Abstract
Aim To investigate and compare the surgical outcomes of limbal autograft and limbal allograft transplantations in patients with corneal burns.
Methods In total, 20 patients (n=22 eyes) with chemical burn and two patients (n=2 eyes) with thermal burn were included in this study. Limbal autograft or limbal allograft transplantation surgery was performed in all patients. HLA-typing was tested before allograft surgeries. Limbal allografting was performed in all eyes using donor tissue from live relatives. Systemic cyclosporine A was administered for immunosuppression.
Results The corneal surface was successfully reconstructed in all eyes (100%) after limbal autografting, two eyes required additional amniotic membrane transplantation and one eye required allografting. The mean follow-up period for limbal autografts was 13.9±7.0 months. Limbal allografting failed to reduce corneal vascularity and opacification in five (55.6%) eyes and was successful only in four (44.4%) eyes (mean follow-up 16.2±11.2 months) (P=0.002). In all, 15 eyes undergoing limbal autografting completed re-epithelialization of the cornea at a mean of 35.6±60.2 days. The mean epithelial healing time in nine eyes undergoing limbal allografting was 13.0±7.3 days (P=0.525). After limbal autografting, functional vision (≥1/10) was attained in 12 (80%) eyes. Only one eye (11.1%) achieved functional vision after limbal allografting (P=0.036). Penetrating keratoplasty was performed in three patients following limbal allografting. No cyclosporine-associated side effects were observed.
Conclusions Limbal autograft transplantation is an effective and safe procedure for unilateral corneal burns. It seems that limbal allograft transplantation is better combined with penetrating keratoplasty for a better visual outcome and higher graft survival rate. Systemic immunosuppression seems to be necessary for limbal allografts even in the presence of HLA-matched donor tissues.
Similar content being viewed by others
Introduction
The management of ocular surface disorders, particularly ocular burns, has been a challenging condition for years for the ophthalmologists. Even under favourable circumstances, visual performance is disturbed by ocular surface scarring, vascularization, persistent epithelial defects, and associated dry eye soon after initial injury in most cases of ocular burns. Conventional keratoplasty techniques, keratoprosthesis, or other treatment modalities are often associated with postoperative complications and low success rates in these eyes.1,2,3,4
Recent studies of epithelial healing and limbal stem cell transplantation in ocular surface disorders due to various aetiologies (chemical and thermal burns, Stevens–Johnson syndrome, aniridia, atopic keratoconjunctivitis, limbal tumours, contact-lens wear, etc) have improved our understanding of the ocular surface dysfunction. Since Thoft5 first described epithelial transplantation in 1977, many studies6,7,8,9,10 were published concerning different surgical procedures due to limbal stem cell deficiency, such as limbal transplantation and keratoepithelioplasty.
Limbal autograft transplantation (LTau), a procedure for unilateral ocular surface disorders in which the limbal tissue is obtained from the unaffected eye, was first reported by Kenyon and Tseng in 1989. Limbal allograft transplantation (LTal) has been introduced for bilateral ocular surface disorders in which a heterologous limbal tissue is transferred either from a living, related donor eye or from cadaveric eye. It has been reported that allograft transplantation results in a healthier ocular surface, particularly when the immunosuppression is performed even if the donor tissue is human leucocyte antigen (HLA) matched to the recipient. Compared to LTal, limbal autografts are believed to have a higher survival rate as there is no risk of graft rejection. Promising results of these two surgeries have led the ophthalmologists to use these treatment methods in many types of ocular surface disorders in the recent years.11,12,13
Both LTau and LTal are now proven to be successful for stabilizing ocular surface in patients with chemical and thermal burns. Comparisons of outcomes for ocular surface disorders due to various aetiologies and for the acute and chronic phases of corneal burns have been reported previously for limbal autografts and allografts separately.8,9,11,12,13,14,15,16,17 In this study, besides investigating the surgical outcomes of LTau and LTal surgeries, we also aimed to compare the results of these two surgeries in patients with chemical and thermal burns.
Methods
In all, 15 patients (n=15 eyes) who underwent LTau and seven patients (n=9 eyes) who underwent LTal for corneal surface problems caused by chemical and thermal injuries, were included in this study. In the LTau group, there were 11 eyes with alkali burn, three eyes with acid burn and one eye with thermal burn, and the LTal group included eight eyes with alkali burn and one eye with acid burn. Two patients in the LTal group underwent surgeries for both eyes.
