Abstract
Purpose
To analyse the spectrum of angiographic features in patients monolaterally or bilaterally affected by pseudoexfoliation syndrome (PES), with and without glaucoma, and to evaluate the sensibility and specificity of these features in the diagnosis of glaucoma.
Methods
Sixty-eight patients affected by PES and 20 healthy subjects underwent iris fluorescein angiography (IFA) and iris indocyanine green angiography (IICGA). Angiographic features analysed were hypoperfusion, microneovascularizations, and anastomotic vessels.
Results
There was no statistically significant difference among unaffected, unilaterally affected, and bilaterally affected eyes. Patients affected by PES glaucoma showed a statistically significant difference with respect to the other groups for most of the variables. The results of qualitative variables revealed a gradual increase of the vascular involvement in the different groups. Peripupillary tufts, stromal tufts, and radial arterioles showed the best sensibility and specificity values on IFA, whereas radial arterioles and plexuses showed the highest sensibility and specificity values on IICGA. Considering all the parameters, the results were not associated with large effects on the post-test probability of disease. The values of likelihood ratio indicated that none of the examined variables was sufficiently able to discriminate patients affected by PSE glaucoma from the overall group.
Conclusions
Patients clinically affected only monolaterally by PES show microvascular changes, which are similar in both eyes. Glaucoma PES represents a more advanced stage of the disease, with more pronounced alterations, even though no typical microvascular pattern can be identified by iris angiography.
Similar content being viewed by others
Introduction
Pseudoexfoliation syndrome (PES) is an age-related fibrillopathy with systemic involvement, characterized by synthesis and deposition of an abnormal extracellular fibrillar material. Iris involvement is histologically expressed by iris vasculopathy, with degeneration of smooth muscle cells, pericytes, and endothelial cells, pseudoexfoliation material deposits at the periphery of iris vessels, with thickening and reduplication of basement membranes.1, 2 The reported histological changes are the morphological correlate of the blood–aqueous barrier (BAB) breakdown, which can be studied by means of several techniques, including fluorophotometry,3 laser flare-cell meter,4, 5, 6 immunohistochemical tracer,7 and iris angiography.3, 8, 9, 10, 11
Typical features of PES on iris angiography are hypoperfusion, microneovascularizations, and anastomotic vessels.3, 9, 10, 11 Comparison between iris fluorescein angiography (IFA) and iris indocyanine green angiography (IICGA) has shown that IICGA is superior in disclosing iris hypoperfusion and anastomotic vessels, whereas IFA allows a more precise detection of microneovascularizations.10, 11 Nevertheless, no study has tried to correlate the iris vascular changes with the different clinical manifestations of PES. The aims of the present study are to compare the spectrum of quantitative and qualitative angiographic features in patients monolaterally or bilaterally affected by PES and to evaluate the sensibility and specificity of these features in the diagnosis of PES glaucoma.
Materials and methods
The study enrolled patients who were affected by PES and were examined in the outpatient department of Trieste Eye Clinic between January 2002 and February 2004. The research adhered to the tenets of the Helsinki Declaration and was approved by the Institutional Review Board. Each patient was carefully informed about the purpose of the research, providing signed consent to all procedures. The inclusion criterion was the presence of previously undiagnosed PES. Exclusion criteria were presence of any other eye disease able to affect the iris vascular pattern, ocular hypothensive therapy, or previous laser or surgical treatment.
The diagnosis of PES was based upon the biomicroscopic evidence of flakes of pseudoexfoliation material on the anterior lens capsule and/or the pupillary margin of the iris. PES glaucoma was diagnosed in PES patients with glaucomatous optic neuropathy (cupping, rim notching, or diffuse thinning on fundus stereobiomicroscopy performed under pupil dilation with the aid of a +78 D lens). Standard automated perimetry was performed with the Humphrey Field Analyser (HFA, Carl Zeiss, Dublin, CA, USA; 24-2 program SITA standard strategy) and defects were classified as glaucomatous with either glaucoma hemifield test outside normal limits or pattern standard deviation with probability <5%. Defects had to be reproducible, that is, confirmed in at least two consecutive tests. All patients underwent a complete ophthalmological examination, including IFA and IICGA, before the administration of any therapy.
