Abstract
Traditional blood pressure (BP) methodology is subject to observer error such as terminal digit preference and single number preference leading to inaccuracies in measurement. A high percentage (60–90%) of terminal BP readings digit being zero has been reported from general medical- and hospital-based clinics. This study examined terminal digit preference in a hypertension specialty practice and assessed clinical factors that may be associated with zero preference in this setting. A retrospective chart review of patients presenting to the hypertension clinic at the University of Connecticut Health Center during the month of September 2001 was performed. Data were extracted on age, gender, height, weight, treatment status, and systolic and diastolic BP measurements taken by nursing staff and attending physicians. Terminal digit preference was apparent in BP readings taken by both nursing staff and physicians. Zero was the terminal systolic BP digit in 40% of readings taken by the nursing staff and 31% of readings taken by physicians. For diastolic BP readings, the percentages were 23 and 36%, respectively. Nurses also recorded 43% of diastolic BP readings with terminal digit 2. Age was significantly higher in those persons in whom the physician diastolic BP terminal digit was zero than in those with nonzero terminal digits (67±14 vs 59±18 years, P=0.008). Body mass index was lower in the patient group with diastolic terminal digit zero bias compared to those with nonzero terminal digits (28±5 vs 32±6 kg/m2, P=0.02). In conclusion, although the frequency of zero digit preference did not reach the 60–80% levels found in previous studies, there was evidence of terminal digit preference in the systolic and diastolic measurements taken by nursing staff and attending physicians in a specialist hypertension clinic. We believe that the lower levels of terminal digit preference observed are an effect of increased training in proper BP measurement and technique. However, the observed bias in measurement even in a hypertension unit argues for regular monitoring and feedback to minimize such errors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Feher M, Harris-St John K, Lant A . Blood pressure measurement by junior hospital doctors, a gap in medical education? Health Trends 1992; 24: 59–61.
Kemp F, Foster C, Mc Kinlay S . How effective is training for blood pressure measurement? Prof Nurse 1994; 8: 521–522.
Gillespie A, Curzio J . Blood pressure measurement: assessing staff knowledge. Nurs Standard 1998; 12: 35–37.
Johnston GD . Digit preference lays conclusions about orlistat open to doubt. BMJ 2001; 322: 110.
Keary L, Atkins N, O'Brien ET . Terminal digit preference and heaping in office blood pressure measurements [abstract]. J Hum Hypertens 1998; 12: 787–788.
Stoneking HT, Hla KM, Samsa GP, Feussner JR . Blood pressure measurements in the nursing home: are they accurate? Gerontologist 1992; 32: 536–540.
Wingfield D et al., on behalf of the Syst-Eur Investigators. Terminal digit preference and single-number preference in the Syst-Eur trial: influence of quality control. Blood Press Monit 2002; 7: 169–177.
Patterson HR . Sources of error in recording the blood pressure of patients with hypertension in general practice. BMJ 1984; 289: 1661–1664.
Wen SW et al. Terminal digit preference, random error, and bias in routine clinical measurement of blood pressure. J Clin Epidemiol 1993; 46: 1187–1193.
Ali S, Rouse A . Practice Audits: reliability of sphygmomanometers and blood pressure recording bias. J Hum Hypertens 2002; 16: 359–361.
Hessel PA . Terminal digit preference in blood pressure measurements: effects on epidemiological associations. Int J Epidemiol 1986; 15: 122–125.
Perloff D et al. Special report: human blood pressure determination by sphygmomanometry. Circulation 1993; 88: 2460–2470.
Kay LE . Accuracy of blood pressure measurement in the family practice center. J Am Board Fam Pract 1998; 11: 252–258.
Wingfield D, Freeman GK, Bulpitt CJ . Selective recording in blood pressure may increase subsequent mortality. Q J Med 2002; 95: 571–577.
Parati G et al, and the participants in the 2001 Consensus Conference on Ambulatory Blood Pressure Monitoring. Blood pressure measurement in research. Blood Press Monit 2002; 7: 83–87.
Fagard RH, Staessen JA . Characteristics of conventional blood pressure in studies on the predictive power of ambulatory blood pressure. Blood Press Monit 2002; 7: 33–36.
Staessen JA, O'Brien ET, Lutgarde T, Fagard RH . Modern approaches to blood pressure measurement. Occup Environ Med 2000; 57: 510–520.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thavarajah, S., White, W. & Mansoor, G. Terminal digit bias in a specialty hypertension faculty practice. J Hum Hypertens 17, 819–822 (2003). https://doi.org/10.1038/sj.jhh.1001625
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001625
Keywords
This article is cited by
-
Screening for hypertension in adults: protocol for evidence reviews to inform a Canadian Task Force on Preventive Health Care guideline update
Systematic Reviews (2024)
-
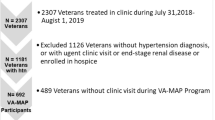
Protocol to improve hypertension management in a VA outpatient clinic
Journal of Human Hypertension (2023)
-
Concept, hardware development, and clinical trials of a Galinstan based Mercury free sphygmomanometer: Merkfree
Scientific Reports (2022)
-
A retrospective evaluation of the risk of bias in perioperative temperature metrics
Journal of Clinical Monitoring and Computing (2019)
-
Do physicians measure patients’ blood pressure, and are those measurements reliable?
Journal of Human Hypertension (2018)