment of hypotension in preterm infants. J Pediatr 1999;134:701–705.
Seri I, Tan R, Evans J . Cardiovascular effects of hydrocortisone in preterm infants with pressor-resistant hypotension. Pediatrics 2001;107:1070–1074.
Tantivit P, Subramanian N, Garg M, Ramanathan R, deLemos RA . Low serum cortisol in term newborns with refractory hypotension. J Perinatol 1999;19:352–357.
Davidian M . Applied Longitudinal Data Analysis, Class Syllabus (ST-732). Raleigh, NC: North Carolina State University, Spring 2002. (www.stat.ncsu.edu/~st732_info/Davidian/#syllabus).
Gunn VL, Nechyba C . The Harriet Lane Handbook. Missouri: Harcourt; 2002. p. 712, 907.
Hanna CE, Jett PL, Laird MR, Mandel SH, LaFranchi SH, Reynolds JW . Corticosteroid binding globulin, total serum cortisol, and stress in extremely low-birth-weight infants. Am J Perinat 1997;14:201–204.
Williams GH, Dluhy RG . Disorders of the adrenal cortex. In: Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison's Principles of Internal Medicine. New York: McGraw-Hill; 2001. p. 2001–2084.
LE Roux CW, Chapman GA, Kong WM, Dhillo WS, Jones J, Alaghband-Zadeh J . Free cortisol index is better than serum total cortisol in determining hypothalamic–pituitary-adrenal status in patients undergoing surgery. J Clin Endocrinol Metab 2003;88:2045–2048.
Pittinger TP, Sawin RS . Adrenocortical insufficiency in infants with congenital diaphragmatic hernia: a pilot study. J Pediatr Surg 2000;35:223–226.
Thomas S, Murphy JF, Dyas J, Ryalls M, Hughes IA . Response to ACTH in the newborn. Arch Dis Child 1986;61:57–60.
Soliman AT, Taman KH, Rizk MM, Nasr IS, AIRimawy H, Hamido MSM . Circulating adrenocorticotropic hormone (ACTH) and cortisol concentrations in normal, appropriate-for-gestational-age newborns versus those with sepsis and respiratory distress: cortisol response to low-dose and standard-dose ACTH tests. Metabolism 2004;53:209–214.
Winter JSD . Fetal and Neonatal Adrenocortical Physiology. In: Polin RA, Fox WW, Abman SH, editors. Fetal and Neonatal Physiology. Philadelphia, PA: WB Saunders; 2004. p. 1915–1925.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fernandez, E., Schrader, R. & Watterberg, K. Prevalence of Low Cortisol Values in Term and Near-Term Infants with Vasopressor-Resistant Hypotension. J Perinatol 25, 114–118 (2005). https://doi.org/10.1038/sj.jp.7211211
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211211
This article is cited by
-
The use of supplemental hydrocortisone in the management of persistent pulmonary hypertension of the newborn
Journal of Perinatology (2021)
-
Adrenal insufficiency in neonates undergoing cardiopulmonary bypass and postoperative hypothalamic-pituitary-adrenal function after prophylactic glucocorticoids
Journal of Perinatology (2019)
-
An evaluation of hydrocortisone dosing for neonatal refractory hypotension
Journal of Perinatology (2017)
-
Steroid use for refractory hypotension in congenital diaphragmatic hernia
Pediatric Surgery International (2017)
-
Barriers to enrollment in a randomized controlled trial of hydrocortisone for cardiovascular insufficiency in term and late preterm newborn infants
Journal of Perinatology (2017)