Healthy volunteers, without any ocular and systemic diseases, who were examined in the outpatient department of the Eye Clinic for reading-glass prescriptions were considered as control group.
IFA and IICGA were carried out using IMAGEnet System H1024 (Topcon Corp., Japan).
Angiographic alterations were assessed on the basis of hypoperfusion, microneovascularizations, and anastomotic vessels.9 In particular, hypoperfusion was revealed by reduction of the number of radial arterioles, sectorial filling defects, and attenuation of radial arterioles. Microneovascularization was classified as pupillary tufts, peripupillary tufts, stromal tufts, and plexuses. Anastomotic vessels were subdivided into peripheral loops, obliquely or circumferentially running vessels, or pronounced lesser circle of the iris. The number of each single feature was calculated in each iris, even for eyes without slit-lamp evidence of PES (ie eyes not clinically affected in monolateral PES). Angiograms were independently read by two separate investigators (TL, PI), who were unaware of the purpose of the study and the condition of the patients. The uncertain cases were evaluated by a third author (GR). A measurement of intergrader agreement (κ-value) was calculated for the graders.
The main variables evaluated in this study included radial arterioles, sectorial filling defects, attenuated arterioles, pupillary tufts, peripupillary tufts, stromal tufts, plexuses, peripheral loops, oblique vessels, and lesser circle. Quantitative variables were expressed as mean±SD for the five groups (control, unaffected, monolaterally affected, bilaterally affected, and glaucoma) measured with IFA and ICGA. All variables were expressed as frequencies and percentages. The Kruskal–Wallis test provided a statistical analysis of differences between the five groups for each quantitative variable. A nonparametric multiple comparison test for Kruskal—Wallis was then used to examine the differences between all possible pairs of groups. χ2 with Bonferroni multiple comparison correction was used to evaluate the statistical significance of the difference between frequencies for all variables in each pair of groups. Moreover, sensibility, specificity, and likelihood ratio (LR) (CI 95%) were calculated in order to identify the variables with the best discriminating performance between PES eyes with and without glaucoma. An LR was defined as the probability of a given test result in those with disease divided by the probability of the same test result in those without the disease. Once determined, an LR could be incorporated directly into the calculation of the post-test probability of disease by using a formulation of the Bayes theorem. The LR for a given test result indicated how much that result will raise or lower the probability of disease. A value of 1 means that the test provided no additional information, and a ratio higher or lower than 1 increases or decreases the likelihood of disease, respectively. The Mann–Whitney test was performed to compare microneovascularization and hypoperfusion features on IFA and IICGA in glaucoma and non-glaucoma groups. Statistical analysis was performed using SPSS® Advanced Statistical™ 10.0 Software (SPSS Sciences, Chicago, IL, USA).
Results
Sixty-eight patients (136 eyes) fulfilled the inclusion and exclusion criteria. There were 38 (56%) female and 30 (44%) male patients. All patients were Caucasian, with a mean age of 64.9±7.5 SD (range: 53–79). Nineteen patients presented monolateral and 31 bilateral PES, whereas 18 patients were bilaterally affected by PES glaucoma.
Twenty healthy subjects (40 eyes) agreed to take part in the study as a control group. Their mean age was 62.5±7.8 SD (range: 53–80). Complete demographics are listed in Table 1. The κ score between the two graders who read the angiograms was 0.86.
The results of quantitative variables are summarized in Table 2. IICGA turned out to be better than IFA for disclosing features of hypoperfusion and anastomotic vessels, as opposed to microneovascularizations. All variables showed no statistically significant difference among unaffected, unilaterally affected, and bilaterally affected (U-UA-BA) groups. Moreover, most variables in patients affected by PES glaucoma were statistically different compared to the other groups (P<0.001). In particular, both on IFA and on ICGA, eyes with PES glaucoma showed statistically significant values, with regard to radial arterioles, in both control and U-UA-BA groups. On the other hand, sectorial filling defects and attenuated arteriole values were statistically different compared with the control group only. As for microneovascularization, the pupillary tuft values were significantly greater only with respect to the control group, whereas all the other variables were statistically different with regard to the control and U-UA-BA groups.
