Abstract
Objective
To investigate the intraocular penetration of moxifloxacin into the aqueous and vitreous after oral administration in humans.
Methods
A prospective, nonrandomized study of 27 consecutive patients scheduled for elective parsplana vitrectomy surgery between 1 October and 31 December 2004 was carried out. Aqueous, vitreous, and serum samples were obtained and analysed after oral administration of a single 400 mg tablet of moxifloxacin a few hours before surgery. Assays were performed using high-performance liquid chromatography.
Results
Mean±SD moxifloxacin concentrations in the serum (n=27), aqueous (n=25), and vitreous (n=27) were 1.34±0.98, 0.21±0.21, and 0.09±0.09 μg/ml, respectively. The mean±SD sampling times after oral administration of the moxifloxacin tablet for serum, aqueous, and vitreous were 2.02±0.51, 1.53±0.45, and 1.55±0.46 h, respectively. The minimum inhibitory concentration for 90% of isolates (MIC90) was far exceeded in the aqueous for a wide spectrum of key pathogens, whereas it was not exceeded in the vitreous for several organisms. Of note, the MIC90 for Staphylococcus epidermidis was not exceeded in any of the samples.
Conclusions
Orally administered moxifloxacin achieves measurable levels in the noninflammed human eye, with the aqueous levels effective against a variety of pathogens. However, the spectrum of coverage does not appropriately encompass the most common causative organisms in endophthalmitis, especially Staphylococcus epidermidis. Further studies are needed to precisely define the role of oral moxifloxacin in the treatment of or prophylaxis against intraocular infections.
Similar content being viewed by others
Introduction
Bacterial endophthalmitis is one of the most serious complications after intraocular surgery. The Endophthalmitis Vitrectomy Study (EVS) investigated the microbiologic spectrum of infecting organisms in the largest number of postoperative endophthalmitis cases so far, in a prospective manner.1 It revealed that 94.2% of isolates from postoperative endophthalmitis are Gram-positive pathogens, most commonly Staphylococcus epidermidis and Staphylococcus aureus. Gram-negative pathogens, the most common being Proteus mirabilis, accounted for only 5.9% of confirmed-growth isolates.1 The EVS also investigated the use of intravenous amikacin and ceftazidime along with intravitreal antibiotics for postoperative endophthalmitis and found no benefit.2 These two drugs were shown to have very poor intravitreal penetration by later studies.3, 4 In the post-EVS era, it has been shown that fluoroquinolones can achieve effective intravitreal levels after oral administration even in noninflammed eyes.5, 6, 7, 8, 9, 10
Of these, the newly released fourth-generation fluoroquinolones (moxifloxacin and gatifloxacin, grepafloxacin, and trovafloxacin) have a spectrum of activity encompassing Gram-positive and Gram-negative bacteria, including Staphylococcus epidermidis, Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes, Haemophilus influenzae, Escherichia coli, Bacillus cereus, Neisseria gonorrhoeae, and P. mirabilis. In addition, they demonstrate good activity against atypical pathogens such as Mycoplasma, Legionella, and Chlamydia species, as well as the anaerobic organism Propionibacterium acnes.11, 12 They have a greater binding affinity to the bacterial DNA–DNA gyrase complex, with the resultant greater potency in inhibiting bacterial DNA synthesis.13 The more favourable pharmacokinetic profile might be due to alterations of the original fluoroquinolone moiety (for example, moxifloxacin and gatifloxacin possess an 8-methoxy side chain). Among these, moxifloxacin, a novel fourth generation fluoroquinolone, has a spectrum of coverage against the pathogens most commonly responsible for postoperative, post-traumatic, and bleb-associated endophthalmitis with minimum inhibitory concentration (MIC) levels for Gram-positive bacteria, which are generally lower than those of the other fluoroquinolone antibiotics, including gatifloxacin.14, 15
Moxifloxacin has 90% oral bioavailability, can be administered regardless of food, and reaches peak plasma concentrations 1–2 h after oral dosage, with an approximate half-life of 10 h.16 It is widely distributed into many tissues and body fluids, with a serum protein binding of 50%. There have been no known life threatening reactions.16 Moreover, two studies have documented effective penetration of oral8 and topical10 moxifloxacin into the aqueous humor alone and both aqueous and vitreous respectively. However, there are no studies documenting the penetration of orally administered moxifloxacin into the vitreous in humans. We hence chose to determine the penetration pharmacokinetics of orally administered moxifloxacin into the human aqueous and vitreous.