After explaining the details of the procedure, informed consent was obtained from all patients and donors before surgery. A brief medical record concerning information about age, gender, underlying ocular pathology, duration of disease, previous medical, or surgical treatments was obtained from all participants. The ophthalmologic examination included evaluation of visual acuity, biomicroscopy of the anterior segment, measurement of intraocular pressure, and fundoscopic examination. Preoperative patient details are listed in Tables 1 and 2. Donor eyes were also evaluated for evidence of stem cell injury before surgery. HLA-matching (Class-1) was performed in all allograft surgeries using a standard serological method and up to a maximum of two mismatches was accepted as an adequate degree of matching.
The surgical indications in all patients were determined by assessing the degree of vascularization with corneal opacity (VCO), conjunctivalization, or epithelial status of the cornea. Patients with bilateral ocular surface damage underwent limbal allografting and those who had a healthy contralateral eye underwent limbal autografting. All surgical procedures were decided and performed by the same surgeon (ÖÖ) in this study.
Surgery was performed under general anaesthesia in one patient. The rest of the patients’ and the donors’ surgeries were performed under local anaesthesia. Surgical details in both limbal grafting and amniotic membrane transplantation procedures were similar to those described in previous reports.11,12,13,14,15,16,18,19
After surgery, the recipient eye was treated with ofloxacin eyedrops one drop every 3 h, dexamethasone eyedrops one drop every 3 h, artificial eyedrops one drop every 2 h, and chloramphenicol ointment at bedtime. Topical steroids were tapered after 3 months and discontinued after 12 months, topical antibiotics were discontinued after 2 months. Systemic cyclosporine A (Cyc A) was administered (5 mg/kg) for immunosuppression in all allograft patients, starting 3 days before the surgery. It was tapered to 2 mg/kg for a period varying from 3 to 5 months and discontinued according to the corneal surface stability.
Results
LTau was performed in 15 eyes of 15 patients using limbal tissue from the contralateral healthy eye. Of these patients, 14 were male and one was female, with a mean age of 28.0±12.0 years (range, 3–50 years). The underlying cause was chemical burn in 14 eyes (11 alkali, three acid) and thermal injury in one eye. The mean follow-up period was 13.9±7.0 months, while the median follow-up was 15.0 months.
LTal was performed in nine eyes of seven patients. All patients were male in this group with a mean age of 43.1±13.3 years (range, 30–71 years). Limbal allografting was performed in both eyes in two patients (cases 5 and 6). The mean follow-up period was found to be 16.2±11.2 months, while the median follow-up was 16.0 months. The patients received limbal tissue from related HLA-matched donors. None of the donor eyes revealed changes in visual acuity or ocular surface after surgery. HLAs were matched in all procedures.
The mean duration of injury before presentation was 65.7±89.2 months (range, 0.5–276 months) for limbal autografts and 173.7±134.9 months (range, 12–396 months) for limbal allografts (Mann–Whitney U, P=0.018). Four patients in the limbal autograft group had undergone surgeries in the affected eye before admission. These were penetrating keratoplasty in three eyes and limbal peritomy in one eye. The limbal allograft group contained five patients who had past ocular surgeries including penetrating keratoplasty in three cases, peritomy in one case and LTal in two cases, which had been performed in various centres.
A total of 15 limbal autograft surgeries were performed in 15 eyes. One patient (case 7) also underwent limbal allograft surgery for the affected eye in this group for the renewal of ocular surface problem. Amniotic membrane transplantation (AMT) was performed in two eyes for the refractory persistent epithelial defect (PED) despite LTau (cases 7 and 13). In total, 12 LTal surgeries were performed in nine eyes of seven patients in this study. In three patients (cases 2, 4, and 5), LTal surgery was repeated for the same eye. Three penetrating keratoplasties were performed in two eyes (cases 2, 3, and 6) after LTal in this group. Tables 3 and 4 summarize the postoperative results of LTau and LTal surgeries.