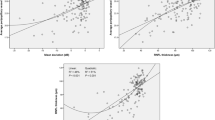
The results of qualitative variables are shown in Figures 1 (anastomotic vessels), 2 (hypoperfusion), 3 (microneovascularization). The data revealed a gradual increase in the vascular involvement in different groups. In particular, the unaffected group showed no difference with respect to the control group, especially with respect to hypoperfusion and anastomotic vessels.
The values of the sensibility and specificity, as well as the values of LR of the radial arterioles, peripheral loops, peripupillary tufts, stromal tufts, and plexuses in 136 eyes (36=glaucoma; 100=no glaucoma) are listed in Table 3. Taking IFA into account, peripupillary tufts, stromal tufts, and radial arterioles were the variables showing the best sensibility and specificity values. On the other hand, radial arterioles and plexuses showed the highest sensibility and specificity values on IICGA.
For all parameters, the results were not associated with large effects on the post-test probability of disease. The values of LR indicated that none of the examined variables was sufficiently able to discriminate patients affected by PSE glaucoma from the overall group.
Table 4 shows a comparison among the features analysed with two methodologies in glaucoma and non-glaucoma groups. Radial arterioles (P<0.001), peripupillary tufts (P<0.01), stromal tufts (P<0.001), and plexuses (P<0.001) all turned out to be statistically different in IFA. Radial arterioles (P<0.001), sectorial filling defects (P<0.01), pupillary tufts (P<0.05), peripupillary tufts (P<0.001), plexuses (P<0.001), peripheral loops (P<0.01), and lesser circle (P<0.05) were statistically different on IICGA.
Discussion
PES is a frequent systemic disorder characterized by an accumulation of fibrillary material within several tissues. Besides the eye, PES may involve skin, heart, abdominal aorta, lung, liver, kidney, cerebral meninges, and gall bladder.2 At the ocular level, PES is to be considered a bilateral disorder with asymmetric eye involvement, even when the clinical examination reveals the presence of typical alterations only in a single eye. Indeed, ultrastructural studies have demonstrated that histological alterations are also present in anterior segment tissues of fellow eyes ostensibly not involved, including typical PES fibril deposits on iris and ciliary epithelia and in the dilator muscle, increased accumulation of extracellular matrix, and degenerative changes of iris pigment epithelium and dilator muscle cells.12, 13
Considering the fact that PES can predispose to several conditions requiring medical or surgical treatment, it is important to define precisely the stage of the disorder. Iris angiography can easily highlight the microvascular abnormalities typical of PES, and may prove useful in assessing the degree of vascular impairment in a non-invasive way.
Several authors have identified hypoperfusion, microneovascularizations, and anastomotic vessels as being common features on IFA.3, 9, 10, 11 IFA has been proved to be superior in detecting microneovascularizations, whereas IICGA is more precise in disclosing iris hypoperfusion and anastomotic vessels.10, 11 In the current investigation, we have tried to assess if there is a gradual progression of the severity of microvascular abnormalities in the different stages of the disease. The results of quantitative analyses show that unaffected, affected, and bilateral groups are quite similar, whereas eyes affected by PES glaucoma have more severe involvement. A gradual progression of the vascular impairment is shown by the evaluation of the qualitative analyses in the different subgroups. These findings indicate that clinically unaffected eyes share the same microvascular alterations typical of eyes in which PES is clinically evident, even though some features, such as hypoperfusion and microneovascularizations, are expressed to a lesser extent. On the other hand, eyes affected by PES glaucoma reveal a more severe angiographic involvement, which can be interpreted as indicative of a more advanced stage of the disease.