Methods
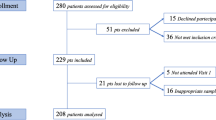
We performed this study with the approval of our Ethics committee and the Institutional Review Board. In total, 27 consecutive adult patients, aged 20–76 years (mean±SD age, 46.74±15.63 years), undergoing elective pars plana vitrectomy between 1 October and 31 December 2004, at the Aravind Eye hospital and Postgraduate Institute of Ophthalmology, Madurai, were included in the study. Exclusion criteria included known sensitivity to fluoroquinolones, such as renal disease (creatinine level >1.8 mg/dl (>159.1 μmol/l)), use of any other antibiotic(s) in the preceding 3 weeks, pregnancy or current breast-feeding, current use of a class IA or class III antiarrhythmic agent. We also excluded previously vitrectomized eyes, and eyes with fresh vitreous haemorrhage as indication for vitrectomy (<1 month), or active endophthalmitis. It was also ensured that the patients were not receiving antacids, calcium, and iron supplements at that time, which are known to affect the absorption of moxifloxacin.
After informed consent was obtained, patients were administered by the ward nurse, a single tablet of 400 mg of moxifloxacin (Torrent Pharmaceuticals Ltd, Ankleshwar, India) 1–2 h before surgery. All the moxifloxacin tablets belonged to the same batch and were purchased in bulk. The ward nurse also noted the exact time of administration of the tablet. Prospectively, completed data forms were designed to include age, medical history, lens status, the indication for vitrectomy, time of moxifloxacin administration and time of sample (serum, aqueous and vitreous) collection, and concentrations of moxifloxacin in the serum, aqueous, and vitreous. Patients were asked to return the empty tablet cover of moxifloxacin to ensure compliance.
Aqueous and vitreous samples were obtained before infusion of any intraocular irrigating solution to obtain undiluted, pure samples. In the operative suite, approximately 0.1 ml of aqueous fluid was aspirated through a paracentesis site using a 30-gauge needle attached to a syringe. Within 10 min, 0.2–0.3 ml of vitreous fluid was obtained using a vitreous cutter attached to a syringe via a short length of tubing. Approximately, 8–10 ml of venous blood was also collected and serum was isolated using standard technique.
The samples were immediately frozen at −83°C. These samples along with a sample of moxifloxacin tablets from the batch that was administered to the patients were shipped with dry ice in appropriate packaging material to the All India Institute of Medical Sciences, New Delhi, India. Moxifloxacin concentrations were determined in each of the samples using a previously described high-performance liquid chromatography technique (HPLC) used for estimation of intraocular ciprofloxacin with slight modifications.17 Briefly, Thermo Surveyor HPLC (Thermo Electron Corporation, USA) connected with an autosampler, online degasser and photodiode array detector (model 996;Waters) was used. Acetonitrile and phosphate buffer (20 mM) with pH 2.5 (adjusted with phosphoric acid) was used at the ratio of 25 : 75 pumped at the rate of 1 ml/min. The peak was monitored at 295 nm and the analytical separation was achieved by using Symmetry Shield C18 column (Waters, USA). External calibration curve was made by spiking known concentration of moxifloxacin in drug-free plasma and vitreous humor (obtained from donor eyes from eye bank). For the aqueous humor, drug spiked phosphate-buffered saline pH 7.2 was used to make the external calibration curve. Under the given conditions, moxifloxacin was eluted at the retention time of 3.1 min and the limit of quantification and limit of detection were found to be 0.015 and 0.002 μg/ml, respectively. The calibration curve for moxifloxacin between the concentrations from 0.015–10 μg/ml was found to be linear (r2=0.999). The peak purity and ultraviolet spectral match was achieved using the photograph-diode array (PDA) option using the software Chromquest Ver. 4.0. Serum, aqueous and vitreous samples were deproteinated with acetonitrile in the ratio of 1 : 2 and vortexed for 2 min and centrifuged at 8000 g for 15 min. The supernatant was injected in the volume of 20 μl into the HPLC column for analysis. All the samples were processed at the same time, and in between every 10 samples a known standard was used to confirm the lack of variation in the analytical parameters.
Mean±SD of the drug concentrations in the serum, aqueous, and vitreous were computed. Aqueous and vitreous moxifloxacin concentrations were compared with already established in vitro MIC90 data (Table 1).15 Mann–Whitney U-test was performed to determine if any significant differences existed between various subsets of patients, with regard to the phakic status.