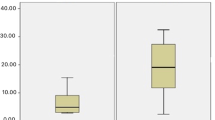
Seven eyes (46.7%) underwent LTau in the acute phase (<4 months) and eight eyes (53.3%) in the chronic phase (>4 months) after chemical or thermal burn. Patients who underwent LTal were all in the chronic phase of chemical or thermal burn (Fisher's exact test, P=0.022). Surgical indications for LTau included corneal vascularization with opacification in seven (46.7%) surgeries and persistent epithelial defect in eight (53.3%) surgeries. All limbal allograft surgeries were performed on patients having corneal vascularization with opacification (Fisher's exact test, P=0.003). Corneal vascularization with opacification persisted in five (55.6%) eyes undergoing limbal allografting and only regressed in four (44.4%) eyes. Corneal vascularization with opacification regressed and persistent epithelial defects healed in all eyes (100%) after limbal autografting (Fisher's exact test, P=0.002) (Figure 1).
Case 2, right eye (Table 1). (a) Alkali burn in acute phase of injury with persistent epithelial defect. (b) Clear corneal surface with minimal opacification after limbal autografting.
In all, 15 eyes undergoing limbal autografting had complete re-epithelialization of the cornea with a mean of 35.6±60.2 days (range, 5–210 days). Epithelial healing delayed in two eyes (cases 7 and 13) after LTau and AMT was performed twice to promote the epithelialization in these eyes. All eyes with limbal allografts achieved complete re-epithelialization of the cornea with a mean of 13.0±7.3 days (range, 6–30 days) (Mann–Whitney U, P=0.525). Re-epithelialization of the cornea in eight eyes undergoing LTau in the chronic phase was completed at a mean of 33.3±71.3 days (range, 5–210) and at a mean of 13.0±7.3 days (range, 6–30 days) in nine eyes undergoing LTal in the chronic phase of injury (Mann–Whitney U, P=0.358). The mean epithelial healing time for the eyes that were operated upon in the acute phase of corneal burn in LTau group was 38.1±50.0 days (range, 9–150 days).
When compared with the eyes in the chronic phase of corneal burn in the LTau group, a statistically significant difference was seen (Mann–Whitney U, P=0.031).
Limbal donor tissues were placed in only one quadrant in three LTau surgeries (one inferior, one nasal, and one temporal) and in two quadrants in 12 LTau surgeries (nine inferior–superior and three nasal—temporal). There were six LTal surgeries with single limbal graft (two inferior, one superior, one nasal, and two temporal) and six LTal surgeries with double limbal grafts (six inferior–superior). Nine simultaneous superior and inferior limbal autograftings and six simultaneous superior and inferior limbal allograftings were performed for corneal surface reconstruction in each groups. The mean epithelial healing time in eyes with limbal superior and inferior autografts was 53.2±73.9 days (range, 6–210 days) and was 10.6±2.8 days (range, 7–14 days) with limbal superior and inferior allografts (Mann–Whitney U, P=0.099).
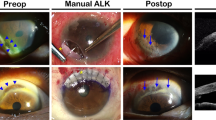
After limbal autografting, functional vision (≥1/10) was achieved in 12 (80%) eyes. Visual improvement ranged from 1/10 to 8/10 in these eyes. Among nine eyes undergoing limbal allografting, functional visual success was achieved in only one eye (11.1%) (Fisher's exact test, P=0.036). Additional penetrating keratoplasties resulted in functional visual improvement in two eyes also from this group after LTal (cases 3 and 6) (Figure 2). Visual acuity after LTau was ≥1/10 in six (75%) eyes operated upon in the chronic phase of corneal burn. Only one (11.1%) eye undergoing LTal in the chronic phase of corneal burn achieved a similar (<1/10) postoperative visual improvement (Fisher's exact test, P=0.046).
Case 6, right eye (Table 2). (a) Alkali burn in chronic phase of injury with corneal vascularization and opacification. (b) Corneal surface cleared significantly after limbal allografting. (c) Additional penetrating keratoplasty improved the vision.