The second aim of the study was to assess the sensibility and specificity of features such as hypoperfusion, anastomotic vessels, and microneovascularizations in the diagnosis of PES glaucoma. Plexuses examined by means of IFA showed the highest values of sensitivity (0.80) and specificity (0.83). Nevertheless, the corresponding LR showed a moderate effect on the post-test probability of disease. Overall, no angiographic variable showed an LR with a sufficiently large effect to define the diagnosis of PES glaucoma. This is not surprizing bearing in mind the random distribution of vascular changes typical of PES. Therefore, even though our results indicate that eyes affected by PES glaucoma show greater microvascular alterations, there is no typical microvascular pattern detectable by iris angiography, which can be associated with PES glaucoma.
In conclusion, iris angiographic examination demonstrates that patients clinically affected only monolaterally by PES show microvascular changes, which are similar in both eyes. Glaucoma PES represents a more advanced stage of the disease with more pronounced alterations, even though no typical microvascular pattern can be identified by iris angiography.
References
Asano N, Schlotzer-Schrehardt U, Naumann GO . A histopathologic study of iris changes in pseudoexfoliation syndrome. Ophthalmology 1995; 102: 1279–1290.
Naumann GO, Schlotzer-Schrehardt U, Kuchle M . Pseudoexfoliation syndrome for the comprehensive ophthalmologist. Intraocular and systemic manifestations. Ophthalmology 1998; 105: 951–968.
Brooks AM, Gillies WE . Fluorescein angiography and fluorophotometry of the iris in pseudoexfoliation of the lens capsule. Br J Ophthalmol 1983; 67: 249–254.
Kuchle M, Nguyen NX, Horn F, Naumann GO . Quantitative assessment of aqueous flare and aqueous ‘cells’ in pseudoexfoliation syndrome. Acta Ophthalmol (Copenh) 1992; 70: 201–208.
Kuchle M, Nguyen NX, Hannappel E, Beck W, Ho ST, Naumann GO . Tyndallometry with the laser flare cell meter and biochemical protein determination in the aqueous humor of eyes with pseudoexfoliation syndrome. Ophthalmologe 1994; 91: 578–584.
Kuchle M, Nguyen NX, Hannappel E, Naumann GO . The blood–aqueous barrier in eyes with pseudoexfoliation syndrome. Ophthalmic Res 1995; 27 (Suppl 1): 136–142.
Nguyen NX, Martus P, Kuchle M . A clinical comparative study of tyndallometry using 2 laser flare meters. Klin Monatsbl Augenheilkd 1996; 209: 89–93.
Vannas A . Fluorescein angiography of the vessels of the iris in pseudoexfoliation of the lens capsule, capsular glaucoma and some other forms of glaucoma. Acta Ophthalmol Suppl 1969; 105: 1–75.
Brooks AM, Gillies WE . The development of microneovascular changes in the iris in pseudoexfoliation of the lens capsule. Ophthalmology 1987; 94: 1090–1097.
Parodi MB, Bondel E, Saviano S, Ravalico G . Iris fluorescein angiography and iris indocyanine green videoangiography in pseudoexfoliation syndrome. Eur J Ophthalmol 1999; 9: 284–290.
Parodi MB, Bondel E, Saviano S, Ravalico G . Iris indocyanine green angiography in pseudoexfoliation syndrome and capsular glaucoma. Acta Ophthalmol Scand 2000; 78: 437–442.
Hammer T, Schlotzer-Schrehardt U, Naumann GO . Unilateral or asymmetric pseudoexfoliation syndrome? An ultrastructural study. Arch Ophthalmol 2001; 119: 1023–1031.
Kivela T, Hietanen J, Uusitalo M . Autopsy analysis of clinically unilateral exfoliation syndrome. Invest Ophthalmol Vis Sci 1997; 38: 2008–2015.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parodi, M., Liberali, T., Iacono, P. et al. The spectrum of iris angiography abnormalities in pseudoexfoliation syndrome. Eye 22, 49–54 (2008). https://doi.org/10.1038/sj.eye.6702602
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702602
Keywords
This article is cited by
-
Quantitative analysis of radial peripapillary capillary plexuses in patients with clinically unilateral pseudoexfoliation syndrome
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)
-
Anterior chamber aqueous flare, pseudoexfoliation syndrome, and glaucoma
International Ophthalmology (2016)