Results
The mean±SD sampling times after oral administration of the moxifloxacin tablet for serum, aqueous, and vitreous were 2.02±0.51, 1.53±0.45, and 1.55±0.46 h, respectively. No serious adverse reactions attributable to the antibiotic were noted.
Indications for vitrectomy in the 27 patients were as follows (Table 2): retinal detachment (n=11), long standing vitreous haemorrhage (n=12), ectopia lentis (n=3), and macular hole (n=1).
Aqueous data from patients 15 and 16 were removed from the study, as laboratory analysis showed insufficient sample volume to perform HPLC. Mean±SD moxifloxacin concentrations in the serum (n=27), aqueous (n=25), and vitreous (n=27) were 1.34±0.98, 0.21±0.21, and 0.09±0.09 μg/ml, respectively. The percentages of serum moxifloxacin concentration achieved in the aqueous and vitreous were 15.59 and 6.77%, respectively. The sample of moxifloxacin tablet from the batch that was administered to the patients was also found to contain 108% of the label claim.
Among the serum, aqueous, and vitreous concentrations, there appeared to be several values that were considered outliers. For example, patient 16 had serum levels approximately 67-fold, and patients 4 and 15 had vitreous levels 45 times below the mean values of the rest of the group, respectively (Table 2). We chose to include all data obtained in the study, as the investigators could not explain these high or low concentrations and attributed them to variability of moxifloxacin pharmacokinetics in individual patients.
A subgroup analysis of the aqueous and vitreous values was carried out based on the lens status to see if prior intraocular surgery leads to alteration of the drug pharmacokinetics, since it is conceivable that intravitreal levels of a drug might be higher in an eye that has undergone surgery. In total, 16 patients had phakic eyes, while 11 patients were pseudophakic. Of the 16 phakic eyes, three patients had ectopia lentis and had a subluxed lens that was still visible in the pupillary axis, with no vitreous in the anterior chamber. They underwent a parsplana lensectomy and vitrectomy. In the phakic and pseudophakic patients the drug concentrations in the aqueous were 0.17±0.16 and 0.27±0.26 μg/ml, respectively, while the drug concentrations in the vitreous were 0.07±0.11 and 0.11±0.08 μg/ml respectively. There was no statistically significant difference in these values by Mann–Whitney U-test (P-value of 0.16 and 0.09 for the aqueous and vitreous samples, respectively).
Comment
The main reason we chose to study the intraocular penetration of orally administered moxifloxacin is that the MIC90 of moxifloxacin was generally lower than those for the other fluoroquinolone antibiotics against the pathogens most commonly responsible for postoperative, post-traumatic, and bleb-associated endophthalmitis (Table 1).15 These include Staphylococcus epidermidis (which accounted for 70% of the Endophthalmitis Vitrectomy Study isolates),1 Streptococcal or Staphylococcal species or by Gram-negative organisms (especially P. mirabilis), P. acnes, etc.
The mean±SD levels of moxifloxacin in the aqueous and vitreous in our study were significantly lower than that reported by Hariprasad et al9 for gatifloxacin (mean±SD levels of 1.34±0.34 and 1.08±0.54 μg/ml in the human vitreous and aqueous, respectively). However, they had used a loading dose of 400 mg gatifloxacin tablet twice a day before sample collection in order to achieve peak plasma concentrations more rapidly, despite the fact that the recommended dose of gatifloxacin is 400 mg once daily. The recommended dose of moxifloxacin too is 400 mg once daily. In our study, we administered only a single oral dose of 400 mg of moxifloxacin in order to more closely simulate the clinical scenario and to more precisely determine the intraocular penetration. Of course, this could have accounted for the lower intraocular levels seen in our study.
In another study, by Hariprasad et al,10 six-hourly administration of topical 0.5% moxifloxacin resulted in aqueous and vitreous levels that were lesser (0.88±0.88 and 0.06±0.06 μg/ml, respectively) than the levels achieved in our study. However, intensive two-hourly topical application was found to achieve reasonably good aqueous levels (2.28±1.23 μg/ml) although the vitreous levels (0.11±0.05μg/ml) were not satisfactory. Both the values were, however, higher than that found by us in our study. It is possible that penetration/equilibration of orally administered moxifloxacin with ocular fluids takes longer to achieve higher levels when compared to intensive topical administration, which has been shown to achieve excellent intraocular levels previously.18 However, the low aqueous levels of moxifloxacin in our study were similar to another study by Hariprasad et al19 using presoaked collagen shield devices for delivery of moxifloxacin.