Systemic Cyc A was administered in all patients for a period of 5–12 months after LTals. In case 2, systemic corticosteroid had been started after first limbal allografting to prevent graft rejection, but the ocular surface did not recover after surgery. Therefore, a second LTal was performed and systemic Cyc A was given for immunosuppression. Visual acuity was 1/10 after 2 months and the ocular surface was stable. However, unfortunately, penetrating keratoplasty failed in this eye because of graft abscess, which developed 6 months after surgery. In case 5, the ocular surface problem reoccurred following discontinuation of Cyc A at 6 months, therefore a second LTal surgery was performed on this eye. No Cyc A-associated side effect was observed during immunosuppression.
Discussion
Corneal burns are well-known causes of ocular surface disorders. It has always been very difficult to improve visual performance and ocular discomfort in these eyes. Patients with chemically damaged limbal tissue may experience persistent epithelial defects, corneal vascularization and opacification, conjunctivalization, and even perforation. All of these lead to decreased vision and ocular discomfort as well as poor prognosis for future keratoplasty. Following the introduction of limbal transplantation, especially in the last 10 years, ophthalmologists have treated many cases of corneal burns successfully by means of this new and promising therapeutic approach.
LTau from the fellow eye and LTal from a heterologous donor have been shown to be effective and safe methods of treatment for corneal surface reconstruction because of various aetiologies. The disadvantages of limbal allografting are the risk of graft rejection and side effects of systemic immunosuppression against limbal autografting.
In this study, limbal transplantation surgery was performed for corneal burns in a total of 22 patients (24 eyes). Of these eyes, 15 underwent limbal autografting and nine eyes underwent limbal allografting. Limbal autografting was performed in seven eyes in the acute phase (<4 months) and nine eyes in the chronic phase (>4 months) of corneal burns. Kenyon and Tserg11 and Tsai et al19 have performed LTau as early as 2–4 weeks after chemical corneal burns. Some authors9,16,17 suggest waiting until the ocular inflammation subsides for a better graft survival. We had four eyes that were operated upon 4 weeks after injury, and all these eyes were deprived of most of the corneal epithelium owing to chemical burns. However, they all attained excellent visual outcomes and ocular surface stability after limbal autografting. We suggest that, in the presence of large epithelial defects and small areas of limbal ischaemia, early limbal grafting may be beneficial for preventing vascularization and conjunctivalization of the cornea.
Persistent epithelial defect was the surgical indication in all patients (100%) who underwent limbal autografting in the acute phase of corneal burns. Rao et al9 reported that in the presence of PED, visual function may be worsened after limbal autografting as a result of delayed epithelial healing. Seven of the eyes (87.5%) with PED achieved functional vision after limbal autografting in this study. None of the eyes had PED except for case 13 in the chronic phase of injury. Corneal vascularization with opacification also regressed in all patients (100%) with visual improvement after limbal autografting.
Reducing corneal vascularization with limbal allografts was not as easy as in limbal autografts. Corneal vascularization regressed only in four (44.4%) eyes and persisted in five (55.6%) eyes at a mean follow-up of 16.2 (range, 4–34) months after limbal allograftings. Rao et al9 reported survival of 77.8% at a mean follow-up of 17.2 months (range, 3–33 months) and Daya and Ilari14 reported a survival of 80% with a mean follow-up of 26.2 months (range, 17–43 months). Although the follow-up time in the series of Daya and Ilari14 is nearly twice longer than that of Rao et al,9 the final outcome is rather similar; therefore, the follow-up time does not seem to influence the survival rates too much in allografts. However, risk of graft rejection, discontinuation of immunosuppression, advanced stage ocular surface problems particularly as in these eyes, difficulty of finding HLA-matched donors, and availablity of sufficient amount of graft tissue from donor eye, were all reported to worsen the surgical outcomes in these patients. We presume that the failures for limbal allografts in our study mostly occurred because of advanced stage ocular surface destruction.
Despite its morbidity, oral Cyc A has been shown to improve limbal allograft survival by reducing the rejection rate and the accepted regimen is starting with 2–3 mg/kg and tapering to a dose of 1.5 mg/kg by the end of the first year. Moreover, living related limbal allografts have been reported to require less intensive immunosuppression than cadaveric allografts.20 Although all donors were HLA-matched in this report, we gave Cyc A for immunosuppression to prevent graft rejection at a higher dose (initial dose, 5 mg/kg) than the previous reports. In two patients (cases 2 and 5), lack of immunosuppression for a period of time worsened the ocular surface after LTal. No Cyc A-associated side effects were observed during immunosuppression among patients despite close monitoring of the patients. Most of the previous studies have not reported any significant Cyc A-associated side effects in allograft patients. We suggest systemic immunosuppression even if the donor tissue is HLA-matched for a better graft survival and stable corneal surface after a successful LTal.