Our values are also lower than those published by Garcia-Saenz and co-workers,8 who investigated the penetration of orally administered moxifloxacin into the human aqueous humor. They found that moxifloxacin achieved a mean±SD aqueous concentration of 2.33±0.85 μg/ml. The authors did not study the intravitreal penetration of moxifloxacin. Although they too administered only a single tablet of 400 mg of moxifloxacin, they employed two-dimensional diffusion microbiological assay to estimate the antibiotic concentrations, and not HPLC as used by us. But whether the difference in methodology could account for the difference is debatable since the sensitivities and reproducibility of results of these two methods have been comparable.20 Garcia-Saenz et al16 also administered the tablet 10 h prior to sampling. We administered the tablets roughly 2 h prior to sampling since it has been shown that the mean steady state C(max) of 3.2–4.5 mg/l was reached in 1.5 h after oral administration of a single 400 mg tablet. In order to precisely determine whether this fact accounts for the difference in intraocular levels, we would have to increase the time interval between tablet intake and sample collection from 2 h to further 4, 6, 8, and 10 h postdosage. Our present study evaluated only the possibility of using moxifloxacin approximately 2 h before surgery and its relevant concentrations in the aqueous, vitreous, and plasma samples. We are in the process of initiating another study with intraocular samples being taken at different time frames after administration of moxifloxacin tablet.
Despite the low intraocular levels achieved in our study, the aqueous concentrations exceeded the MIC90 of several organisms (Table 1).15 These included Gram-positive bacteria such as Staphylococcus aureus (MSSA), Streptococcus pneumoniae, and Streptococcus pyogenes, Gram-negative bacteria such as H. influenzae, Klebsiella pneumoniae, Moraxella catarrhalis, N. gonorrhoeae, P. mirabilis, and Enterobacter species, anaerobic bacteria such as Clostridium perfringens, and P. acnes. As found previously,10 the vitreous levels achieved were lower than the aqueous levels in our study, confirming that the blood-aqueous barrier is more permeable than the blood–retinal barrier. However, the vitreous levels were sufficient to exceed the MIC90 of a few organisms such as H. influenzae, M. catarrhalis, N. gonorrhoeae, P. mirabilis, Legionella pneumophila, and Enterobacter species.
Of note, in our study, moxifloxacin was unable to achieve even aqueous levels that would be effective against Staphylococcus epidermidis, Pseudomonas aeuroginosa, and Staphylococcus aureus (MRSA) species; the former being the most common cause of postoperative endophthalmitis.1 Intravitreal levels that would be effective against Staphylococcus epidermidis, Staphylococcus aureus (MRSA), and P. acnes were also not achieved in our study. But before concluding that oral moxifloxacin might not be a suitable initial treatment choice in endophthalmitis, studies evaluating the intraocular levels after different time intervals following administration as well as the cumulative levels achieved after 2 or more days of dosage need to be carried out.
In summary, orally administered moxifloxacin achieves therapeutic levels in the noninflammed human eye, especially with the levels achieved in the aqueous effective against a variety of pathogens. However, the spectrum of coverage does not appropriately encompass the most common causative organisms in endophthalmitis, especially Staphylococcus epidermidis. The pharmacokinetic findings of this investigation also show that orally administered 400 mg of moxifloxacin can achieve relatively higher aqueous when compared to vitreous concentrations. The concentrations achieved are independent of the phakic status of the eye. Future studies will be needed to precisely define the role of orally administered moxifloxacin in the treatment of or prophylaxis against intraocular infections.
References
Han DP, Wisniewski SR, Wilson LA, Barza M, Vine AK, Doft BH et al. Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol 1996; 122: 1–17.
Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study: a randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol 1995; 113: 1479–1496.
el-Massry A, Meredith TA, Aguilar HE, Shaarawy A, Kincaid M, Dick J et al. Aminoglycoside levels in the rabbit vitreous cavity after intravenous administration. Am J Ophthalmol 1996; 122: 684–689.
Aguilar HE, Meredith TA, Shaarawy A, Kincaid M, Dick J . Vitreous cavity penetration of ceftazidime after intravenous administration. Retina 1995; 15: 154–159.
Cekic O, Batman C, Yasar U, Basci NE, Bozkurt A, Kayaalp SO et al. Human aqueous and vitreous humour levels of ciprofloxacin following oral and topical administration. Eye 1999; 13: 555–558.
Donnenfeld D, Perry HD, Snyder RW, Moadel R, Elsky M, Jones H et al. Intracorneal, aqueous humor, and vitreous humor penetration of topical and oral ofloxacin. Arch Ophthalmol 1997; 115: 173–176.