Re-epithelialization of the cornea in patients who underwent limbal autografting in the acute and chronic phases of chemical and thermal burns was successfully completed in 13 eyes. In two eyes, re-epithelialization was delayed (case 7:150 days and case 13:210 days) and amniotic membrane transplantations were performed to overcome this problem and these two eyes achieved re-epithelialization. Interestingly, case 7 underwent an LTal 1 year after limbal autografting on the same eye and re-epithelialization was achieved at first month after surgery. Including these two cases, a statistically significant difference was found in epithelial healing times between the acute and chronic phases of corneal burns (P=0.031). Rao et al9 reported a two-fold delay in healing times in the chronic phase (8.3 days) of corneal burns when compared to acute phase (15 days). Kenyon and Tseng11 also reported a significant difference in healing times in the acute and chronic phases (P=0.12).
In this study, mean epithelial healing times for limbal autografting may be considered as much longer than previous reports (Tan et al15:<3 weeks), but these results are related to the prolonged epithelial healing times in two patients. The mean epithelial healing time was 13.38±8.50 days when those two cases were excluded.
Re-epithelialization was achieved in all seven patients (nine eyes) who underwent limbal allografting. The mean epithelial healing time (13.0 days) compared favourably with those reported by Rao et al9 (13.4 days) and Tan et al15 (<4 weeks). When epithelial healing times in patients who underwent LTaus and LTals in the chronic phase of corneal burns were compared, no statistical difference was seen between these groups (P=0.358). Tan et al15 reported a similar result for limbal autografting and limbal allografting in their series including ocular surface disorders, but owing to various aetiologies also including corneal burns. Presumably, this is the first study comparing the epithelial healing times of corneal burns, besides other parameters, following LTaus and LTals.
The visual outcomes of limbal autograft surgery in the acute and chronic phases of corneal burns differed from the series of Rao et al.9 Visual acuities improved significantly (≥1/10) in 12 patients after limbal autografting. Among these patients, six (50%) were in the acute phase and six (50%) were in the chronic phase of injury. However, functional vision was not achieved in patients who underwent limbal allografting. Only one patient attained functional vision after limbal allografting and two patients achieved this after successful penetrating keratoplasties.
Preoperative visual acuities in autografts were not much better than were in allografts in this study; all eyes (100%) had a visual acuity of counting fingers or worse in allograft group before surgery, while 13 (86.6 %) eyes had the same degree of visual loss in autograft group. As mentioned before, in limbal autografts, the presence of PED did not influence the visual outcome and all of these patients gained good functional vision. Patients with corneal opacification and vascularization responded to limbal autografting with better final visual acuities than limbal allografting. Long-standing or bilateral ocular surface dysfunctions could be thought to decrease the success rate in both groups; because even after limbal autografting, long-standing ocular surface problems prevented a good functional vision (cases 1, 4, and 6). Therefore, we may say that limbal autografts seem to be superior to limbal allografting under similar ocular conditions. Maybe the main aim of limbal allografting should be to relieve patients’ symptoms first and thereafter to prepare the corneal surface for a successful future keratoplasty. This was partly achieved in this study. Keratoplasties may still have poor prognosis after limbal allografting because of other ocular surface problems including lid abnormalities, dry eye, etc, as in one of our patients (case 2). These should also be treated properly before performing keratoplasty.
In conclusion, LTau is an effective and safe procedure offering a stable corneal surface and improved visual function for unilateral corneal burns in the intermediate term. Although LTal from HLA-matched donors, in patients with bilateral corneal burns seems to be insufficient alone, combining it with penetrating keratoplasty may result in a better prognosis of graft survival and improved visual function in these eyes. Bilateral and severe corneal burns are still challenging after successful limbal allograftings; owing to such reasons, systemic immunosuppression seems to be mandatory, even in the presence of HLA-matched donor tissues after limbal allograft transplantation.