Fiscella RG, Nguyen TKP, Cwik MJ, Phillpotts BA, Friedlander SM, Alter DC et al. Aqueous and vitreous penetration of levofloxacin after oral administration. Ophthalmology 1999; 106: 2286–2290.
Garcia-Saenz MC, Arias-Puente A, Fresnadillo-Martinez MJ, Carrasco-Font C . Human aqueous humor levels of oral ciprofloxacin, levofloxacin, and moxifloxacin. J Cataract Refract Surg 2001; 27: 1969–1974.
Hariprasad SM, Mieler WF, Holz ER . Vitreous and aqueous penetration of orally administered gatifloxacin in humans. Arch Ophthalmol 2003; 121: 345–350.
Hariprasad SM, Blinder KJ, Shah GK, Apte RS, Rosenblatt B, Holekamp NM et al. Penetration pharmacokinetics of topically administered 0.5% moxifloxacin ophthalmic solution in human aqueous and vitreous. Arch Ophthalmol 2005; 123: 39–44.
Bauernfeind A . Comparison of the antibacterial activities of the quinolones Bay 12-8039, gatifloxacin (AM 1155), trovafloxacin, clinafloxacin, levofloxacin, and ciprofloxacin. J Antimicrob Chemother 1997; 40: 639–651.
Mather R, Karanchak LM, Romanowski EG, Kowalski RP . Fourth generation fluoroquinolones: new weapons in the arsenal of ophthalmic antibiotics. Am J Ophthalmol 2002; 133: 463–466.
Wise R . A review of the clinical pharmacology of moxifloxacin, a new 8-methoxyquinolone and its potential relation to therapeutic efficacy. Clin Drug Invest 1999; 17: 365–387.
Kowalski RP, Dhaliwal DK, Karenchak LM, Romanowski EG, Mah FS, Ritterband DC et al. Gatifloxacin and moxifloxacin: an in vitro susceptibility comparison to levofloxacin, ciprofloxacin, and ofloxacin using bacterial keratitis isolates. Am J Ophthalmol 2003; 136: 500–505.
Blondeau JM . A review of the comparative in-vitro activities of 12 antimicrobial agents, with a focus on five new ‘respiratory quinolones. J Antimicrob Chemother 1999; 43 (suppl B): 1–11.
Keating GM, Scott LJ . Moxifloxacin: a review of its use in the management of bacterial infections. Drugs 2004; 64: 2347–2377.
Talwar D, Kulkarni A, Azad R, Gupta SK, Velpandian T, Sharma Y et al. Intraocular ciprofloxacin levels after oral administration in silicone oil-filled eyes. Invest Ophthalmol Vis Sci 2003; 44: 505–509.
Goldstein MH, Kowalski RP, Gordon YJ . Emerging fluoroquinolone resistance in bacterial keratitis. Ophthalmology 1999; 106: 1313–1318.
Hariprasad SM, Mieler WE, Shah GK, Blinder KJ, Apte RS, Holekamp NM et al. Human intraocular penetration pharmacokinetics of moxifloxacin 0.5% via topical and collagen shield routes of administration. Trans Am Ophthalmol Soc 2004; 102: 149–155 discussion 155–157.
Liu W, Liu QF, Perkins R, Drusano G, Louie A, Madu A et al. Pharmacokinetics of sparfloxacin in the serum and vitreous humor of rabbits: physicochemical properties that regulate penetration of quinolone antimicrobials. Antimicrob Agents Chemother 1998; 42: 1417–1423.
Acknowledgements
We acknowledge the support of Aravind Medical Research Foundation for the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors do not have proprietary interest in any of the materials or methods used in this study
Rights and permissions
About this article
Cite this article
Vedantham, V., Lalitha, P., Velpandian, T. et al. Vitreous and aqueous penetration of orally administered moxifloxacin in humans. Eye 20, 1273–1278 (2006). https://doi.org/10.1038/sj.eye.6702094
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702094
Keywords
This article is cited by
-
Literature- and Experience-Based Consensus for Acute Post-operative Endophthalmitis and Endogenous Endophthalmitis in Taiwan
Ophthalmology and Therapy (2024)
-
In vitro Susceptibilities of Methicillin-Susceptible and Resistant Staphylococci to Traditional Antibiotics Compared to a Novel Fluoroquinolone
Journal of Ophthalmic Inflammation and Infection (2020)
-
Vitreous and aqueous penetration of orally administered moxifloxacin in humans
Eye (2007)
-
Reply to Kampougeris et al
Eye (2007)