References
Chiou AG-Y, Florakis GJ, Kazim M . Management of conjunctival cicatrizing diseases and severe ocular surface dysfunction. Surv Ophthalmol 1998; 43: 19–46.
Theng JTS, Tan DT . Combined penetrating keratoplasty and limbal allograft transplantation for severe corneal burns. Ophthalmic Surg Lasers 1997; 28: 765–768.
Mattax JB, McCulley JP . Corneal surgery following alkali burns. Int Ophthalmol Clin 1988; 28: 76–82.
Brodovsky SC, McCarty CA, Snibson G, Loughnan M, Sullivan L, Daniell M et al. Management of alkali burns, a 11-year retrospective review. Ophthalmology 2000; 107: 1829–1835.
Thoft RA . Conjunctival transplantation. Arch Ophthalmol 1977; 95: 1425–1427.
Copeland RA, Char DH . Limbal autograft reconstruction after conjunctival squamous cell carcinoma. Am J Ophthalmol 1990; 110: 412–415.
Jenkins C, Tuft S, Liu C, Buckley R . Limbal transplantation in the management of chronic contact lens-associated epitheliopathy. Eye 1993; 7: 629–633.
Kenyon KR, Rapoza PA . Limbal allograft transplantation for ocular surface disorders. Ophthalmology 1995; 102: 101–102.
Rao SK, Rajagopal R, Sitalakshmi G, Padmanabhan P . Limbal allografting from related living donors for corneal surface reconstruction. Ophthalmology 1999; 106: 822–828.
Tsubato K, Shimazaki J . Surgical treatment of children blinded by Stevens–Johnson syndrome. Am J Ophthalmol 1999; 128: 573–581.
Kenyon KR, Tseng SCG . Limbal autograft transplantation for ocular surface disorders. Ophthalmology 1989; 96: 709–723.
Tsai RJF, Tseng SCG . Human allograft limbal transplantation for corneal surface reconstruction. Cornea 1994; 13: 389–400.
Rao SK, Rajagopal R, Sitalakshmi G, Padmanabhan P . Limbal autografting: comparison of results in the acute and chronic phases of ocular surface burns. Cornea 1999; 18: 164–171.
Daya SM, Ilari L . Living related conjunctival limbal allograft for the treatment of stem cell deficiency. Ophthalmology 2001; 108: 126–134.
Tan DTH, Ficker LA, Buckley RJ . Limbal transplantation. Ophthalmology 1996; 103: 29–36.
Ronk JF, Ruiz-Esmenjaud S, Osorio M, Bacigalupi M, Goosey JD . Limbal conjunctival autograft in a subacute alkaline corneal burn. Cornea 1994; 13: 465–468.
Morgan S, Murray A . Limbal autotransplantation in the acute and chronic phases of severe chemical injuries. Eye 1996; 10: 349–354.
Tseng SCG, Parabhasawat P, Lee SH . Amniotic membrane transplantation for conjunctival surface reconstruction. Am J Ophthalmol 1997; 124: 765–774.
Tsai RFJ, Sun TT, Tseng SCG . Comparison of limbal and conjunctival autograft transplantation in corneal surface reconstruction in rabbits. Ophthalmology 1990; 97: 446–455.
Daya SM, Dugald Bell RW, Habib NE, Powell-Richards A, Dua HS . Clinical and pathological findings in human keratolimbal allograft rejection. Cornea 2000; 19: 443–450.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interest/research funding: None
Rights and permissions
About this article
Cite this article
Özdemir, Ö., Tekeli, O., Örnek, K. et al. Limbal autograft and allograft transplantations in patients with corneal burns. Eye 18, 241–248 (2004). https://doi.org/10.1038/sj.eye.6700640
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700640
Keywords
This article is cited by
-
Ocular Surface Preparation Before Keratoprosthesis Implantation
Ophthalmology and Therapy (2022)
-
Therapeutic Strategies for Corneal Wound Angiogenesis
Current Pathobiology Reports (2020)
-
Oral Mucosal Epithelial Cells Grown on Porous Silicon Membrane for Transfer to the Rat Eye
Scientific Reports (2017)
-
Verätzungen und Verbrennungen des Auges
Der Ophthalmologe (2011)
-
Management of severe ocular burns with symblepharon
Graefe's Archive for Clinical and Experimental Ophthalmology (2009)